Research Article Open Access
Closed-Loop VR-Based Interaction to Improve Walking in Parkinson's Disease
Raymond Chong1*, Kyoung-Hyun Lee1, John Morgan2, Shyamal Mehta2, Jake Griffin1, Jason Marchant1, Nathan Searle1, Joey Sims1 and Kapil Sethi21 Department of Physical Therapy, Georgia Health Sciences University, Augusta, Georgia, USA
2 Department of Neurology, Georgia Health Sciences University, Augusta, Georgia, USA
- *Corresponding Author:
- Raymond Chong
Department of Physical Therapy
Georgia Health Sciences University
Augusta, Georgia, USA
Tel: 706 721 1489
E-mail: rchong8@hotmail.com
Received date : October 27, 2011; Accepted date : December 07, 2011; Published date : December 13, 2011
Citation: Chong R, Lee KH, Morgan J, Mehta S, Griffin J, et al. (2011) Closed- Loop VR-Based Interaction to Improve Walking in Parkinson’s Disease. J Nov Physiother 1:101. doi:10.4172/2165-7025.1000101
Copyright: © 2011 Chong R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Visual cueing have been reported to help improve walking in people with Parkinson’s disease. However, many of these studies incorporate instructions and familiarization/practice, making it unclear whether the visual cues themselves were really effective or what parameters of walking are mutable. Here we used a closed-loop virtual visual cueing system to probe the automatic locomotor structures in subjects with idiopathic Parkinson’s disease and no freezing episodes. The cues moved in synchrony to the velocity of each subject’s walking but in the opposite direction, thereby giving rise to the perception of walking across a stationary landscape. In the absence of explicit instructions and practice, the virtual visual cues induced spontaneous changes among various walking kinematics in moderate-severe but not early-stage subjects. The largest effect was seen in the decrease in time to execute the first step (step initiation). Subjects completed the first step faster in the presence of the visual cues. Step length and walking speed on the other hand, decreased with exposure to the cues, i.e. subjects started out fast but then slowed down in the remainder of the walk. We conclude that the novel effects of the closed-loop visual cues produce mixed outcomes in walking performance. While step initiation improved spontaneously, the normalization of speed and step length would require cognitive strategies and practice as indicated in previous studie
Keywords
Bradykinesia; Freezing; GaitAid; Gait; Visual cues; Virtual reality; Visual dysfunction
Introduction
The basal ganglia-supplementary motor area (BG-SMA) loop is thought to be involved in a number of stereotypical and spontaneous behaviors including walking by inducing the circuitries of pattern generators in the brainstem and spinal cord [1-5]. In Parkinson’s disease (PD), anticipatory postural adjustments (APA) during voluntary stepping were found to be reduced after the area over the SMA underwent 1-Hz repetitive transcranial magnetic stimulations. The severity of PD symptoms was negatively correlated with APA duration. Stepping performance was not affected with stimulation of the dorsolateral premotor cortex [6].
As the disruption of the BG-SMA system increases with the progression of PD, patients become more reliant on the use of vision to move around. The reasons are still unclear but several hypotheses have emerged lately. For example, one possible benefit of visual cues is that it may help PD individuals to focus on their walking [7-12] possibly by aiding the ability to switch cognitive sets and holding short-term memory [13,14] or via greater cortical involvement [11,15-19].
The effect of visual cues in improving walking may occur spontaneously by circumventing the endogenous preparatory or setrelated stage of motor control [20-22] which is abnormal in PD [13,23]. The spontaneity is also somewhat validated by clinical observations in individuals with PD. Providing horizontal but not vertical or diagonal lines on the floor serves as a visual aid which helps overcome the phenomenon of shuffling gait or freezing when the individual attempts to walk [24]. It is not clear however, why transverse but not parallel lines are effective in triggering the walking [25,26]. Cadence increased more than controls when PD subjects walked while looking down at transverse lines. The increased cadence was accompanied by enhanced activation of the right lateral premotor region [27]. The beneficial effects of visual cues are confusing because they sometimes produce the opposite effect. PD patients are known to involuntarily slow down or stop walking when nearing a doorway [28,29]. Handwriting is larger when it is carried out with eyes closed [30].
Other studies suggest that the beneficial effect of visual cues on walking may be derived from the use of different neural pathways such as the cerebellar-premotor circuitry [27,31-34] including inputs from the superior parietal region [35] which is thought to enable visually-guided control of lower-body movements [36] when the basal-ganglia-supplementary connections are circumvented in PD [37-39]. Besides proprioceptive signals from the spinocerebellar tract [40], the cerebellum cortex also receives extensive visual signals from the superior colliculi, pretectal areas and lateral geniculate body. These neurons project to the cerebellar cortex via the purkinje and mossy fibres which convey slow- and fast-moving visual stimuli respectively [41].
The phenomenon of freezing in PD is thought to be related to irregularities of the frontal [42,43], brainstem [44-46] visual systems [47,48], and engrained synchronization of the basal ganglia system [49-51]. Bradykinetic gait including reduced step length is therefore thought to be a harbinger of things to come [52]. However, since not every patient goes on to develop dementia or freezing, the mechanism of visually-incited walking remains mysterious.
A number of studies have attempted to determine the effects of visual cues on improving walking performance in PD. These experiments included verbal prompting and practice trials, making it unclear how the visual cues themselves might have helped improve their walking. Clinicians often have to strike a delicate balance between allowing patients to explore the interactions between a walking aid and the surrounding workspace versus providing intense practice with detailed instructions and verbal cues. The former can lead to bad habits setting in while the latter can result in frustration and noncompliance. A better understanding of how visual aids can improve walking performance spontaneously would thus provide the needed scientific evidence of their beneficial effects which can then be augmented with practice and instructions.
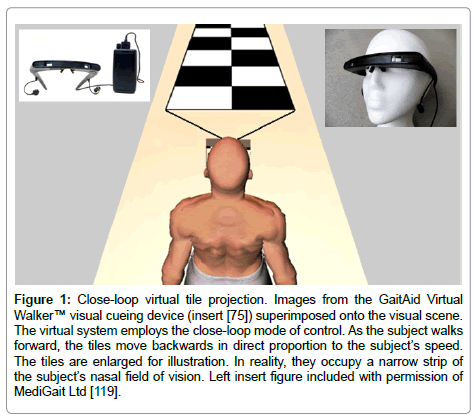
In the current study, subjects viewed virtual contrasting tiles while walking a linear trajectory without overt instructions or practice in order to determine the exclusive effect of the visual cues, as opposed to goal-oriented walking based on explicit instructions or practice [16,53-61]. The virtual visual cues in the current study are based on a closed-loop (feedback) model of stimulating the visual system [62,63]. The cues are synchronized to the speed of each subject’s forward advances but in the reverse direction. This imparts to the subject the perception of walking across stationary tiles (Figure 1). This mode of control keeps in check of any unwanted perception of central or peripheral visual flow from the cues as in the case of an open-loop system. In such a system, the cues move independently of the subject’s motion with the objective of augmenting or inducing the visual system and locomotor pattern generators [64]. The potential benefits of openloop systems however, are offset by their obvious drawback. Openloop schemes must dabble with the tricky challenge of enhancing walking while simultaneously creating conflicting sensory inputs to the central integrative mechanisms. Resolution of sensory discord is known to be inefficient in PD [65-71].
Figure 1: Close-loop virtual tile projection. Images from the GaitAid Virtual Walker™ visual cueing device (insert [75]) superimposed onto the visual scene. The virtual system employs the close-loop mode of control. As the subject walks forward, the tiles move backwards in direct proportion to the subject’s speed. The tiles are enlarged for illustration. In reality, they occupy a narrow strip of the subject’s nasal field of vision. Left insert figure included with permission of MediGait Ltd [119].
We hypothesized that the closed-loop visual cues will produce an improvement in walking performance in PD subjects in non-freezing moderate to more severe stages of the disease without incorporating a significant practice or learning component into the activity [72]. In particular, we expect the first step (step initiation) to occur faster. It is possible however, that the visual cues may also be distracting [73] and cause subjects to slow down. Subjects in the early stages of the disease who did not have significant walking impairments were also studied to determine the effects of the visual cues as a function of disease severity.
Materials and Methods
Subjects
47 subjects diagnosed with idiopathic Parkinson’s disease (PD) in their usual anti-PD drug regimen participated in the study. The study was approved by the institutional review board. 26 were classified as early-stage Hoehn & Yahr (H&Y) 1-2 (17 men and 9 women) while 21 subjects were classified as moderately-severe H&Y 2.5-4 (13 men and 8 women) [74]. Subjects averaged 68.8 +/- 7.9 years old with 8.1+/- 5.4 years disease duration. Freezing was not indicated in any of the subjects, nor was it observed during testing. Details of subjects’ characteristics are summarized in Table 1.
| Age (years) | UPDRS total | Brady | H&Y | Duration (years) | RAPID-1 | RAPID-2 | RAPID-3 | MM | PDQ8 | PDQ8-1 | PDQ8-2 | PDQ8-3 | PDQ8-4 | PDQ8-5 | PDQ8-6 | PDQ8-7 | PDQ8-8 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | 69/68 | 16.7/29.9* | 2.4/6* | 1.7/3* | 7.1/9.3 | 2.7/4.9* | 4.3/4.2 | 2.2/26.9* | 27.1/27.6 | 9.5/13.5* | 1.1/1.9* | 1.6/2 | 1.1/1.5 | 0.7/1 | 1.5/1.8 | 1/1.6 | 1.2/2* | 1.3/1.8 |
| Standard Deviation | 8/8 | 7.8/10.6 | 2/3.5 | 0.4/0.5 | 5.2/5.5 | 2.7/3.9 | 2.4/2.5 | 3.8/63.8 | 3.3/2.8 | 5.7/5.5 | 1.2/0.9 | 1.5/1.2 | 1.1/1.2 | 0.8/0.8 | 1/1.1 | 1.1/1.3 | 1.2/1 | 1.3/0.9 |
| Standard Error | 2/2 | 1.5/2.4 | 0.4/0.8 | 0.1/0.1 | 1/1.2 | 0.5/0.9 | 0.5/0.6 | 0.7/13.9 | 0.6/0.6 | 1.1/1.2 | 0.2/0.2 | 0.3/0.3 | 0.2/0.3 | 0.2/0.2 | 0.2/0.3 | 0.2/0.3 | 0.2/0.2 | 0.3/0.2 |
| Minimum | 55/50 | 4/13 | 0/0 | 1/2.5 | 0/1.2 | 0/0 | 1/1 | 0/0 | 20/18 | 0/5 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 | 0/0 |
| 25% Percentile | 64/63 | 10.5/22.6 | 0.9/3.6 | 1.5/2.5 | 3.1/4.8 | 0/1 | 2/2 | 0/0 | 25.8/26.5 | 5/9.5 | 0/1 | 0/1 | 0/0.5 | 0/0 | 1/1 | 0/0 | 0/1 | 0/1 |
| Median | 68/68 | 16.3/29.5 | 2.5/5 | 2/3 | 6.4/9 | 1.5/5 | 5/5 | 0/2 | 28/28 | 9/13 | 1/2 | 1.5/2 | 1/1 | 0/1 | 1.5/2 | 0.5/2 | 1/2 | 1/2 |
| 75% Percentile | 76/75 | 22.3/36.1 | 4/8.1 | 2/3 | 8.5/11.5 | 5/9 | 6/6.5 | 3/15 | 30/29.5 | 14/17 | 2/3 | 3/3 | 2/2.5 | 1.3/2 | 2/3 | 2/3 | 2/3 | 2/2 |
| Maximum | 84/84 | 34/52 | 6/13 | 2/4 | 24/25 | 9/12 | 8/8 | 12/270 | 30/30 | 21/24 | 4/3 | 4/4 | 4/4 | 2/2 | 3/4 | 3/4 | 4/3 | 4/4 |
| Lower 95% CI of Mean | 66/65 | 13.5/24.9 | 1.6/4.3 | 1.6/2.7 | 5/6.8 | 1.6/3.1 | 3.4/3.0 | 0.7/-2 | 25.8/26.3 | 7.1/11 | 0.6/1.5 | 1/1.5 | 0.6/0.9 | 0.4/0.6 | 1.1/1.3 | 0.5/0 | 0.7/1.5 | 0.8/1.4 |
| Upper 95% CI of Mean | 72/72 | 19.8/34.9 | 3.3/7.6 | 1.9/3.2 | 9.2/11.8 | 3.8/6.7 | 5.3/5.4 | 3.7/55.9 | 28.4/28.9 | 11.8/16 | 1.6/2.3 | 2.1/2.5 | 1.5/2 | 1/0.4 | 2/2.3 | 1.4/2.2 | 1.7/2.4 | 1.8/2.2 |
| Coefficient of Variation | 11.1/12.3 | 46.7/35.6 | 82.8/59 | 23.6/16.9 | 72.5/59.2 | 103.3/80.2 | 55.2/60.2 | 171.7/237.1 | 12.1/10.3 | 60.7/40.2 | 105.6/49.5 | 93.5/59.2 | 101.5/81.9 | 121/83.7 | 64.3/64.5 | 115.7/79.3 | 103.5/52.4 | 98.6/48.2 |
Table 1: Subject characteristics grouped by disease severity. (H&Y 1-2/H&Y 2.5-4). UPDRS, Section 3 of the Unified Parkinson’s Disease Rating Scale [76]; Total, total score; Brady, sum of items 40-44; H&Y, Hoehn and Yahr disease rating scale [74]; Duration, disease duration; RAPID-1, 2 and 3, postural instability questionnaire [77]; MMSE, mini-mental status examination [80]; PDQ, quality of life questionnaire [78,79]; PDQ8, total score; PDQ8-1 through 8, individual scores. * p < .05.
The visual device used in this study is the GaitAid Virtual Walker™ closed-loop system [75]. It has an eyeglass goggle component, dual earphones, and battery source. Earphones which provide auditory clicks also come as part of the device and can be used in conjunction with the visual cues if desired. The battery source is worn on the midlateral aspect of the subject’s hip and contains a tri-axial accelerometer system. When the device is turned on, virtual visual cues in the form of tiled flooring can be seen through the lenses along the nasal visual field. The device operates in the closed-loop mode in which the accelerometers detect the subject’s vertical motions and move the tiled flooring accordingly. The virtual tiles are displayed as black and white squares arranged in two strips of alternating color. They are designed to mimic the real thing in that they not only gradually decrease in size as they lay further away from the subject but the vertical edges are also angled accordingly (Figure 1). As the subject walks, the nearest and largest pair of tiles disappears and is replaced by the next pair ahead while expanding to the same size as the disappearing pair. Adjacent pairs of tiles go through the same replacement algorithm. The overall visual effect is that the speed of the tile movements feels proportional to the subject’s movements. The tiles appear to be stationary and the subject perceives walking over them [62,63].
Procedures
All instructions about what to do during the experiments were explained to the subjects while they were seated. Subjects were then familiarized to the goggle still sitting in the chair. They moved their head around while viewing the device that was alternately turned On and Off several times. Subjects were told that during testing, they were to walk at their comfortable pace looking ahead (i.e. not to stare down at their feet) and to keep walking until asked to stop. Subjects then stood up and the first trial was administered immediately. Practice trials were not allowed, i.e. the first trial of each visual condition was the first time subjects experienced them walking. Each visual condition (On versus Off) was dispensed thrice in alternating order with the starting condition counterbalanced among the subjects. Subjects wore the goggle the entire time during the experiment. In each trial, subjects’ walking performance over 9.14 meters (30 feet) of level and unobstructed surface was videotaped for blinded analyses afterwards. The primary tester walked with the subject but slightly behind in order to avoid providing any visual feedback or interference to the subject. A gait belt was applied around the subject’s waist to ensure safety.
Data analyses
The primary outcome measures were the change in walking kinematics: duration of first step (step initiation), duration of walking over 9.14 meters, step length, walking speed and cadence. They were calculated based on the distance walked, the number of steps taken and the duration of walking. Changes were quantified as percent-change values by calculating the difference between walking performance with the visual cues On versus Off divided by visual cues Off. The group mean of the first trial and average of three trials in each kinematic measure was then subjected to a one-sample two-tailed t-test to test the effect of the visual cues against the null hypothesis (i.e. zero percent change in performance between visual cues Off and On).
Secondary outcome measures included the use of Pearson simple linear correlation analyses to determine the associations among the walking kinematic variables and disease profiles: disease severity [76], disease duration, postural instability [77], quality of life [78,79] and cognitive state [80]. Additional secondary analyses included comparing the two groups of subjects using independent t-tests. In order to increase the power of detecting group differences, no corrections to were made to minimize the inflated Type I error. The alpha level for the test of significance was set at p < .05 in all cases. All analyses were carried out with the GraphPad Prism software (GraphPad Prism v5.04, GraphPad Software Inc., CA).
Results
In the H&Y stages 2.5-4 group, with the visual cues turned On, subjects’ first step initiation was faster, they took shorter steps and walked slower (p < .05) without changing their cadence. The visual cues produced the strongest effect in speeding up step initiation (Table 2). The correlations among the walking kinematics ranged between -.511 and .711. Changes in step length covaried positively with walking speed (p < .05, Table 3). In addition, faster step initiation was associated with a higher feelings of depression and incidence of muscle cramps (p < .05) while a larger decrease in step length was associated with a higher degree of bradykinesia and disease severity (p < .05). Faster cadence was associated with a higher degree of body bradykinesia and communication problems (p < .05, Table 4).
| Cues Off | