Case Report Open Access
Colocutaneous Fistula as a Result of Chronic Hidradenitis Suppurativa
Richard S Hoehn and Bradley R Davis*Department of Surgery, University of Cincinnati School of Medicine, Cincinnati, OH, USA
- *Corresponding Author:
- Bradley R. Davis
Division of Education, ML #0558
University of Cincinnati, Department of Surgery
231 Albert Sabin Way, Room 1586 Cincinnati, OH, USA
Tel: 45267-0558
Fax: 513.558.3474
E-mail: davisbd@ucmail.uc.edu
Received date: July 26, 2014; Accepted date: October 06, 2014; Published date: October 11, 2014
Citation: Hoehn RS and Davis BR (2014) Colocutaneous Fistula as a Result of Chronic Hidradenitis Suppurativa. J Gastroint Dig Syst 4:224. doi:10.4172/2161-069X.1000224
Copyright: © 2014 Hoehn RS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Hidradenitis suppurativa is a chronic inflammatory disease affecting the skin of the axillae, groin, and perineum. It has many known sequelae including psychological stress, lymphedema, scarring, and fistula formation.
Case Presentation: TS is a 56-year-old male with a long history of hidradenitis affecting all of the classic areas. He has had excision and skin grafting of his axillae. He has also suffered from extensive involvement of his groin and perineum. Approximately 5 years ago he developed a spontaneous colocutaneous fistula at his umbilicus that eventually required surgical management.
Discussion: This is a new and unique presentation of hidradenitis that highlights the extensive morbidity caused by the disease. There are no other reports of hidradenitis affecting intra-abdominal tissues. Hidradenitis can be chronic and indolent, or it can be devastating. While multiple medical therapies exist, surgery is the only true cure.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Introduction: Hidradenitis suppurativa is a chronic inflammatory disease affecting the skin of the axillae, groin, and perineum. It has many known sequelae including psychological stress, lymphedema, scarring, and fistula formation. Case Presentation: TS is a 56-year-old male with a long history of hidradenitis affecting all of the classic areas. He has had excision and skin grafting of his axillae. He has also suffered from extensive involvement of his groin and perineum. Approximately 5 years ago he developed a spontaneous colocutaneous fistula at his umbilicus that eventually required surgical management. Discussion: This is a new and unique presentation of hidradenitis that highlights the extensive morbidity caused by the disease. There are no other reports of hidradenitis affecting intra-abdominal tissues. Hidradenitis can be chronic and indolent, or it can be devastating. While multiple medical therapies exist, surgery is the only true cure.
Keywords
Fistula; Hidradenitis suppurativa; Inflammatory disease
Introduction
Hidradenitis Suppurativa is a chronic, recurrent, inflammatory disease of the skin, initially presenting as tender subcutaneous nodules that spontaneously rupture or coalesce to form deep dermal, exquisitely painful abscesses. The inflammatory abscesses ultimately heal producing fibrosis, dermal contractures, and induration of the skin. It is most often seen in the second or third decade of life with a prevalence of 1-4%. The most common location of disease is the axilla (70%) followed by the perineum and groin. Once believed to be the result of apocrine gland infection it is now considered a disease of follicular occlusion [1].
There are several documented sequelae of chronic hidradenitis. With recurrent flares the skin becomes thickened and scarred in the areas affected [2]. Also, sinus tracts can form and drain purulent fluid [3]. It is well known that perianal fistulas can result from repeated flares [4,5]. There is also documentation of urethral fistula formation when inflammation occurs on the penis [6].
Case Presentation
TS is a 56 year old African American male with a past medical history of diabetes mellitus type 2, controlled with diet and infrequent insulin, and hidradenitis suppurativa for 29 years. The hidradenitis initially involved only his axillae and at that time he underwent excision and skin grafting bilaterally with good results. Since then he has developed significant groin and perineal disease. He has been treated multiple times for perianal fistulae and his numerous flares have left his genitals scarred and dysmorphic. He developed urethro-cutaneous fistulae at his ventral penoscrotal junction seven years ago. He has since been seen by a urologist and has been intermittently catheterized.
