Research Article Open Access
Communication Skills Training Significantly Improves Lung Cancer Patient`s Understanding
Wiebke Nehls1*, Sabine Gabrijel1, Alexander Kiss2, Sandra Delis1, Nina-Barbara Black1, Jens Kollmeier1, Andrea Koch3 and Torsten Bauer1
1Clinic for Pneumology, Lungenklinik Heckeshorn, HELIOS Klinikum Emil von Behring, Berlin, Germany
2Division of Psychosomatic Medicine, University Hospital, Basel, Switzerland
3Department of Pneumology, Allergology, Sleep- and Ventilation Medicine, Berufsgenossenschaftliches Uniklinikum Bochum-Bergmannsheil, Bochum, Germany
- *Corresponding Author:
- Wiebke Nehls
Klinik für Pneumologie, Lungenklinik Heckeshorn
HELIOS Klinikum Emil von Behring
Walterhöferstraße 11, 14165 Berlin, Germany
Tel: 0049 30 8102-2776
E-mail: wiebke.nehls@gmx.de
Received date: May 21, 2014; Accepted date: August 08, 2014; Published date: August 18, 2014
Citation: Nehls W, Gabrijel S, Kiss A, Delis S, Black NB, et al. (2014) Communication Skills Training Significantly Improves Lung Cancer Patient`s Understanding. J Palliat Care Med 4:182. doi: 10.4172/2165-7386.1000182
Copyright: © 2014 Nehls W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Introduction: We investigated whether a communication skill training (CST) for physicians leads to improved satisfaction of patients with the disclosure procedure about lung cancer and whether the patient´s recall can be improved.
Methods: In an observation study 101 patients, who were disclosed about their lung cancer diagnosis, were questioned about the recall and satisfaction regarding diagnosis, therapy and therapy goal. The contents of the physicians’ structured questionnaire were then matched with the questions posed to patients in interviews regarding recall. A total of 37 physicians from the lung cancer center attended to a structured CST with simulated patients on basis of the SPIKES model. After this intervention, 100 diagnosed patients were interviewed accordingly.
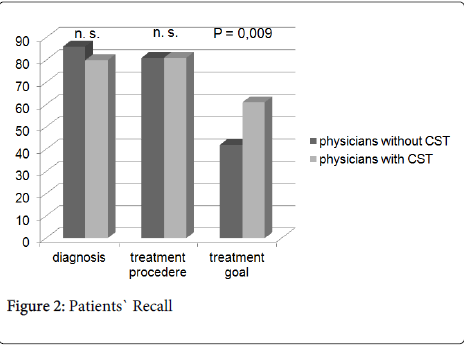
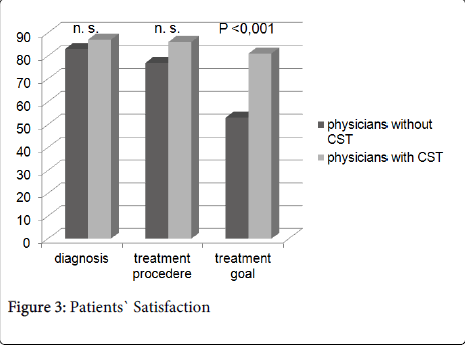
Results: Patients recall of diagnosis and therapy was very high in the observational study (correct recall of diagnosis 86%, correct recall of therapy 81%). The recall results of the physicians trained in communication were comparably high (80% and 82%). The recall of the therapeutic goal respectively, were initially low (42%) and could be raised significantly using the CST (61%; p=0.009). The level of satisfaction with the conversation about diagnosis and therapy was high in both studies. Patients` satisfaction with communication about the treatment goal improved significantly when disclosed by trained physicians (81% versus 53%; p<0.001).
Conclusion: Lung cancer patients do understand the therapeutic goal and their prognosis better, if the disclosing physician took part in a CST. Moreover, patients are more satisfied with the conversation about their prognosis, when trained physicians explain the disease.
Keywords
Lung cancer; Patient-centred communication; Physician` disclosure; Prognosis; Communication skills training
Abbreviations
CST: Communication Skills Training
Introduction
Could it be that a physician communication skills training can improve cancer patients' recall, understanding, and patient satisfaction? When physicians communicate with their patients about a cancer diagnosis there is a tendency to show inadequate perception and lack of competence with the patient’s situation – in terms of a full and effective comprehension of the patient’s ability to cope with the information and impact of the disease [1]. From the patient’s perspective substantial issues are not sufficiently incorporated within the physician’s modus – specifically, the patient’s emotional needs and information about prognosis. This leads to more of a psychological burden, which has the possibility of a two-fold negative result: (a) The psychosomatic impact on the patient could actually make their condition worse than otherwise; (b) The psychological burden might lead the patient to choose a course of treatment that could actually make their condition worse than otherwise [2].
Noticeable is the patient’s inadequate understanding after disclosure of their condition by the physician. Patients know they suffer from cancer and want to be informed about their prognosis [3-6]. However, the goal of treatment and prognosis is often insufficiently understood [7-9], because physicians tend to talk more about medical issues than about the prognosis [10]. The result of this is patients treated with a palliative approach often don’t understand their prognosis and the goal of treatment [9]. When information is withheld there is an adverse effect on patients, relatives and the treatment team [11,12].
Communication Skills Training (CST) for the physician may reduce this problem. The physician has an improved empathetic attitude and the patient copes with his/her emotions better [12-14]. Moreover, CST compels the physician to ask more open questions and pay more attention to the psychosocial aspects of the patient’s experience [15,16]. The SPIKES-Protocol addresses the communication items Setting, Perception, Invitation, Knowledge, Exploration of Emotions, and Strategy and has proven to be useful and effective [10,17].
The results of several randomized studies support the effectiveness of such measures in the form of an objective change of communicative competence [18], see also recent meta-analyzes [14,19] and updated Cochrane Review [20]. However, due to methodological difficulties, there is as yet no sufficient evidence that the corresponding changes in the communicative competence of the physicians also become a patient-side benefits [12,21-23].
The aim of this study was to investigate whether the implementation of a structured CST leads to greater patient satisfaction with the manner and effectiveness of the disclosure of lung cancer. We focus on lung cancer patients, because they have special needs for patient-centered communication, due to their limited prognosis. In other studies, it was noted that they were even worse oriented compare to other cancer patients regarding their prognosis and the treatment goal [9].
Patients and Methods
This (INTERVENTION) study follows a previous (OBSERVATION) study, which served as a historical control. In the previous study 101 lung cancer patients were interviewed regarding how they understood their disease, therapy, treatment goal and prognosis, and how satisfied they felt about the manner of the “messenger” and how effective the communication of the information was [24].
All consecutive patients with a new diagnosis of lung cancer between December 2010 and July 2011 were eligible for the study. The prospective participants were cleared up about the risks and the benefits of the research study. The informed consent process included human subject protections such as risk, confidentiality, etc. in oral and written form. The participants` data were anonymized. Patients who agreed to participate and fulfilling the inclusion criteria (i.e. fluency in German and not critically ill) were approached one to three days after a trained physician had disclosed the diagnosis.
A total of 116 patients met the eligibility criteria. Sixteen had declined. Records were excluded from analyses if patient or physician responses were missing. If the patient was unavailable to meet in person, then the questionnaire was administered by telephone. Complete datasets were available for 100/116 patients (86%). We collected socio-demographic information (age, sex, civil state, children, and employment) and clinical (stage) characteristics of patients. The stage of Lung cancer was in accordance with the seventh edition of the TNM Classification of Malignant Tumours [25].
The Ethical Committee of Berlin Medical University (Charité) approved the study. Informed written consent was obtained from the patient after full disclosure of the study purpose.
Communication Skills Training (CST)
The study was performed in a tertiary lung cancer center with 40 physicians of all educational levels. All physicians of the unit were asked to participate in a CST based on the SPIKES model.
Of 40 physicians, three were unavailable for the training and 37 agreed to participate (93%). A total of 26/40 (63%) disclosed diagnosis, therapy options, and treatment goals after the training. These 26 were approached and agreed to participate in the intervention study. Seven (27%) were pulmonary specialists, and two (8%) were internists, Most of the participants (fifteen, 58%) were residents.
The concept for the communication skills training notes that several strategies already have been proven in other training to be effective at improving communicative skills [12,26-29].
The first part of the intervention was a theoretical introduction to the SPIKES model [17]. This introduction took place at the weekly medical education of the pulmonary unit. All participating physicians were provided with a card for their white coat pocket, containing the six facets of the SPIKES model. Additionally, the physicians’ rooms were equipped with a poster of the six steps of the SPIKES model.
The second part of the intervention was training with professional actors playing patients in four different roles of newly diagnosed lung cancer [30-33]. Selection of physicians who role-played with simulated patients was random [34]. The whole group was instructed in giving feedback. After the role-play, the physician who role-played gave feedback first. Then the simulated patient gave feedback to the physician [35].
There was also an observing group consisting of physicians who are members of the CST team. This group gave feedback regarding specific contents of the SPIKES model. Due to time and logistical constraints not all physicians in the study could actively participate in the role-playing exercise. 61% were able to role-play, whilst 39% were passive observers. Of course, both sets could benefit one from participation, the other from objective observation.
The last part of the intervention involved giving a detailed feedback and video demonstration of examples of role-plays in the weekly medical education of the pulmonary unit. In total the training lasted five hours and was performed by WN and SG.
Measures
In accordance with the observation study patient’s information-recall and satisfaction with communication were recorded by means of a structured interview [24]. Two interviewers (WN, SG) performed all interviews and were blinded to the content of prior physician-patient communication.
