Cocaine-Induced Midline Destructive Lesions (Cimdl): Diagnostic and Therapeutic Challenges
Received: 02-May-2022 / Manuscript No. jart-22-64550 / Editor assigned: 04-May-2022 / PreQC No. jart-22-64550 (PQ) / Reviewed: 18-May-2022 / QC No. jart-22-64550 / Revised: 20-May-2022 / Manuscript No. jart-22-64550 (R) / Accepted Date: 22-May-2022 / Published Date: 27-May-2022 DOI: 10.4172/2155-6105.100467
Abstract
Cocaine-induced midline destructive lesions (CIMDL) represent one of the rare but devastating consequences of cocaine addiction.
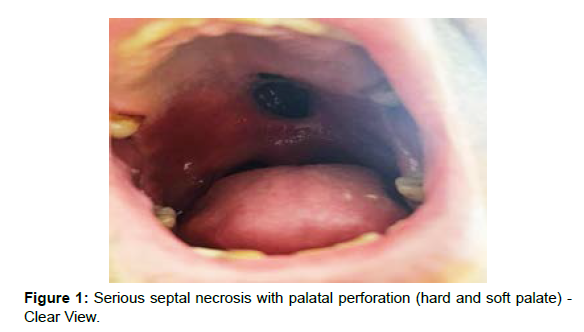
We report the case of a 52-year-old man with a history of severe and chronic cocaine addiction (up to 2g/d) for more than 25 years, who was referred by the ENT department for detoxification. The patient complained of repetitive epistaxis, nasal regurgitation with recurrent sinus infections, and chronic facial pain. On clinical examination, he showed necrosis of the septum complicated by a palatal perforation and presented a strong positivity for ANCA tests with a p-ANCA pattern. The CIMDL was retained after eliminating other etiological diagnoses.
The approach in the management of CIMDL is multidisciplinary, including dental professionals, maxillofacial surgeons, and psychologists.
The patient received initially conservative treatment with a palatal obturator prosthesis, but restarted cocaine intake 12 weeks after. There was progressing of the perforation with significant impact on the patient's quality of life.
In the present study, we review the available literature to discuss the diagnosis, and the therapeutics options in CIMDL, underlining the importance of abstinence as an absolute requirement, to consider surgical reconstruction.
Abbreviations:
CIMDL: Cocaine-Induced Destructive Midline Lesions; CUD: Cocaine Use Disorder; ANCA: Anti Neutrophil Cytoplasmic Antibodies; GPA: Granulomatosis with polyangiitis; cANCA: ANCA with cytoplasmic staining pattern; pANCA: ANCA with a perinuclear staining pattern; NE: neutrophil elastase
Keywords: Addiction, Addiction research, Addiction therapy, Cocaine-induced midline destructive lesions, CIMDL, Cocaine, Palatal perforations
Introduction
About 20 million people have abused cocaine in the previous year, as reported in the World Drug Report 2021 [1]. Cocaine abuse is known to cause severe consequences including tachydysthymia, severe hypertension, acute coronary syndrome, stroke, acute myocardial and renal failure, seizures, hyperthermia, cocaine-induced rhabdomyolysis, and fetal/maternal morbidity and mortality [2].
Snorting cocaine can lead to the development of serious and extensive destruction of the osteocartilaginous structures of nose, sinuses and palate [3]. These characteristic lesions are commonly called cocaine-induced midline destructive lesions (CIMDL) [4]. Prevalence of CIMDL is 4.8% among cocaine users [5].
CIMDLs represent a challenging problem for the physician from both the diagnostic and therapeutic point and view and there is still a lack of data in the literature [6].
We report the observation of a patient with a naso-palatal perforation induced by chronic and severe cocaine use. We discuss the diagnosis; and therapeutics options, underlining the importance of abstinence as an absolute requirement.
Case Report
The patient is M H., 52 years old, singer, has been divorced twice and has a 15 year old son.
He had a 25 years history of cocaine snorting (up to 2 grams inhaled per day), an irregular follow-up since 2019 and was referred by the ENT department for detoxification. He presented hyper nasal voice, repetitive epistaxis and nose reflux of liquids and solids. The ENT examination revealed an oronasal defect almost painless, with marginal necrosis, localized in the middle and posterior part of the hard palate, and almost total absence of the nasal septum. Imaging exploration revealed an absent nasal septum and a bony defect of the nasal cavity floor.