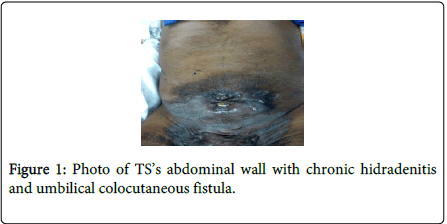
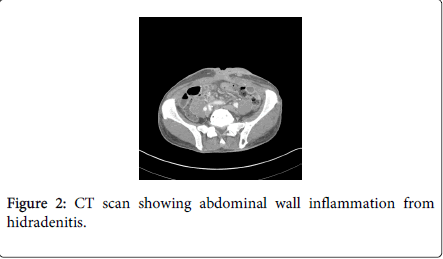
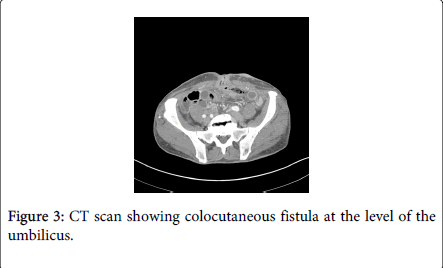
For 5 years TS has had sporadic drainage from his umbilicus that began to appear feculent (Figure 1). He underwent a colonoscopy that was not completed due to sharp bends in the sigmoid colon that could not be negotiated safely. The mucosa however appeared normal at that time with no stigmata of inflammatory bowel disease. A subsequent CT scan showed irregular soft tissue density in the anterior pelvis with soft tissue tracts extending to the umbilicus, encasing the sigmoid colon, and inseparable from the superior border of the bladder (Figures 2-4).
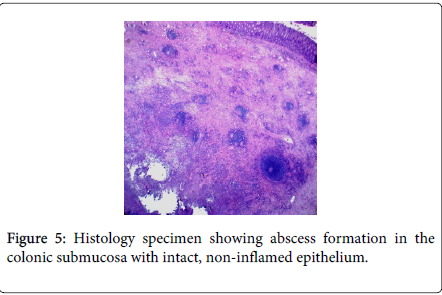
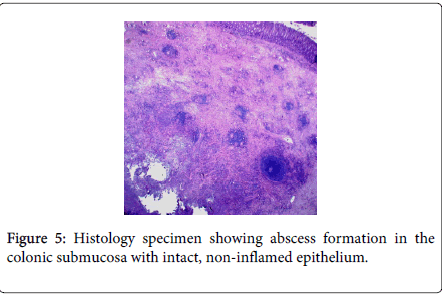
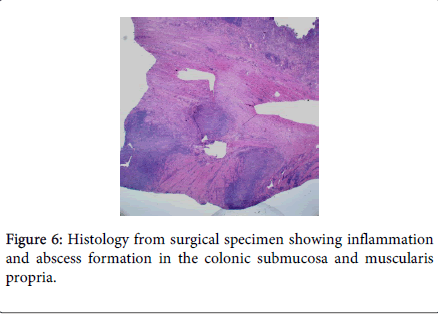
TS underwent a laparoscopic sigmoid colectomy with creation of a diverting loop ileostomy. At the time of surgery his sigmoid colon was noted to be adherent to the anterior abdominal wall requiring difficult dissection. His post-operative course was complicated by a prolonged ileus. His pathology report showed “Colonic fistula with abscess formation associated with marked acute and chronic inflammation and extensive fibrosis. Acute serositis. Negative for malignancy.” There was no evidence of neoplasm, diverticulitis, or inflammatory bowel disease. Histologic slides are significant for abscess formation in the submucosa and muscularis propria (Figures 5 and 6). There was no inflammation of the colonic mucosa.
Discussion
We believe this case is the first documentation of hidradenitis with intra-abdominal sequelae. Our literature search did not reveal any cases of hidradenitis involving abdominal organs. TS had chronic inflammation and lymphedema of his groin that progressed to his abdominal wall and subsequently developed a colocutaneous fistula. He has no history of intra-abdominal pathology. Histologic examination of his surgical specimen shows inflammation spreading from the abdominal wall towards the bowel, not vice-versa. This inflammation involved a substantial amount of sigmoid colon as well as bladder. Based on this, our belief is that the cause of his colocutaneous fistula is chronic hidradenitis suppurativa rather than inflammatory bowel disease or another intra-abdominal process.
