Cognitive Reserve: Evidence of Delayed of Dementia - A Case Report
Received: 22-Sep-2017 / Accepted Date: 26-Sep-2017 / Published Date: 10-Oct-2017
Abstract
The cognitive reserve is described as the efficient connectivity between neural networks which differs from the concept of cerebral reserve, indicative of larger volume of neural cells and, therefore, an increased ability to tolerate brain insults or effects of aging itself. A more detailed explanation would include the idea that the neural compensation mechanism uses alternative ways of the brain to perform activities considered complex. This activation is not observed in normal brains and may allow the individual to maintain levels of performance close to the basal state. In the present study we describe the case of an 85-year-old female, 15 years of schooling (Social Work), whose nephew reported having noticed a change in mood three years ago. There was no complaint regarding cognitive symptoms, neither by the elderly nor by relatives and caregivers. In the global geriatric evaluation the elderly presented a performance in the cognitive screening lower than expected, but also scored positively for depressive symptomatology. In this way the patient was included in a protocol of cognitive investigation which includes: laboratory tests, structural and functional neuroimaging, neuropsychological evaluation and pragmatic functionality assessment. The results of these evaluations indicated that there were no metabolic and blood changes, besides the results of the neuropsychological evaluation that suggested preserved cognitive performance, except for discrete changes in executive function and speed of reasoning, which would even be compatible with alterations associated with depressive symptomatology. The pragmatic functional evaluation presented results that corroborated with the neuropsychological assessment. On the other hand, the results of neuroimaging (structural and functional) suggested a significant reduction in cortical volume and, in addition, nucleocapsular, subinsular and thalamic regions. There was also generalized hypometabolism, especially bilateral frontotemporal regions. This neuroimaging result would be compatible with an elderly woman diagnosed with moderate to advanced dementia. However, this patient had an extraordinary cognitive reserve and did not show impairment of cognitive and functional performance in daily life activities. In this sense it is portrayed how the cognitive reserve in an elderly person can delay the onset of cognitive decline and prolong the quality of life of both the elderly and their family.
Keywords: Cognitive Reserve; Elderly; Dementia; Functional assessment; Geriatric; Positrons emission tomography
Case Report
We described the case of an 85-year-old female, 15 years of schooling (Social Work), whose nephew reported having noticed a change in mood three years ago. The onset of symptoms was observed and associated with the fact that the elderly had retired. They also reported that there was worsening of these symptoms about a year after the death of her brother. In addition to depressive symptoms, there was no complaint regarding cognitive symptoms, neither by the elderly nor by relatives and caregivers.
Despite this, the elderly had full-time assistance by formal caregivers because she had walking difficulties after a fall with mild head trauma three years ago and also began to show fear of falling. Thus, she has progressively stopped performing the instrumental activities. Still, the caregivers affirmed that the elderly was cognitively preserved and would be able to perform instrumental and basic activities of daily life, not performing them because of an emotional component, interpreted by the relatives as a way for the patient to draw the attention of the family.
This patient presented a history of hypertension, hypertriglyceridemia, severe sarcopenia, decreased visual and auditory acuity and depression with a treated episode in the past. The nephew also complained of a dysphagia, urinary and fecal incontinence and an episode of mental confusion due to a urinary infection.
In the global geriatric evaluation the patient presented a performance in the cognitive screening lower than expected, but also scored positively for depressive symptomatology. In the Mini Mental State Examination there were 24 points, with a total of 30 points, and in the simplified Geriatric Depression Scale, there were 07 points, for a total of 15 points. Therefore, a possible depressive disorder could be associated with impairment on cognitive performance.
In this way, the elderly was included in a cognitive research protocol, which included laboratory tests, structural neuroimaging and neuropsychological assessment.