Physicians who met with patients were asked to complete a written report of information provided to the patient regarding diagnosis, treatment procedure, and treatment goal. This was to be done within the first 72 hours after the disclosure of diagnosis. The contents of the physicians’ structured questionnaire were carefully matched with the questions posed to patients in interviews regarding recall.
Patient Recall: Regarding Diagnosis, Treatment Procedure and Treatment Goal
Patients were asked the following three questions:
(1) “What did your physician tell you about your diagnosis?”
(2) “What did your physician tell you about the treatment procedure?”
(3) “Did the physician discuss the treatment goal?”
Responses regarding diagnosis were rated fully congruent if patients could say they had lung cancer with or without metastasis, partially congruent if they answered with only a partial description and incongruent if they did not mention cancer.
Answers about the treatment procedure were scored fully congruent if patients described exactly what the treatment procedure was, partially congruent if they had mentioned part of the proposed treatment procedure and incongruent if they answered otherwise.
With respect to treatment goal answers were only rated fully congruent if they could recall whether the primary goal was to cure or palliate the cancer.
Patient Satisfaction with Communication
Satisfaction with communication was assessed by the following questions, proposed by Schofield et al [7]:
(1) “How would you rate the way the diagnosis of cancer was discussed with you?”
(2) “How would you rate the way the treatment procedure for your cancer was discussed with you?”
(3) “How would you rate the way the goal of treatment was discussed with you?”
Patients could score excellent, good, satisfactory, inadequate or poor.
Quality of Life, Depression and Anxiety
During the above mentioned interview patients were also approached with standardized questionnaires regarding quality of life, depression and anxiety. They were given the German version of the validated European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire QLQ-C30 (EORTC QLQ-C30) [36,37]. The EORTC quality of life questionnaire (QLQ) is a system for assessing the health- related quality of life (QoL) of cancer patients. The EORTC QLQ-C30 was field tested in a sample of lung cancer patients in 13 countries to confirm the hypothesised scale structure, to establish reliability and to evaluate validity. It consists of five functional scales (physical, role, cognitive, emotional, and social), three symptom scales (fatigue, pain, and nausea and vomiting), a global health status / QoL scale, and a number of single items assessing additional symptoms commonly reported by cancer patients (dyspnoea, loss of appetite, insomnia, constipation and diarrhoea) and perceived financial impact of the disease.. The Hospital Anxiety and Depression Scale (HADS) is used for measurement of psychometric properties [38]. The HADS is a fourteen item scale, seven of the items relate to anxiety and seven relate to depression.
Statistical Analyses
Satisfaction measures and response options were categorized a priori into two groups: high (excellent/good) and mid-low (satisfactory/inadequate/poor) satisfaction. To characterize the patients in the study sample and to summarize the patient’s ratings of physician communication on each topic in the questionnaire, descriptive statistics were used. Scores and quantitative variables were summarized as means ± standard deviations (SD). For comparisons of categorical variables between groups chi-square tests were appropriate. Continuous variables were compared with student´t-test where appropriate. The level of significance for all tests was set to 0.05, and all analyses were carried out with the Statistical Package for Social Sciences (SPSS 13.0) on a windows operating system.
Results
Descriptives of Patients and Physicians
Patient characteristics are summarized in Table 1. Mean age was 68 ± 10 years. A higher proportion of the sample was male (54%), married (54%), with children (82%) and retired (77%). According to clinical staging, 2%, 17%, 34%, and 47% of patients had stage I, II, III, and IV disease respectively.
| Characteristics | Patients | ||
|---|---|---|---|
| No. | % | ||
| Total No. of patients | 100 | ||
| Age (years) | Mean (± SD) | 68.3 (± 10) | |
| Sex, male | 54 | 54 | |
| Sex, female | 46 | 46 | |
| Civil state | Never married | 4 | 4 |
| Married | 54 | 54 | |
| Widower | 17 | 17 | |
| Divorced | 24 | 24 | |
| Seperated | 1 | 1 | |
| Children | None | 18 | 18 |
| 1 | 32 | 32 | |
| 2 | 33 | 33 | |
| 3 | 12 | 12 | |
| 4 and more | 5 | 5 | |
| Country of birth | Germany | 95 | 95 |
| EU | 2 | 2 | |
| Non-EU | 3 | 3 | |
| Education | Academic | 8 | 8 |
| Employment | Employed | 23 | 23 |
| Stage of disease | I | 2 | 2 |
| II | 17 | 17 | |
| III | 34 | 34 | |
| IV | 47 | 47 | |
| Treatment approach | Curative approach | 38 | 38 |
| Palliative approach | 62 | 62 | |
Table 1: Patients´ Sociodemographic and Disease-Related Characteristics.