The microbiological tests and various biopsies of the perforation borders were negative for inflammatory, oncological and immunological diseases and showed unspecific reparative findings with no granulomas, vasculitis nor neoplastic cells. The Culture shows the growth of multi-resistant Staphylococcus aureus (S. aureus).
The search for anti-neutrophil cytoplasmic antibodies (ANCA) was positive. The diagnosis of CIMDL was retained following a complete physical, laboratory, radiological and immunological evaluation.
The CIMDL had a significant impact on the interpersonal relationships and the quality of life of the patient.
Obturator prosthesis has been proposed to repair palatal defects,
but he relapsed 12 weeks later. After one year, there was a worsening of the perforation. Some adjustments were necessary to adapt the patient to the new oral condition; alternatively, a new prosthesis was made while waiting for a surgical treatment.
Discussion
Diagnosis of CIMDLs
In conjunction with cocaine use, cocaine-induced destructive midline lesions (CIMDLs) are defined by the presence of at least two of the following three criteria (clinical or radiologic evidence):
(1) Septal perforation, and/or
(2) Perforation of the inferior turbinates and/or inter sinus-nasal septum, and/or
(3) Perforation of the hard palate [3].
Evaluation of a patient with destructive midface lesions should include an investigation of intranasal cocaine use. Localized ENT involvement, an inconsistent ANCA profile, and atypical biopsy findings for WG should be recognized as features of CIMDL [7]. To establish the diagnosis of CIMDL, a series of investigations including endoscopic, radiological, histopathological and serological examinations are imperative [4].
The patient has a history of cocaine addiction over 25 years (up to 2 grams inhaled per day).
The ear, nose and throat (ENT) evaluation and radiographic investigations revealed an oronasal septal perforation with marginal signs of necrosis, in the middle and the posterior third of the hard palate, which are common to several other differential diagnoses.
The differentiation of cocaine-induced midline destructive lesions (CIMDL) and limited granulomatosis with polyangiitis (GPA) may be difficult. The CIMDL is a pathology that mimics systemic diseases with positive anti-neutrophil cytoplasmic antibodies (ANCA) [8]. ANCA, specifically for neutrophil elastase (NE), represent a valuable diagnostic marker for CIMDL. Wiesner et al. reported high frequency (84%) of HNE ANCAs in patients presenting with CIMDL [9].
Treatment
Due to the lack of literature reports, there is no solid data on successful management [10]. A multidisciplinary approach is mandatory in the management of CIMDL, involving dental professionals, maxillofacial surgeons, and psychologists [11].
The therapy for palatal defects in CIMDL includes both reconstructive surgery and prosthetic obturators [6].
Cocaine-induced palatal perforations are dynamic and unstable in size [5].
Initially, the treatment approach may be conservative [12]. The palatal prosthesis with obturator is a fast and non-invasive option for patients starting their abstinence period. It will prevent the reflux during deglutition and will reduce nasal voice improving quality of life of the patients [13].
In this study, the results of the obturator were initially satisfactory, but the abstinence did not exceed twelve weeks and with progression of the disease, the patient was forced to make regular modifications of the product, with a consequent increase in cost and a decrease in patient satisfaction. Considering the aggravation of the perforation in our present case, the surgical approach became effectively the most adapted alternative to provide comfort to our patient.
There are many surgical techniques in the literature and the decision on the type of surgical intervention will depend on lesion location and size, the residual bone support and soft tissue in the area. Management should also take into consideration other factors such as the daily dose and duration of cocaine addiction, infections, general patient conditions and surgeon´s preferences [4]. However, it is only after a suitable interval of abstinence, which will confirm the patient's engagement, and if the defect stays relatively stable in terms of dimension over time, that a surgical intervention may be considered; if not then the reconstructive cover may fail with recurrence of perforations [6].
Thus, it is essential to advise the patient before the surgical act about the high probability of relapse, given the unknown state of the palatal microvascular lesions [14].
In the Di costa et al 2021 study, seven patients had no further progression of the lesions, and this was related to the quality and duration of abstinence, while the relapse in the eighth patient was responsible for the worsening of the perforation [11]. A 6-12 months drug-free period is generally accepted as valid though others even suggest 4 years. [15]. Moreover, the association of cocaine addiction and tobacco smoking may be responsible for a significant decrease in tissues perfusion [16]; consequently, it is recommended to quit also tobacco smoking.
