Commentary: Over-diagnosis and Under-Diagnosis of Alzheimer's Disease
Received: 03-Oct-2018 / Accepted Date: 05-Oct-2018 / Published Date: 12-Oct-2018 DOI: 10.4172/2161-0460.1000449
Keywords: Alzheimer’s disease; Over diagnosis; Under diagnosis
Abbreviations
ACh: acetylcholine; AD: Alzheimer’s disease; BPSD: behavioral and psychological symptoms of dementia; BT: bipolarity; ChAT: choline acetyltransferase; ChEI: cholinesterase inhibitor; MCI: mild cognitive impairment
Commentary
Alzheimer’s disease (AD) is diagnosed by DSM-5 [1] or NINCDSADRDA Work Group [2]. Clinically, this disorder is diagnosed by forgetfulness and disturbances of daily livings. However, we feel there existence at substantial level of over-diagnosis and under-diagnosis of AD. Therefore in this article, we discuss the reasons why over-diagnosis and under diagnosis of AD is occurred.
We consider that over diagnosis of AD is occurred when we misdiagnose the depression or bipolarity [3] (BT). Depression is tended to develop AD [4] and when depression occurs, cognitive dysfunctions also occur, which is same as those of AD (pseudo-dementia) [5,6]. On the elderly persons, not only BT but also aging process cause pseudodemented state. Moreover, this state is also similar with the symptoms of AD. In this state, when we prescribe cholinesterase inhibitors (ChEI), agitation and aggressiveness are occurred sometimes. We emphasize that we should find out BT.
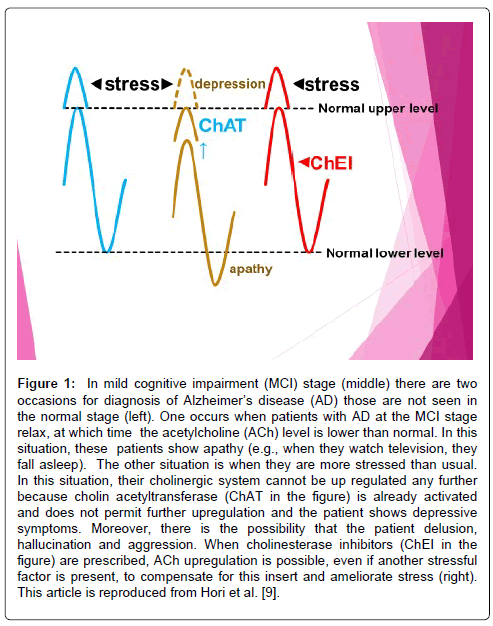
We consider that under diagnosis of AD is occurred when we overlook the apathy. We also feel that the major problem is that many physicians diagnose AD based only on the cognitive functions and diagnostic imaging in clinical setting but not on apathy symptoms founded out in everyday life. As mentioned before, AD pathology causes the degeneration of cholinergic neurons. However, because the compensatory mechanism works, the activity of choline acetyltransferase (ChAT, an enzyme that produces acetylcholine (ACh)) is not down regulated in the mild to moderate stages of AD [7,8]. According to this compensatory mechanism, at mild stage of AD, ChAT activity in AD patients could have been high, which could account for the fact that the ACh level was relatively normal and in ordinal situations, cognitive functions in AD patients were relatively intact. This compensatory reaction to the onset of AD may be attributable to hyperactivity of presynaptic cholinergic neurons. If this compensatory mechanism works, the cholinergic system is intact, rather than deteriorated. However, if this compensatory mechanism continues, continuation of hyperactivity cholinergic neurons causes early degenerations of these neurons because of fatigue. If we can prescribe ChEI, the compensatory mechanism can be mild and prevention of early degeneration of cholinergic neuron is possible. Therefore, we should not overlook this state when we diagnose AD. We speculate that there might be two situations in which ACh might be down regulated or overburdened [9]. We show this in (Figure 1). In mild cognitive impairment (MCI) stage (Figure 1, middle) there are two occasions for diagnosis of AD, those are not seen in the normal stage (Figure 1, left). One occurs when patients with AD at the MCI stage relax, at which time the ACh level is lower than normal. In this situation, these patients show apathy (e.g., when they watch television, they fall asleep). The other situation is when they are more stressed than usual. In this situation, their cholinergic system cannot be up regulated any further because ChAT is already activated and does not permit further upregulation and the patient shows depressive symptoms. Moreover, there is the possibility that the patient faces delusion, hallucination and aggression [10,11]. When ChEIs are prescribed, ACh upregulation is possible, even if another stressful factor is present, to compensate for this insert and ameliorate stress (Figure 1, right). We reported that behavioral and psychological symptoms of dementia (BPSD) is caused by BT or AD pathology [10,11]. In fact, after the patient show these BPSD, the progression of AD is accelerated. Moreover, when the patient complains the subjective memory complains, we should start the treatment for AD [12].