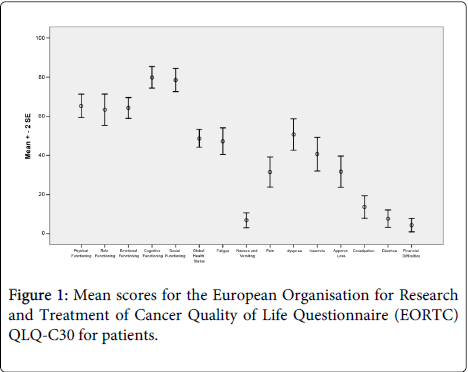
Quality of Life (QoL) is shown in Figure 1. The sample had a high score for the functional scales/high or healthy level of functioning, and a low level of symptomatology/problems compared to the general German population [39]. Only in the fatigue and dyspnea scale they scored slightly higher than in the other symptom scales. The score for the global health status is relatively high and represents a good QOL.
The prevalence of HADS scores, indicative of anxiety disorder and depression, was noteworthy in our study because the figures of 9% (9 of the 100 patients) suffering anxiety disorder and 17% (17 of the 100 patients) with depression is less than the usual percentage in cancer patients [40].
Mean age of physicians was 36 ± 6 years. Fourteen out of 26 (54%) were male. Seven (27%) were fully trained as pulmonary physicians.
Patient Recall
Patient recall is presented in Table 2. Patient recall of information regarding diagnosis was fully congruent in 80 of 100 (80%) patient cases. In 80 of 98 (82%) cases patient recall was fully congruent with information reportedly provided to them about treatment procedure. However, patient recall of the treatment goal was fully congruent in 59 of 97 (61%) patients.
| Physician`s Information | Congruence of Patient and Physician | Patient Satisfaction With Communication | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fully Con-gruent | Partially Con-gruent | In-congruent | High | Mid to Low | ||||||||
| Ntotal* | No. | % | No. | % | No. | % | No. | No. | % | No. | % | |
| Diagnosis | 100 | 80 | 80 | 15 | 15 | 5 | 5 | 99 | 86 | 87 | 13 | 13 |
| Treatment Procedure | 98 | 80 | 81,6 | 1 | 1 | 17 | 17,3 | 91 | 78 | 86 | 13 | 14 |
| Treatment Goal | 97 | 59 | 60,8 | - | - | 38 | 39,2 | 78 | 63 | 81 | 15 | 19 |
| Curative | 37 | 17 | 45,9 | - | - | 20 | 54,1 | 29 | 24 | 83 | 5 | 17 |
| Palliative | 60 | 42 | 70 | - | - | 18 | 30 | 49 | 39 | 80 | 10 | 20 |
Table 2: Congruence Between Physicians`Information and Patients`Recall Regarding Diagnosis, the Treatment Procedure, and the Goal of Treatment and Patient Satisfaction With Communication About Diagnosis, Treatment Procedures, and Goal of Treatment.
Among 37 patients informed that the therapeutic approach was to be curative, seventeen patients (46%) recalled this information fully, compared with 42 of 60 (70%) patients in the palliative care group.
Patient Satisfaction
Patients’ satisfaction with communication is presented in Table 2. Most patients were highly satisfied with communication of diagnosis (87%), treatment procedure (86%) and of the treatment goal (81%). There was negligible difference between patients dealing with a curative goal (83%) versus a palliative goal (80%) regarding satisfaction with communication of the treatment goal.
Patient Recall of Information and Satisfaction With Communication About the Treatment Goal and Prognosis with respect to Patient and Physician Factors.
Patients who were accompanied at the time of disclosure of diagnosis recalled information about the treatment goal significantly better than patients who were alone (p = 0.028). The results are shown in Table 3.