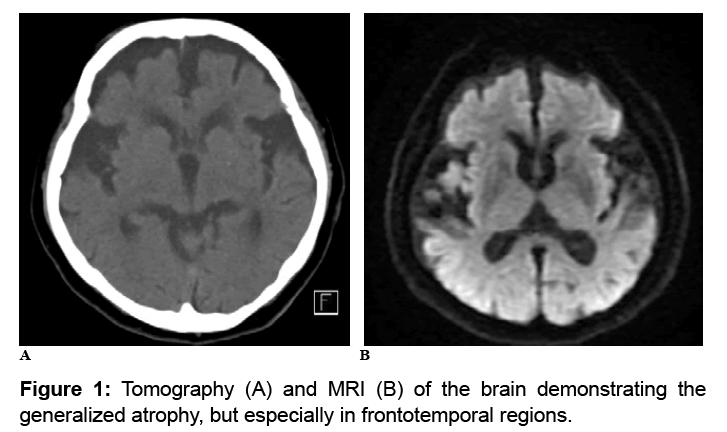
The results of these evaluations indicated that there were no metabolic and blood changes, besides the results of the neuropsychological evaluation that suggested preserved cognitive performance, except for discrete changes in executive function and speed of reasoning. These discrete impairments would be compatible with alterations associated with depressive symptomatology. However, the result of tomography and MRI of the brain (Figure 1) suggested a significant reduction in cortical volume and, in addition, nucleocapsular, subinsular and thalamic regions. This result would be compatible with an elderly diagnosed with moderate to advanced dementia, which surprised the health care team.
Because of this result that seemed incongruous between cognitive and neuroimaging tests, functional evaluations were requested: functional neuroimaging examination (Positron Emission Tomography - PET) and functional evaluation of the daily life activities.
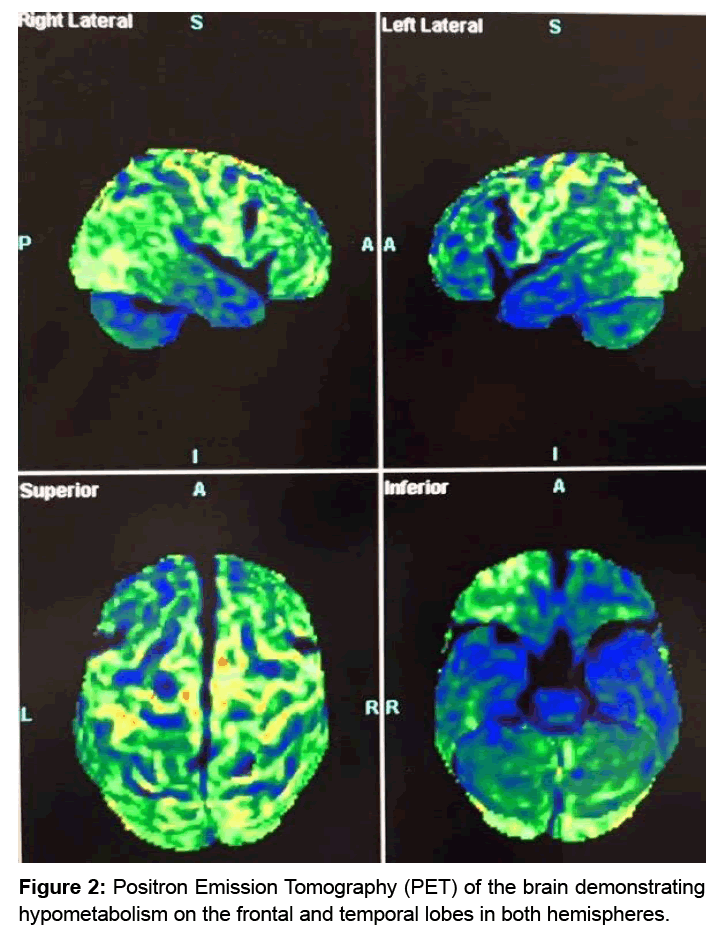
The result of the PET examination (Figure 2) indicated important bilateral frontotemporal hypometabolism and some areas with hypermetabolism in posterior regions and cerebellum. This corroborated with the result of previous structural neuroimaging. On the other hand, the functional evaluation suggested a result that it’s according with the result of the previous neuropsychological evaluation, that is, the elderly patient was able to perform daily activities without the mediator’s need in several tasks. There was only exception for activities that required executive skills (categorized thinking, clock design, puzzle building and colored block model) and that required verbal mediation, guiding and stimulating behavior.