Figure 1: In mild cognitive impairment (MCI) stage (middle) there are two occasions for diagnosis of Alzheimer’s disease (AD) those are not seen in the normal stage (left). One occurs when patients with AD at the MCI stage relax, at which time the acetylcholine (ACh) level is lower than normal. In this situation, these patients show apathy (e.g., when they watch television, they fall asleep). The other situation is when they are more stressed than usual. In this situation, their cholinergic system cannot be up regulated any further because cholin acetyltransferase (ChAT in the figure) is already activated and does not permit further upregulation and the patient shows depressive symptoms. Moreover, there is the possibility that the patient delusion, hallucination and aggression. When cholinesterase inhibitors (ChEI in the figure) are prescribed, ACh upregulation is possible, even if another stressful factor is present, to compensate for this insert and ameliorate stress (right). This article is reproduced from Hori et al. [9].
In order to prevent over-diagnosis and under diagnosis of AD, we should hear their behaviors in everyday life and life history of the patient. Apathy and depression are not always seen in clinical settings. These symptoms are shown in their everyday lives.
Therefore, we consider it is important that we should not misdiagnose depression and not overlook apathy founded out in every life of patients or persons with old age. Alternatively these procedures are painful. Therefore, it is difficult for early diagnosis of elderly subjects with mild cognitive impairment [13]. However, these processes are interesting as for psychiatrist because we can see the lives of patients who live longer lives.
References
- Zelazny K, Simms LJ (2015) Confirmatory factor analyses of DSM-5 posttraumatic stress disorder symptoms in psychiatric samples differing in criterion a status. J Anxiety Disord 34: 15-23.
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, et al. (1984) Clinical diagnosis of Alzheimer's disease: Report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology 34: 939-944.
- Akiskal HS (2007) The emergence of the bipolar spectrum: Vlidation along clinical-epidemiologic and familial-genetic lines. Psychopharmacol Bull 40: 99-115.
- Barbe C, Jolly D, Morrone I, Wolak-Theirry A, Drame M, et al. (2018) Factors associated with quality of life in patients with Alzheimer's disease. BMC Geriatr 18: 159.
- Kang H, Zhao F, You L, Giorgetta C, Venkatesh D, et al. (2014) Pseudo-dementia: A neuropsychological review. Ann Indian Acad Neurol 17: 147-154.
- Tripathi R, Mehrotra S (2015) Pseudo-dementia: A neuropsychological review. Ann Indian Acad Neurol 18: 123-124.
- Gilmor ML, Erickson JD, Varoqui H, Hersh LB, Bennett DA, et al. (1999) Preservation of nucleus basalis neurons containing choline acetyltransferase and the vesicular acetylcholine transporter in the elderly with mild cognitive impairment and early Alzheimer’s disease. J Comp Neurol 411: 693-704.
- De Kosky ST, Ikonomovic MD, Styren SD, Beckett L, Wisniewski S, et al. (2002) Upregulation of choline acetyltransferase activity in hippocampus and frontal cortex of elderly subjects with mild cognitive impairment. Ann Neurol 51: 145-155.
- Hori K, Hosoi M, Konishi K, Sodenaga M, Hashimoto C, et al. (2016) Cholinesterase inhibitors as a disease-modifying therapy for Alzheimer’s disease: The anticholinergic hypothesis. Austin J Clin Neurol 3: 1091.
- Konishi K, Hori K, Oda T, Tominaga I, Asaoka T, et al (2009) Effects of aging on behavioral symptoms in Alzheimer's disease. Psychogeriatrics 9: 11-16.
- Hori K, Konishi K, Tomioka H, Tani M, Minegishi G, et al. (2012) Mood symptoms are related to psychotic symptoms in severe Alzheimer's disease. J Addict Res Ther S5: 002.
- Choe YM, Byun MS, Lee JH, Sohn BK, Lee CDY, et al. (2018) Subjective memory complaint as a useful tool for the early detection of Alzheimer’s disease. Neuropsychiatry Dis Treat 14: 2451-2460.
- Hori K, Hashimoto C, Sasaki O, Tadokoro M, Tsukahara S, et al. (2017) Difficulty for early diagnosis of Alzheimer’s disease: Especially MCI Level. Physiother Rehabil 2: 2.
Citation: Sodenaga M, Hori K, Konishi K, Hashimoto C, Katsumura K, et al. (2018) Commentary: Over-diagnosis and Under-Diagnosis of Alzheimer's Disease. J Alzheimers Dis Parkinsonism 8: 449. DOI: 10.4172/2161-0460.1000449
Copyright: © 2018 Sodenaga M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3563
- [From(publication date): 0-2018 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 2781
- PDF downloads: 782