Color Doppler Ultrasound Evaluation of Optic Nerve Head Arteries in Young Black Africans with Primary Open-angle Glaucoma (POAG)
Received: 13-Aug-2021 / Accepted Date: 27-Aug-2021 / Published Date: 03-Sep-2021 DOI: 10.4172/2167-7964.1000338
Abstract
Background: Primary open-angle glaucoma (POAG) is a common cause of blindness. It is particularly common and severe in the black population, occurring in younger subjects.
Aim: The aim of this study was to investigate color Doppler ultrasound (CDU) characteristics of the arteries of the optic nerve head (ONH) in young black patient with POAG.
Method: a prospective descriptive and analytical study of the measures of the blood flow parameters of the arteries of the ONH by CDU, in a consecutive series of 30 black-Africans glaucomatous patients of both sexes, aged 18 to 45 years diagnosed positive for POAG.
Results: A female predominance with a sex ratio of 0.76 was noted. Intra ocular pressure (IOP) was normal in 60% in the right eye, 66.7% in the left eye, or 63.3% in both eyes. The Arterial peak systolic velocity (PSV) was normal in 53.3%, low (46.7%) for the ophthalmic artery (OA). No cases of increased PSV were recorded. The PSV was accelerated in 98.3% in the central retinal artery (CRA), and normal (33.3%) or accelerated (65%) in the paraoptic short ciliary artery (PCA). The correlation analysis between variations in PSV and IOP does not show a statistically significant relationship (p> 0.05) for the three arteries of the ONH. The resistive index (RI) were elevated in 11.7%, 70% and 45%, respectively in the OA, CRA and PCA. No case of decreased resistance was found for the three arteries. The correlation between RI and IOP also did not show a statistically significant correlation (p> 0.05).
Conclusion: CDU of the arteries of ONH in black origin young glaucomatous patients presents peculiarities. PSVs are low or normal in OA, with RI most often normal, while PSV are high or normal in CRA and PCA and RI high in the majority of cases.
Keywords: Color Doppler ultrasound; primary open-angle glaucoma; black-African.
Introduction
Primary open-angle glaucoma (POAG) is a chronic progressive anterior optic neuropathy characterized by visual field test alterations and pathological excavation of the optic nerve head (ONH) [1].
Glaucoma is the second leading cause of blindness in the United States of America [2]. In Africa, it is the second leading cause of blindness after cataract in rural areas [3]. According to the World Health Organization, more than 100 million people are suspected of glaucoma, more than 20 million suffer from it and more than 5 million are blind because of this condition [4].
The PAOG is called primitive, because there is no identifiable cause, even there are known risk factors, including African ethnicity or the black color of the skin and age. Indeed, it is the leading cause of blindness in American black [2]. Regarding the age, if in the white population PAOG is more common in the elderly, with an average age of 65.6 years in the study of Bresson-Dumont H. et al. [5] and 63.7 years in that of Martinez A. et al. [6]. In black African’s, it predominates in a younger population, around 45 years [7, 8].
The pathophysiology of POAG is not clearly established. Hypo perfusion of the optic nerve, linked to microcirculatory abnormalities is considered to be one of the physiopathological factors. This hemodynamic factor has been cited by several studies as a risk factor and prognosis for POAG [9-14]. Most of the studies available focus on groups of glaucomatous subjects of high average age and Caucasian origin [5, 6]. The objective of this study was to study the color Doppler ultrasound (CDU) characteristics of arterial vascularization in the ONH in young black patients with PAOG.