Hidradenitis suppurativa, or acne inversa, is a disease that can cause significant morbidity as a result of the chronic relapsing inflammatory reaction in the axillae, groin, and perineum. The many known consequences of hidradenitis include psychological stress, lymphedema, fistulae, cancer, and even death [2,4,5,7-12].
Initial treatment of HS is often medical with topical agents, antibiotics, and proper hygiene. Often patients will present with subcutaneous abscess which are treated with incision and drainage. Then, depending on the individual circumstances, the patient is allocated to one of the multiple forms of nonsurgical management or to further surgery with curative intent once local inflammatory changes subside. Patients who present with an infected sinus tract and surrounding cellulitis may benefit from immediate unroofing and of the tract and delayed further intervention.
For cure in the elective setting, the entire affected area must be excised down to the subcutaneous fat. Then the resulting wound can be closed primarily without tension, or by secondary intention for larger wounds. Perineal and perianal wounds so treated rarely require a colostomy. Large wounds may also be treated by immediate or delayed split thickness skin graft. The recurrence rate after wide surgical excision has been reported at 0% for perianal disease, 3% for axillary disease and 37% for inguinoperineal disease [13].
The 10 year experience of Kagan et al shows promise for treating chronic hidradenitis with excision and primary closure, excision and healing by secondary intention, and excision and grafting based on their algorithm [14]. They treated patients with medically refractory hidradenitis and had no recurrences at their operative sites. While medical therapy should be first line treatment, surgical excision is the only curative option, and is often necessary in extensive disease [4,5,7,8,10].
References
- Yazdanyar S, Jemec GB (2011) Hidradenitissuppurativa: a review of cause and treatment.CurrOpin Infect Dis 24: 118-123.
- Faye O, Petit F, Poli F, Petit T, Wechsler J, et al. (2007) [Lymphedema as a complication of hidradenitissuppurativa in three patients].Ann DermatolVenereol 134: 567-569.
- Konety BR, Cooper T, Flood HD, Futrell JW (1996) Scrotal elephantiasis associated with hidradenitissuppurativa.PlastReconstrSurg 97: 1243-1245.
- Vickers MA (1975) Operative management of chronic hidradenitissuppurativa of the scrotum and perineum.J Urol 114: 414-416.
- Balik E, Eren T, Bulut T, Büyükuncu Y, Bugra D, et al. (2009) Surgical approach to extensive hidradenitissuppurativa in the perineal/perianal and gluteal regions.World J Surg 33: 481-487.
- Chaikin DC, Volz LR, Broderick G (1994) An unusual presentation of hidradenitissuppurativa: case report and review of the literature.Urology 44: 606-608.
- Revuz J (2009) Hidradenitissuppurativa.J EurAcadDermatolVenereol 23: 985-998.
- Slade DE, Powell BW, Mortimer PS (2003) Hidradenitissuppurativa: pathogenesis and management.Br J PlastSurg 56: 451-461.
- Zachary LS, Robson MC, Rachmaninoff N (1987) Squamous cell carcinoma occurring in hidradenitissuppurativa.Ann PlastSurg 18: 71-73.
- Endo Y, Tamura A, Ishikawa O, Miyachi Y (1998) Perianal hidradenitissuppurativa: early surgical treatment gives good results in chronic or recurrent cases.Br J Dermatol 139: 906-910.
- Moschella SL (1966) Hidradenitissuppurativa. Complications resulting in death.JAMA 198: 201-203.
- Alexander SJ (1979) Squamous cell carcinoma in chronic hydradenitissuppurativa: a case report.Cancer 43: 745-748.
- Davis BR(2010) FASCRS: Pruritus Ani, Pilonidal Sinus and HidradenitisSuppurativa.
- Kagan RJ, Yakuboff KP, Warner P, Warden GD (2005) Surgical treatment of hidradenitissuppurativa: a 10-year experience.Surgery 138: 734-740.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15443
- [From(publication date):
October-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10886
- PDF downloads : 4557