| Patients´ Recall of Treatment Goal and Prognosis | Patients’ Satisfaction With Communication of the Treatment Goal and Prognosis | |||||
|---|---|---|---|---|---|---|
| Correct Recall | Incorrec t Recall | p-value | Satisfied | Not Satisfie d | p-value | |
| Physician Factor, n (%) | ||||||
| Age (>34.5 years), in 54 of 97 cases (57%) | 33/54 (61%) | 21/54 (39%) | p = 0,948 | 38/45 (84%) | 7/45 (16%) | p = 0,336 |
| Sex (male), 43/97 (44%) | 28/43 (65%) | 15/43 (35%) | p = 0,440 | 29/37 (78%) | 8/37 (22%) | p = 0,611 |
| Patient Factor, n (%) | ||||||
| Sex (male), 52/97 (54%) | 31/52 (60%) | 21/52 (40%) | p = 0,793 | 34/43 (79%) | 9/43 (21%) | p = 0,673 |
| Married, 54/97 (56%) | 31/54 (57%) | 23/54 (43%) | p = 0,440 | 35/43 (81%) | 8/43 (19%) | p = 0,876 |
| Children (Yes), 78/96 (81%) | 47/78 (60%) | 31/78 (40%) | p = 0.947 | 48/60 (80%) | 12/60 (20%) | p = 0,876 |
| German, 92/97 (95%) | 57/92 (62%) | 35/92 (38%) | p = 0.327 | 59/73 (81%) | 14/73 (19%) | p = 0,964 |
| Academic, 8/97 (8%) | 5/8 (63%) | 3/8 (37%) | p = 0.919 | 6/8 (75%) | 2/8 (25%) | p = 0,662 |
| Employed, 23/97 (24%) | 10/23 (43.5%) | 13/23 (56.5%) | p = 0.051 | 15/16 (94%) | 1/16 (6%) | p = 0,139 |
| Stage (IIIb, IV), 62/97 (64%) | 37/62 (60%) | 25/62 (40%) | p = 0,758 | 40/53 (75.5%) | 13/53 (24.5%) | p = 0,084 |
| Accompani ed, 64/97 (66%) | 44/64 (69%) | 20/64 (31%) | p = 0.026 | 48/55 (87%) | 7/55 (13%) | p = 0,024 |
| GHS (>50), 35/92 (38%) | 21/35 (60%) | 14/35 (40%) | p = 0,636 | 22/28 (79%) | 6/28 (21%) | p = 0,667 |
| Depressive, 16/93 (17%) | 10/16 (62.5%) | 6/16 (37.5%) | p = 0,837 | 12/13 (92%) | 1/13 (8%) | p = 0,273 |
| DMP congruent, 34/97 (35%) | 19/34 (56%) | 15/34 (44%) | p = 0,464 | 21/27 (78%) | 6/27 (22%) | p = 0,626 |
| Religion (Yes), 52/97 (54%) | 36/52 (69%) | 16/52 (31%) | p = 0,068 | 33/41 (80.5%) | 8/41 (19.5%) | p = 0,947 |
| Living alone, 34/97 (35%) | 21/34 (62%) | 13/34 (38%) | p = 0,889 | 22/28 (79%) | 6/28 (21%) | p = 0,712 |
Table 3: Univariate Analyses of Patients’ and Physicians’ Factors Associated With Patients’ Recall of and Satisfaction with the Treatment Goal and Prognosis.
Comparison to the historical control from the observation study
Socio-demographic and disease-related characteristics of the sample in the intervention study are similar to those of the sample in the observation study. Scores of the EORTC QLQ-C30 questionnaires in the intervention study comply with the results of the observation study. Also, the prevalence of HADS scores indicative of anxiety and depression in the intervention study (9% and 17%) are in accordance with the scores of the observation study (8% and 11%) [24].
Recall of diagnosis was not significantly worse in the intervention study (80%) than in the observation study (86%) (p = 0.259). Recall of treatment procedures was similar in both studies. Recall of the treatment goal was significantly better in the intervention study (61%) compared with the observation study (42%) (p = 0.009). The results are shown in Figure 2.
Satisfaction with communication of diagnosis and treatment procedure was comparable (83% versus 87% and 77% versus 86%). However, satisfaction with communication of the treatment goal was significant better when the physicians had undergone CST (81% versus 53%; p < 0.001). The results are summarized in Figure 3.
Discussion
Communication skills training (CST) implemented in the daily routine improved patient’s satisfaction and recall of the treatment goal.
We investigated a characteristic sample of patients with first diagnosis of lung cancer [41]. The sample of the study matched the sample of the observation study regarding socio-demographic characteristics, functional limitations of quality of life and psychosocial distress. Median age and educational status of physicians who disclosed diagnosis in the intervention study are comparable to those in the observation study. In the intervention study, the proportion of patients with stage IV was slightly lower (47% versus 61%).
In the preceding Observation study patients who could understand they had lung cancer and understood they were going to have chemotherapy or radiation did not necessarily differentiate whether the aim of treatment was palliative or curative. However, this difference is crucial for the patient – physician communication in the health care process [24]. Other authors described poorly oriented patients regarding the treatment goal when disclosed by physicians without CST. For example Weeks et al. found only 31% of lung cancer patients knew their chemotherapy was carried out with a palliative approach [9]. After the observation study, we wanted to know, what could lead to a better understanding of lung cancer patients concerning their treatment goal? This deliberation led us to ask: Could it be that a physician communication skills training can improve cancer patients' recall, understanding, and patient satisfaction? The most important result of our actual study is, that the knowledge of the treatment goal and prognosis can be significantly improved when patients are informed about their diagnosis by trained physicians (61% versus 42%). This result meant that in our lung cancer center, a communication skills training has been implemented as a mandatory continuing education for residents.
In the intervention study patients were significantly more satisfied with information about the treatment goal and prognosis compared to the observation study with untrained physicians. This was true, even if prognosis was limited and the goal of treatment was palliative. In contrast to this result other studies about physician’s communication without training refer to less satisfied patients with information about the treatment goal and prognosis [7-9]. The above mentioned study by Weeks et al concludes that a better understanding of a palliative situation may by nature impact on satisfaction, leading to less satisfied patients [9].
The results concerning the knowledge of diagnosis and treatment and the satisfaction of the conversation about diagnosis and treatment could not be increased comparing the observation study with the intervention study. An improvement was not to be expected here, because in the observation study already a very high level has been reached.
No other study with a comparable sample of lung cancer patients has investigated whether a CST has a positive impact on the patient’s knowledge of and satisfaction with information about the treatment goal and prognosis, so far. Barth et al. showed in a metaanalysis about CST, that patients may benefit from specifically trained health professionals but a comparison to untrained professionals was lacking [14]. The authors of this study can assert that a CST significantly improves the patient’s knowledge of and satisfaction with information about the treatment goal and prognosis.
All clinician-patient interactions desire effective patient recall and understanding as well as satisfaction. Cancer patients are already in the informed consent discussion particularly emotionally charged and - often unspoken - faced with end of life issues. The difficult part of the talks is the change of conversation levels from information to provoked feelings that need to be addressed. Patients with lung cancer often do have a limited life expectation of months, therefore they must know their prognosis and they need to get the opportunity to talk about end-of-life issues. This is the most important substrate for an autonomous decision for all further diagnostic and therapeutic interventions [42]. During disclosing lung cancer diagnosis physicians focus on therapeutic options and avoid talking about prognosis and end-of-life decisions [43,44]. In CST physicians can learn not to limit on technical medical details but also bring into focus patients needs [7,33]. They can become more sensitive to what the patient really needs in terms of appropriate and most useful information. This need for those information is usually underestimated by physicians [45].
Patients who were accompanied for the disclosure of diagnosis knew significantly more about their disease and were significantly more satisfied than patients who were alone. It is well established that an open and early communication with families is an important determinant for how families cope throughout the course of the lung cancer disease. Open and early communication can lead to a decrease in conflicts between patients and their partners [46]. Family conferences have a positive effect on the course of treatment [47,48]. It can be that patients in the intervention study who were accompanied during the disclosure of diagnosis knew more and were more satisfied because communication within the family was better after mutual disclosure of the lung cancer diagnosis. In a CST physicians become sensitized to the benefits of openly inviting relatives and then allowing and enabling them to participate in the disclosing conversation [14,17].
Limitations of the Study
To avoid influence on the way physicians communicate, physician-patient interaction was not documented at the time (e.g. video taping). Therefore the study had to rely upon retrospective self-reports by patients and physicians. Whereas some other studies did document physician-patient interaction [6,49], we did not video or audio tape in order to keep the situation as little artificial as possible. This may have influenced patient recall and satisfaction. However, the time between the disclosure and the interview was short and thus information was unlikely to be skewed. Nevertheless, what information the physician really provided, or how empathetic and honest the physician was remains unknown.
The design of the study required a historical cohort, because it is impossible to disclose a diagnosis to a patient twice. Therefore the same sample could not have been evaluated in both the intervention study and the observation study. However the cohorts were comparable with regard to socio-demographic characteristics, functional limitations and/or psychosocial distress. Due to the study design it was ensured, that none of the patients participated twice. Second, since we had to plan the studies consecutively it is possible that the physicians in the department may have developed a more conscious attitude towards treatment goal and prognosis during the disclosure of lung cancer. This may have boosted our positive results, but does not hamper our conclusions.
Conclusion
We demonstrated that a CST based on the SPIKES-protocol, with professional actors trained as patients, leads to significantly more adequate knowledge of and higher satisfaction with information about the treatment goal and prognosis of lung cancer.
Because the knowledge of a limited prognosis is a substantial precondition for an autonomous and appropriate treatment decision, we recommend establishing conversation training programs for physicians disclosing life-limiting diseases.
Acknowledgement
We thank all the patient and physician participants for giving their time and energy to this study. We would like to thank Paul Black for reading and correcting our English. This paper is part of the doctorial thesis of WN. This study was supported by an unrestricted grant by the Oskar-Helene-Heim foundation, Berlin, Germany.
References
- Fujimori M, Uchitomi Y (2009) Preferences of cancer patients regarding communication of bad news: a systematic literature review. See comment in PubMed Commons below Jpn J ClinOncol 39: 201-216.
- Nelson JE, Gay EB, Berman AR, Powell CA, Salazar-Schicchi J, et al. (2011) Patients rate physician communication about lung cancer. See comment in PubMed Commons below Cancer 117: 5212-5220.
- Clayton JM, Butow PN, Tattersall MH (2005) When and how to initiate discussion about prognosis and end-of-life issues with terminally ill patients. See comment in PubMed Commons below J Pain Symptom Manage 30: 132-144.
- Butow PN, Dowsett S, Hagerty R, Tattersall MH (2002) Communicating prognosis to patients with metastatic disease: what do they really want to know? See comment in PubMed Commons below Support Care Cancer 10: 161-168.
- Hagerty RG, Butow PN, Ellis PM, Dimitry S, Tattersall MH (2005) Communicating prognosis in cancer care: a systematic review of the literature. See comment in PubMed Commons below Ann Oncol 16: 1005-1053.
- Gattellari M, Voigt KJ, Butow PN, Tattersall MH(2002) When the treatment goal is not cure: are cancer patients equipped to make informed decisions? Journal of clinical oncology: official journal of the American Society of Clinical Oncology 20(2): 503-513
- Schofield PE, Butow PN, Thompson JF, Tattersall MH, Beeney LJ, et al. (2003) Psychological responses of patients receiving a diagnosis of cancer. See comment in PubMed Commons below Ann Oncol 14: 48-56.
- Gabrijel S, Grize L, Helfenstein E, Brutsche M, Grossman P, et al. (2008) Receiving the diagnosis of lung cancer: patient recall of information and satisfaction with physician communication. See comment in PubMed Commons below J ClinOncol 26: 297-302.
- Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, et al. (2012) Patients' expectations about effects of chemotherapy for advanced cancer. See comment in PubMed Commons below N Engl J Med 367: 1616-1625.
- McCluskey L, Casarett D, Siderowf A (2004) Breaking the news: a survey of ALS patients and their caregivers. See comment in PubMed Commons below Amyotroph Lateral Scler Other Motor Neuron Disord 5: 131-135.
- Fallowfield LJ, Jenkins VA, Beveridge HA (2002) Truth may hurt but deceit hurts more: communication in palliative care. See comment in PubMed Commons below Palliat Med 16: 297-303.
- Baile WF, Aaron J (2005) Patient-physician communication in oncology: past, present, and future. See comment in PubMed Commons below CurrOpinOncol 17: 331-335.
- Davies P (2001) Delivering bad news. Communication skills must be part of medical education in all specialties. See comment in PubMed Commons below BMJ 322: 865.
- Barth J, Lannen P (2011) Efficacy of communication skills training courses in oncology: a systematic review and meta-analysis. See comment in PubMed Commons below Ann Oncol 22: 1030-1040.
- Delvaux N, Merckaert I, Marchal S, Libert Y, Conradt S, et al. (2005) Physicians' communication with a cancer patient and a relative: a randomized study assessing the efficacy of consolidation workshops. See comment in PubMed Commons below Cancer 103: 2397-2411.
- Fallowfield L, Jenkins V, Farewell V, Solis-Trapala I (2003) Enduring impact of communication skills training: results of a 12-month follow-up. See comment in PubMed Commons below Br J Cancer 89: 1445-1449.
- Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, et al. (2000) SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer. See comment in PubMed Commons below Oncologist 5: 302-311.
- Rabow MW, Dibble SL, Pantilat SZ, McPhee SJ (2004) The comprehensive care team: a controlled trial of outpatient palliative medicine consultation. See comment in PubMed Commons below Arch Intern Med 164: 83-91.
- Uitterhoeve RJ, Bensing JM, Grol RP, Demulder PH, VAN Achterberg T (2010) The effect of communication skills training on patient outcomes in cancer care: a systematic review of the literature. See comment in PubMed Commons below Eur J Cancer Care (Engl) 19: 442-457.
- Moore PM, Rivera Mercado S, GrezArtigues M, Lawrie TA (2013) Communication skills training for healthcare professionals working with people who have cancer. See comment in PubMed Commons below Cochrane Database Syst Rev 3: CD003751.
- Epstein RM (2006) Making communication research matter: what do patients notice, what do patients want, and what do patients need? See comment in PubMed Commons below Patient EducCouns 60: 272-278.
- Salmon P, Mendick N, Young B (2011) Integrative qualitative communication analysis of consultation and patient and practitioner perspectives: towards a theory of authentic caring in clinical relationships. See comment in PubMed Commons below Patient EducCouns 82: 448-454.
- Salmon P, Young B (2005) Core assumptions and research opportunities in clinical communication. See comment in PubMed Commons below Patient EducCouns 58: 225-234.
- Nehls W, Gabrijel S, Kiss A, Kollmeier J, Schmalz O, et al. (2013) Physician communication in a lung cancer center--does the message come across? See comment in PubMed Commons below Pneumologie 67: 688-693.
- Sobin LH, Gospodarowicz MK, Wittekind C(2009) International Union Against Cancer: TNM Classification of Malignant Tumours (7thedn), Wiley-Blackwell, West Sussex, United Kingdom.
- Hobgood C(2005) Delivering the News with Compassion The GRIEV_ING© Death Notification Protocol - Trainer’s Manual. A project supported by Grant No. 2005-VF-GX-K021 awarded by the Office for Victims of Crime office of Justice Programs, U.S. Department of Justice.
- Delvaux N, Razavi D, Marchal S, Brédart A, Farvacques C, et al. (2004) Effects of a 105 hours psychological training program on attitudes, communication skills and occupational stress in oncology: a randomised study. See comment in PubMed Commons below Br J Cancer 90: 106-114.
- Gysels M1, Richardson A, Higginson IJ (2005) Communication training for health professionals who care for patients with cancer: a systematic review of training methods. See comment in PubMed Commons below Support Care Cancer 13: 356-366.
- Bonnaud-Antignac A1, Campion L, Pottier P, Supiot S (2010) Videotaped simulated interviews to improve medical students' skills in disclosing a diagnosis of cancer. See comment in PubMed Commons below Psychooncology 19: 975-981.
- Boulet JR, Murray D, Kras J, Woodhouse J, McAllister J, et al. (2003) Reliability and validity of a simulation-based acute care skills assessment for medical students and residents. See comment in PubMed Commons below Anesthesiology 99: 1270-1280.
- Kneebone RL, Scott W, Darzi A, Horrocks M (2004) Simulation and clinical practice: strengthening the relationship. See comment in PubMed Commons below Med Educ 38: 1095-1102.
- Nikendei C, Zipfel S, Roth C, Löwe B, Herzog W, et al. (2003) [Communication and interaction in psychosomatic education: use of standardized patients]. See comment in PubMed Commons below PsychotherPsychosom Med Psychol 53: 440-445.
- Langewitz W, Heydrich L, Nübling M, Szirt L, Weber H, et al. (2010) Swiss Cancer League communication skills training programme for oncology nurses: an evaluation. See comment in PubMed Commons below J AdvNurs 66: 2266-2277.
- Park I, Gupta A, Mandani K, Haubner L, Peckler B (2010) Breaking bad news education for emergency medicine residents: A novel training module using simulation with the SPIKES protocol. See comment in PubMed Commons below J Emerg Trauma Shock 3: 385-388.
- Greco M, Brownlea A, McGovern J (2001) Impact of patient feedback on the interpersonal skills of general practice registrars: results of a longitudinal study. See comment in PubMed Commons below Med Educ 35: 748-756.
- Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, et al. (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. See comment in PubMed Commons below J Natl Cancer Inst 85: 365-376.
- Fayers P, Aaronson N, Bjordal K, Groenvold M, Curran D, Bottomley A. EORTC QLQ-C30 Scoring Manual (ed 4). Brussels, Belgium, EORTC Publications. 2001.
- Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. See comment in PubMed Commons below ActaPsychiatrScand 67: 361-370.
- Schwarz R, Hinz A (2001) Reference data for the quality of life questionnaire EORTC QLQ-C30 in the general German population. See comment in PubMed Commons below Eur J Cancer 37: 1345-1351.
- Keller M, Sommerfeldt S, Fischer C, Knight L, Riesbeck M, et al. (2004) Recognition of distress and psychiatric morbidity in cancer patients: a multi-method approach. See comment in PubMed Commons below Ann Oncol 15: 1243-1249.
- Putila J, Remick SC, Guo NL (2011) Combining clinical, pathological, and demographic factors refines prognosis of lung cancer: a population-based study. See comment in PubMed Commons below PLoS One 6: e17493.
- Norton SA, Bowers BJ (2001) Working toward consensus: providers' strategies to shift patients from curative to palliative treatment choices. See comment in PubMed Commons below Res Nurs Health 24: 258-269.
- Huskamp HA, Keating NL, Malin JL, Zaslavsky AM, Weeks JC, et al. (2009) Discussions with physicians about hospice among patients with metastatic lung cancer. See comment in PubMed Commons below Arch Intern Med 169: 954-962.
- Keating NL, Landrum MB, Rogers SO Jr, Baum SK, Virnig BA, et al. (2010) Physician factors associated with discussions about end-of-life care. See comment in PubMed Commons below Cancer 116: 998-1006.
- Hancock K, Clayton JM, Parker SM, Walder S, Butow PN, et al. (2007) Discrepant perceptions about end-of-life communication: a systematic review. See comment in PubMed Commons below J Pain Symptom Manage 34: 190-200.
- Badr H, Taylor CL (2006) Social constraints and spousal communication in lung cancer. See comment in PubMed Commons below Psychooncology 15: 673-683.
- Hannon B1, O'Reilly V, Bennett K, Breen K, Lawlor PG (2012) Meeting the family: measuring effectiveness of family meetings in a specialist inpatient palliative care unit. See comment in PubMed Commons below Palliat Support Care 10: 43-49.
- Tan NS, Goodman SG, Yan RT, Elbarouni B, Budaj A, et al. (2013) Comparative prognostic value of T-wave inversion and ST-segment depression on the admission electrocardiogram in non-ST-segment elevation acute coronary syndromes. See comment in PubMed Commons below Am Heart J 166: 290-297.
- Butow PN, Brown RF, Cogar S, Tattersall MH, Dunn SM (2002) Oncologists' reactions to cancer patients' verbal cues. See comment in PubMed Commons below Psychooncology 11: 47-58.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 14199
- [From(publication date):
August-2014 - Jan 27, 2025] - Breakdown by view type
- HTML page views : 9805
- PDF downloads : 4394