Conclusion
The CIMDL is an handicapping disorder with significant impact on the quality of life of cocaine addicted individuals. CIMDL must be readily recognized by clinicians to provide appropriate treatment.
Treatment of palatal perforations in CIMDL includes reconstructive surgery and prosthetic obturators, the latter successfully improve symptoms, but long-term efficacy is strongly related to the evolution of the perforation. Only abstinence can interrupt progression.
References
- World Drug Report (2021) World Drug Report 2021. United Nations Office on Drugs and Crime, Austria.
- Richards JR, Jacqueline K (2022) Cocaine Toxicity. StatPearls Publishers, United States.
- Molteni M, Saibene AM, Luciano K, Maccari A (2016) Snorting the clivus away: an extreme case of cocaine-induced midline destructive lesion. BMJ Case Rep 2016: bcr2016216393.
- Trimarchi M, Bertazzoni G, Bussi M (2014) Cocaine induced midline destructive lesions. Rhinology 52(2):104-111.
- Barrientos J, Corchero G, Soler F (2021) Surgical treatment of cocaine-induced palatal perforations: Report of three cases and literature review. J Clin Exp Dent 13(2): e201-e206.
- Rampi A, Vinciguerra A, Bondi S, Policaro NS, Gastaldi G (2021) Cocaine-Induced Midline Destructive Lesions: A Real Challenge in Oral Rehabilitation. Int J Environ Res Public Health 18(6): 3219.
- Yaman H, Aydın Y, Yılmaz S, Onder E, Guclum E, Ozturk O (2011) Recurrent and Massive Life Threatening Epistaxis due to Nasal Heroin Usage. Clin Exp Otorhinolaryngol 4(3):159-161.
- Wiesner O, Russel KA, Lee AS, Jenne DE, Trimarchi M, et al. (2004) Antineutrophil cytoplasmatic antibodies reacting with human neutrophil elastase as a diagnostic marker for cocaine-induced midline destructive lesions but not autoimmune vasculitis. Arthritis Rheum 50: 2954-2965.
- Trimarchi M, Bondi S, Torre DE, Terreni MR, Bussi M (2017) Palate perforation differentiates cocaine-induced midline destructive lesions from granulomatosis with polyangiitis. Acta Otorhinolaryngol Ital 37(4): 281-285.
- Trimarchi M, Bussi M, Sinico RA, Meroni P, Specks U (2013) Cocaine-induced midline destructive lesions-An autoimmune disease?. Autoimmun Rev 12: 496-500.
- Di Cosola M, Ambrosino M, Limongelli L, Favia G, Santarelli A (2021) Cocaine-Induced Midline Destructive Lesions (CIMDL): A Real Challenge in Diagnosis. Int J Environ Res Public Health 18(15): 7831.
- Trimarchi M, Gregorini G, Facchetti F, Morassi ML, Manfredini C, et al. (2001) Cocaine-induced midline destructive lesions: clinical, radiographic, histopathologic, and serologic features and their differentiation from Wegener granulomatosis. Medicine 80: 391-404.
- Bains MK, Hosseini-Ardehali M (2005) Palatal perforations: past and present. Two case reports and a literature review. Br Dent J 199: 267-269.
- Colletti G, Allevi F, Valassina D, Bertossi D, Biglioli F (2013) Repair of cocaine-related oronasal fistula with forearm radial free flap. J Craniofac Surg 24:1734-1738.
- Berman M, Paran D, Elkayam O (2016) Cocaine-Induced Vasculitis. Rambam Maimonides Med J 7: 1-5.
- Moreno-Artero E, Querol-Cisneros E, Rodríguez-Garijo N, Tomás-Velázquez A, Antoñanzas J, et al. (2018) Mucocutaneous manifestations of cocaine abuse: A review. J Eur Acad Dermatol Venereol 32: 1420-1426.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Bouchra H, Meriem EY (2022) Cocaine-Induced Midline Destructive Lesions (Cimdl): Diagnostic and Therapeutic Challenges. J Addict Res Ther 13: 467. DOI: 10.4172/2155-6105.100467
Copyright: © 2022 Bouchra H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2786
- [From(publication date): 0-2022 - Nov 22, 2025]
- Breakdown by view type
- HTML page views: 2334
- PDF downloads: 452