Method
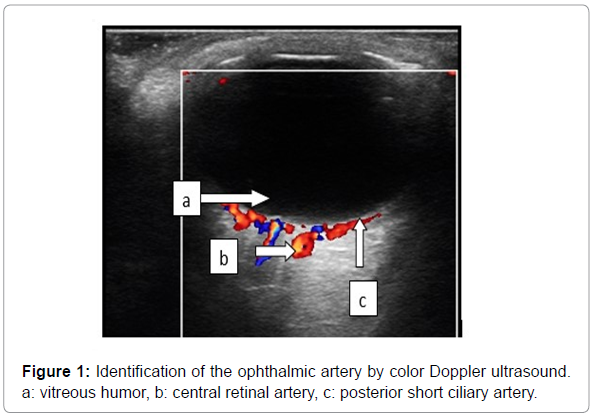
A prospective, descriptive and analytical study was designed to analyze velocity parameters measured by CDU in the arteries of the ONH in glaucomatous patients. The study included in 30 patients aged from 18 to 45 years who were diagnosed positive with PAOG by an ophthalmologist based on ophthalmological arguments. The CDU was performed by the same operator to avoid inter-observer variations, by using the same ultrasound device (MINDRAY CD-60) equipped with a linear probe with Doppler-Color, to avoid the bias related to the machine. The parameters studied included epidemiological data (age and sex, family history of glaucoma), ophthalmic examination data (visual field, intraocular pressure (IOP), tachymetry), the upper extremity blood pressure measurement and the velocity parameters of arterial peak systolic velocity (PSV), end-diastolic velocity (EDV), and resistive index (RI) calculated using the RI= (PSV-EDV)/PSV formula. CDU parameters were recorded bilaterally on the following arteries: the central retinal artery (CRA), ophthalmic artery (OA) and the paraoptic short ciliary artery (PCA). These arteries were identified on CDU using a 10 MHz frequency probe. Mode B was used to highlight the anatomical landmarks of the eye, namely the lens, the vitreous, the posterior edge of the eyeball and the shadow of the optic nerve. After locating the optic nerve, switching on the color Doppler enabled the arteries to be identified and the pulsed Doppler spectrum to be recorded there Figure 1.
Results
General data
The patients included in the study were composed of 43% (13) male and 57% (17) of female, with a sex ratio of 0.76. The mean age of the patients was 30.4 ± 7.6 years. The most represented age group was that of 20 to 25 years (30%) Table 1.
| Age | Number | Percentage |
|---|---|---|
| ≤ 18 | 1 | 3.3 |
| 20-25 | 9 | 30 |
| 26-30 | 5 | 16.7 |
| 31-35 | 8 | 26.7 |
| 36-40 | 3 | 10 |
| 41-45 | 4 | 13.3 |
| Total | 30 | 100 |
Table 1: Distribution of patients by age group.
Clinical and ophthalmological data
IOP was normal in more than half of the cases, with 60% in the right eyes, 66.7% in the left eyes, and 63.3% in both eyes. The values of IOP, central corneal thickness or tachymetry and visual field examination results are summarized in Table 2.
| Intra ocular pressure (IOP) | Right eye n (%) | Left eye n (%) | Total n (%) | |
|---|---|---|---|---|
| Normal | 18(60) | 20(66,7) | 38(63,3) | |
| abnormal (increased) | 12(40) | 10(33,3) | 22(36,7) | |
| Pachymetry (Central corneal thickness) | ||||
| Normal | 19(63,3) | 21(70) | 40(66,7) | |
| Abnormal (thin) | 11(36,7) | 9(30) | 20(33,3) | |
| Visual field test | ||||
| Normal | 10(33,3) | 8(26,7) | 18(30) | |
| Abnormal | 20(66,7) | 22(73,3) | 42(70) | |
Table 2: Results of the ophthalmologic examination.
The blood pressure measurement noted systolic arterial pressure, elevated in 5 patients (16.7%) among whom there were 3 cases of ocular hypertonia (10%). All other cases of IOP elevation were seen in non-hypertensive patients.
The systolic and diastolic perfusion pressure was low in 33.33% of cases (n = 10) and high in 3.33% (n = 1) with a high mean perfusion pressure, measured at 146 mm Hg.
Doppler velocity data
In the Doppler study of the arteries of the ONH, the PSV was normal (53.3%) or low (46.7%) in the OA. No case of acceleration of the PSV was recorded. The PSV was accelerated in almost all cases (98.3%) in the CRA and normal (33.3%) or accelerated (65%) in the PCA (Table 3).
| Ophthalmic artery (OA) | IOP >21 (n = 22) | IOP ≤ 21 (n = 38) | p value | |
|---|---|---|---|---|
| n (%) | n (%) | |||
| High PSV (˃ 58.1) | 0(0) | 0(0) | 0.347 | |
| Normal PSV (23.1- 58.1) | 15(68.2) | 17(44.7) | ||
| Low PSV (< 23.1) | 7(31.8) | 21(55.3) | ||
| Central Retinal Artery (CRA) | 0.887 | |||
| High PSV (˃ 13.4) | 22(100) | 37(97.4) | ||
| Normal PSV (5.8- 13.4) | 0(0) | 1(2.6) | ||
| Low PSV (< 5.8) | 0(0) | 0(0) | ||
| Paraoptic short Ciliary Artery (PCA) | 0.092 | |||
| High PSV (˃ 18.6) | 5(22,7) | 15(39.5) | ||
| Normal PSV (8.1 – 18.6) | 17(77,3) | 22(57.9) | ||
| Low PSV (< 8.1) | 0(0) | 1(2.6) | ||
Table 3: Distribution of peak systolic velocity (PSV) and the IOP.
Correlation analysis between variations in PSV and IOP does not show a statistically significant link for the three ONH arteries studied (p> 0.05).
The calculation of the resistive index generally finds normal or high RIs. No case of decrease of RI was found for the three arteries of the ONH. RIs were elevated in 11.7%, 70% and 45%, respectively, in the OA, CRA and PCA (Table 4).
| Ophthalmic artery (OA) | PIO >21 (n = 22) | PIO ≤ 21 (n = 38) | p value |
|---|---|---|---|
| n (%) | n (%) | ||
| High RI (˃ 0.85) | 4(18.2) | 3(7.9) | 1.371 |
| Normal RI (0.61 – 0.85) | 18(81.8) | 35(92.1) | |
| Low RI (< 0.61) | 0(0) | 0(0) | |
| Central Retinal Artery (CRA) | |||
| High RI (˃ 0.78) | 17(77.3) | 25(65.8) | 0.309 |
| Normal RI (0.48 – 0.78) | 5(22.7) | 13(34.2) | |
| Low RI (< 0.48) | 0(0) | 0(0) | |
| Paraoptic short Ciliary Artery (PCA) | |||
| High RI (˃ 0.73) | 12(54.5) | 15(39.5) | 0.562 |
| Normal RI (0.47 – 0.73) | 10(45.5) | 23(60.5) | |
| Low RI (< 0.47) | 0(0) | 0(0) | |
Table 4: Distribution of Resistive Index (RI) and the IOP.
The correlation between RI and IOP also did not show a statistically significant correlation (p> 0.05).
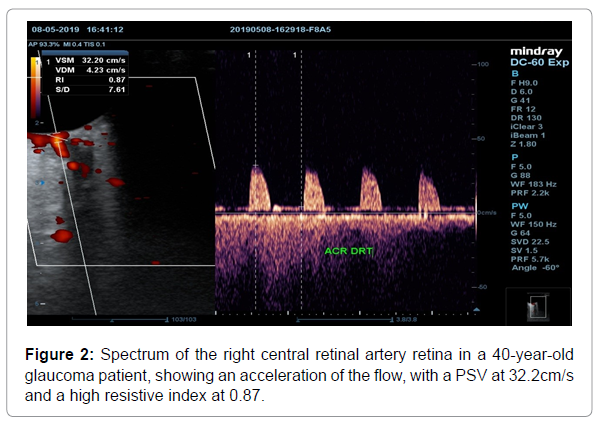
The illustrates on Doppler ultrasound with spectral recording, measurement of velocities and calculation of the RI, of the right CRA of a 40-year-old glaucomatous patient, an acceleration of the PSV and an elevation of the RI (Figure 2).
Discussion
A female predominance with a sex ratio of 0.76 was found in our study. This predominance is not a constant. Indeed if this was also found by Quigley et al. with a frequency of 55% of POAG cases [4]. Atipo-Tsiba PW et al. found in a black population in Congo male predominance [15].
Contrary to expected IOP is more often normal than pathological in POAG. This is a constant already found in other series [16]. Commonly, the tendency is to think that glaucoma is a disease linked to the elevation of IOP. In fact, it has been established for several decades that glaucomatous neuropathies can occur at normal IOPs, located below 21 mmHg [17]. Currently, increased IOP is considered to be a risk factor for glaucoma [18]. It is also a part of monitoring glaucomatous patients, since its elevation is a factor of severity.
Regarding blood pressure, although considered by some to be a risk factor for POAG, its role remains much debated [19-23]. Several studies find a correlation between hypertension and IOP but the relationship between hypertension and glaucoma remains controversial [18]. This correlation may be true in Caucasian populations where glaucoma is observed at ages generally older than our study population [22]. Other studies have introduced the concept of ocular perfusion pressure, involving arterial pressure and IOP, and have shown it decrease in glaucomatous patients [24]. However, in our series, this hemodynamic disturbance was weak, found only in 33.33%.
The PSV in the ophthalmic arteries, were low or normal. No case of elevation above normal values was found. This is the opposite of what was noted in CRAs where only a single value was normal, all PSVs being high. The PCA is at the halfway with the majority of PSVs lying within normal limits. Despite these observations, no statistically significant link was found between PSV and IOP values for each of the three arteries analyzed.
Calculation of RI showed no case of decreased resistance within the arteries of the ONH in young patients with POAG. Differences were noted depending on the arteries. Indeed, RIs were normal in the majority of cases (88.33%) for OA, while they were elevated in 70% in CRA and 50% in PCA.
In general, the results of CDU depend on the target group. Fatima Jimenez -Aragon et al. [25] showed a combination of decreased flow rates and increased resistive indexes in patients with progressing glaucoma compared to those who remain stable, which enabled them to suggest the use of Doppler ultrasound to help set up more aggressive clinical management in conflicting cases with a higher risk of progression.
The peculiarities observed in our series, made of young black Africans, can be considered on the one hand as a specificities of this group, a group which is known as higher at risk of POAG and in whom age recognized as a risk factor for glaucoma due to changes in vascular walls, is not to be taken into account.
The correlation study between RI and IOP reveals, as for PSV, an absence of statistically significant link between the different variables.
Conclusion
The color Doppler ultrasound of the arteries of the optic nerve head in young glaucomatous black African origin patients has special features. PSVs are low or normal in the OA, with RI most often normal, while PSV are high or normal in the CRA and PCA and RI elevated in the majority of cases.
Additional case-control CDU studies in the same population group would make it possible to consolidate the observations, and possibly to study other specific additional parameters, which could be used in the diagnosis, monitoring and prognostic evaluation of patients.
References
- Sellem E (2009) Le glaucome de la clinique au traitement. J Fr Ophtamol 32: 187-220.
- Kwon YH, Fingert JH, Kuehn MH, Alward WL, (2009) Primary open-Angle glaucoma. N Eng J Med 360:1113-1124.
- Balo PK, Wabagira J, Banla M, Kuaovi RK (2000) Specific causes of blindness and vision impairment in a rural area of Southern Togo. J Fr Ophtalmol 23: 459-464.
- Quigley HA, Broman AT, (2020) the number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 90: 262-267.
- Bresson-Dumont H, de Bray JM, Béchetoille A (1999) Echo-Doppler couleur des artères ciliaires courtes para-optiques dans le glaucome vasculaire. J Fr Ophtalmol 22: 743-748.
- MartÃnez J.-P, Kinet J.-M, Bajji M, Lutts S, (2005) NaCl alleviates polyethylene glycolinduced water stress in the halophyte species Atriplex halimus L. J Exp Bot 56: 2421-2431.
- Balo KP, Mihluedo H, Djagnikpo PA, Moukangni A, Bechetoille A (1998) Morphometry of the optic disc in Togolese patients with glaucoma or suspected glaucoma. Preliminary study, J Fr Ophtalmol 21: 328-332.
- Kabuni M, Maertens K (1984) Glaucome chronique simple chez le noir au Zaire. Ann. Scc. Méd. Trop 64:45-50.
- Carter CJ, Brooks DE, Doyle DL, Drance SM, (1990) Investigations into a vascular aetiology for low-tension glaucome. Ophthalmology 97:49-55.
- Flammer J, (1994) the vascular concept of glaucoma. Surv Ophthalmol 38: 3-6.
- Hayreh SS, (1994) Progress in the understanding of the vascular aetiology of glaucoma Curr Opin Ophthalmol 5:26-35.
- Schumann J, Orgul S, Gugleta K, Dubler B, Flammer J (2000) Intraocular difference in progression of glaucoma correlates with intraocular differences in retro bulbar circulation. Am J Ophthalmol 129: 728-733.
- Satilmis M, Orgül S, Doubler B, Flammer J (2003) Rate of progression of glaucoma correlates with retro bulbar circulation and intraocular pressure. Am J Ophthalmol 135: 664-669.
- Galassi F, Sodi A, Ucci F, Renieri G, Pieri B, et al. (2003) Ocular hemodynamics and glaucoma prognosis: a color Doppler imaging study. Arch Ophthalmol 121: 1711-1715.
- Atipo Tsiba PW, Dohvoma VA, Omgbwa Eballe A, Diomandé AI, Ebana, S (2017) Aspects épidémiologiques et cliniques du glaucome au CHU de Brazzaville. Health Sci Dis 18: 70-72.
- Leske MC, Connell AM, Wu SY, Nemesure B, Li X, et al. (2001) Incidence of open-angle glaucoma: the Barbados Eye Studies. The Barbados Eye Studies Group. Arch Ophthalmol 114:1058-1064.
- Leydhecker W, Akiyama K, Neumann HG, (1958) intraocular pressure in normal human eyes. Klin Monbl Augenheilkd Augenarztl Fortbild 133:662-670.
- Martin-du Pan R, Pruijm M, Burnier M, Sunaric-Megevand G, (2016) Pression artérielle et glaucome : attention à la pression artérielle nocturne. Rev Med Suisse 12:1518-1521.
- Klein BE, Klein R, Knudtson MD, (2005) intraocular pressure and systemic blood pressure: Longitudinal perspective: the Beaver Dam Eye Study. Br J Ophthalmol 89: 284-287.
- Zhao D, Cho J, Kim MH, Guallar E, (2014) the association of blood pressure and primary open-angle glaucoma: a meta-analysis. Am J Ophthalmol 158: 615-627.
- Wu SY, Leske MC, (1997) Associations with intraocular pressure in the Barbados Eye Study. Arch Ophthalmol 115: 1572.
- Dielemans I, Vingerling JR, Algra D, Hofman A, Grobbee DE, et al. (1995) Primary open-angle glaucoma, intraocular pressure, and systemic blood pressure in the general elderly population. The Rotterdam Study. Ophthalmology 102: 54-60.
- Tielsch JM, Katz J, Sommer A, Quigley HA, Javitt JC, (1995) Hypertension, perfusion pressure, and primary open-angle glaucoma. A population-based assessment. Arch Ophthalmol 113:216.
- Memarzadeh F, Ying-Lai M, Chung J, Azen SP, Varma R, (2010) Los Angeles Latino Eye Study Group. Blood pressure, perfusion pressure, and open-angle glaucoma: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci 51: 2872.
- Jimenez-Aragon F, Garcia-Martin E, Larrosa-Lopez R, Artigas-MartÃn JM, Seral-Moral P (2013) Role of color Doppler imaging in early diagnosis and prediction of progression in glaucoma. Biomed Res Int 1-11.
Citation: Mazamaesso T, Mamadou D, Pihou G, Nidain M, Abdoultif A, et al. (2021) Color Doppler Ultrasound Evaluation of Optic Nerve Head Arteries in Young Black Africans with Primary Open-angle Glaucoma (POAG). OMICS J Radiol 10: 338. DOI: 10.4172/2167-7964.1000338
Copyright: © 2021 Mazamaesso T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2990
- [From(publication date): 0-2021 - Dec 01, 2025]
- Breakdown by view type
- HTML page views: 2217
- PDF downloads: 773