The elderly referred that throughout her life she was interested in reading and discussing various topics. She also attended many years of formal education and worked up to three years before the onset of symptoms. It is important to emphasize that the reason that interrupted the work activity were problems of the public management that made impossible the operation of the shelter that the elderly was coordinating. Then, it is possible that the onset of depressive symptoms is due to the patient stopped performing, an activity that was very important and pleasurable to her.
Therefore, considering all these results, the interdisciplinary care team considered that it was not possibly a diagnosis of probable dementia, since the elderly woman did not fill the criteria in defined for such diagnosis.
The National Institute of Aging and the Association of Alzheimer’s [1] established in 2011 the following criteria for the diagnosis of probable Dementia of Alzheimer’s:
• Interference with ability to function at work or at usual activities;
• A decline from a previous level of functioning and performing;
• Not explained by delirium or major psychiatric disorder;
• Cognitive impairment established by history-taking from the patient and a knowledgeable informant; and objective bedside mental status examination or neuropsychological testing;
• Cognitive impairment involving a minimum of two cognitive domains;
• Insidious onset;
• Clear-cut history of worsening;
• Absence of other neurological diseases or adverse effects of medication.
On the other hand, a concept that has been described in neuroscience and seems to present an explanation for this apparent incompatibility between these results (cognitive/functional × structural/functional neuroimaging) is the cognitive reserve.
The cognitive reserve is described as the efficient connectivity between neural networks [2,3] which differs from the concept of cerebral reserve, which indicates a larger volume of neural cells and, therefore, an increased ability to tolerate brain insults or effects of aging itself [4]. A more detailed explanation would include the idea that the neural compensation mechanism uses alternative ways of the brain to perform activities considered complex [5]. This activation is not observed in normal brains and may allow the individual to maintain levels of performance close to the basal state [2,6].
Thereby, the elderly of this case report had showed an extraordinary cognitive reserve, since both brain functionality and, especially, cortical structure presented significant degeneration, but the elderly did not present impairment of cognitive and functional performance in daily life activities. It is known that the cognitive reserve is complex and variable among the elderly and is more important than the cerebral reserve [7]. Depending on the intrinsic characteristics of each individual and the environmental factors will play a fundamental role in the evolution of neurodegenerative pathology. When the cognitive reserve is high, the patient may not demonstrate symptoms related to cognitive decline for a long period of time. In this case, it is recommended to perform more complex and specifics tests, especially in patients with high functionality, such as neuropsychological assessment or strategies to perform activities of daily living in order to obtain a more particularized evaluation of the elderly [8].
For this reason the care team of the case made the decision to perform the PET examination and the evaluation of the pragmatic functionality of the elderly, complementing the results of neuropsychological assessments, structural neuroimaging and geriatric clinical evaluation.
In the literature it is well described that patients with Alzheimer’s disease and high cognitive reserve, when in the same stage of dementia as a patient with low reserve, present a much more advanced disease when analyzing the result of PET imaging [9,10]. This data corroborates with the present case study, since the cerebral metabolism presented is compatible with a dementia at an advanced stage, in which the individual would be presenting a considerable cognitive and functional impairment.
Studies involving neurogenesis still describe variables that may be associated with better development of an efficient pattern of neural connectivity. These are: the educational level [11], physical activity [12,13], professional occupation [14,15] intellectual level [16], cognitive stimulus [17] - as reading and thinking exercises - social interaction [18] and in some cases the individual’s own personality may interfere in the cognitive reserve . Such activities as described above have been shown to promote neurogenesis, especially in the hippocampus region [19].
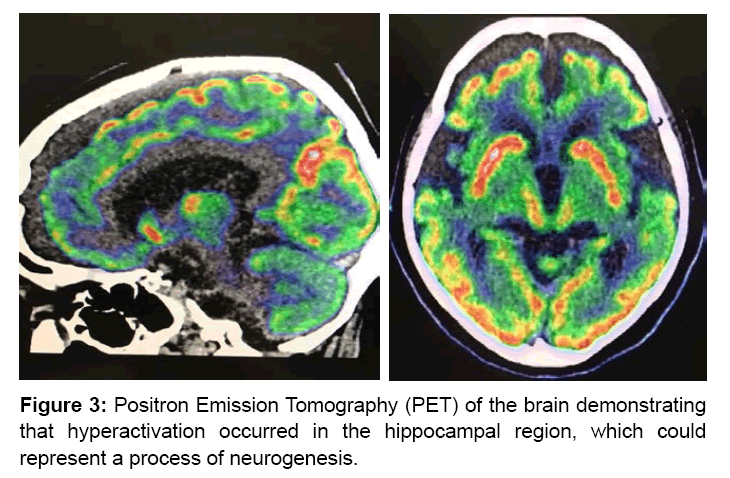
When observe at Figure 3, it is clear that hyperactivation occurred in the functional neuroimaging exam precisely in the hippocampal region, which could represent a process of neurogenesis of the elderly and would justify the clinical presentation.
In relation to variables that are associated with the development of a satisfactory neurogenesis pattern, it is worth mentioning that the elderly described in the present case report presented behaviors of intellectual formation, active work, readings, that is, an elderly attended to the majority of the possible predictors and protectors variables of the development of efficient neural connectivity.
Possibly these life habits favored more efficient neural connectivity and play a role in the current structural damage of the brain of the elderly, that is, probably this neurogenesis delays the symptomatic manifestation of a neurogenerative pathology.
In this sense it is portrayed how the cognitive reserve in an elderly person can delay the onset of cognitive decline and prolong the quality of life of both the elderly and their family.
Another important aspect to be analyzed is the adaptation of each individual, depending on their cognitive reserve, against the presence or not of dementia. There are cases of Alzheimer’s disease with greater cognitive reserve that had a greater neuronal activation in the exams, while healthy elderly with greater cognitive reserve had lower magnitude of activation. In other studies, individuals with Alzheimer’s disease and greater cognitive reserve had less activation, while healthy older adults with greater cognitive reserve had greater activation. These results can be justified by the compensatory reorganization of the neural networks that occur to compensate for the pathological changes [20]. When analyzing the brain structure in terms of impact on the cognitive reserve, it has been observed that the microstructure of the white matter may also contribute to the capacity of the cerebral reserve in humans [21].
One might suppose that in the next adverse event, such as an infectious disease or an episode of delirium, for example, in which it would represent a new insult to the brain of the described patient, could consume all the cognitive reserve and from that moment a diagnosed of neurodegenerative disorder could be possible because it would fulfill basic criteria, such as cognitive and functional impairment and changes in premorbid performance.
Finally, it is necessary to emphasize that patients with high cognitive reserve take longer to manifest the symptoms of memory loss. Some personal characteristics and activities carried out throughout life, especially physical activity, cognitive stimulation and participation in a social support network can help patients to delay the symptoms of cognitive loss and to prolong the quality of life, being more active for a longer time.
After all, the family and the elderly were invited to a return medical appointment in which all the results were explained and the orientations regarding the possible evolution of the cognitive and functional performance of the elderly were also clarified and discussed. It has been suggested that the elderly continue to be stimulated since neurogenesis continues to occur even in an already diseased brain.
References
- McKhann G, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr (2011) "The diagnosis of dementia due to Alzheimer's disease: Recommendations from the National Institute on Aging – Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease." Alzheimer's & Dementia: The Journal of the Alzheimer's Association 7: 263-269.
- Steffener J, Brickman AM, Rakitin BC, Gazes Y, Stern Y (2009) The impact of age-related changes on working memory functional activity. Brain Imaging Behav 3: 142-153.
- Stern Y (2002) What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc 8: 448-460.
- Satz P, Cole MA, Hardy DJ, Rassovsky Y (2011) Brain and cognitive reserve: mediator(s) and construct validity, a critique. J Clin Exp Neuropsychol 33: 121-130.
- Zarahn E, Rakitin B, Abela D, Flynn J, Stern Y (2007) Age-related changes in brain activation during a delayed item recognition task. Neurobiol Aging 28: 784-798.
- Barnett JH, Salmond CH, Jones PB, Sahakian BJ (2006) Cognitive reserve in neuropsychiatry. Psychol Med 36: 1053-1064.
- Stern Y (2012) Cognitive reserve in ageing and Alzheimer's disease. Lancet Neurol 11: 1006-1012.
- Garibotto V, Borroni B, Kalbe E, Herholz K, Salmon E, et al. (2008) Education and occupation as proxies for reserve in aMCI converters and AD: FDG-PET evidence. Neurology 71: 1342-1349.
- Kemppainen NM, Aalto S, Karrasch M, NÃ¥gren K, Savisto N, et al. (2008) Cognitive reserve hypothesis: Pittsburgh Compound B and fluorodeoxyglucose positron emission tomography in relation to education in mild Alzheimer's disease. Ann Neurol 63: 112-118.
- Helzner EP, Scarmeas N, Cosentino S, Portet F, Stern Y (2007) Leisure activity and cognitive decline in incident Alzheimer disease. Arch Neurol 64: 1749-1754.
- Angevaren M, Aufdemkampe G, Verhaar HJ, Aleman A, Vanhees L (2008) Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst Rev 3: CD005381.
- Kramer AF, Hahn S, Cohen NJ, Banich MT, McAuley E, et al. (1999) Ageing, fitness and neurocognitive function. Nature 400: 418-419.
- Stern Y, Albert S, Tang MX, Tsai WY (1999) Rate of memory decline in AD is related to education and occupation: cognitive reserve? Neurology 53: 1942-1947.
- Stern Y, Alexander GE, Prohovnik I, Stricks L, Link B, et al. (1995) Relationship between lifetime occupation and parietal flow: implications for a reserve against Alzheimer's disease pathology. Neurology 45: 55-60.
- Friedland RP, Brun A, Budinger TF (1985) Pathological and positron emission tomographic correlations in Alzheimer's disease. Lancet 1: 228.
- McGeer EG, Peppard RP, McGeer PL, Tuokko H, Crockett D, et al. (1990) 18Fluorodeoxyglucose positron emission tomography studies in presumed Alzheimer cases, including 13 serial scans. Can J Neurol Sci 1: 1-11.
- Stern Y, Habeck C, Moeller J, Scarmeas N, Anderson KE, et al. (2005) Brain networks associated with cognitive reserve in healthy young and old adults. Cereb Cortex 15: 394-402.
- Churchill JD, Galvez R, Colcombe S, Swain RA, Kramer AF, et al. (2005) Exercise, experience and the aging brain. Neurobiol Aging 23: 941-955.
- Scarmeas N, Habeck CG, Zarahn E, Anderson KE, Park A, et al. (2004) Covariance PET patterns in early Alzheimer's disease and subjects with cognitive impairment but no dementia: utility in group discrimination and correlations with functional performance. Neuroimage 23: 35-45.
- Teipel SJ, Meindl T, Wagner M, Kohl T, Bürger K, et al. (2009) White matter microstructure in relation to education in aging and Alzheimer's disease. J Alzheimers Dis. 17 : 571-583.
Citation: Zanetti M, Shigaeff N, Menzes AHT, Takahashi AA (2017) Cognitive Reserve: Evidence of Delayed of Dementia - A Case Report. J Dement 1: 101.
Copyright: © 2017 Shigaeff N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Usage
- Total views: 4868
- [From(publication date): 0-2017 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 3951
- PDF downloads: 917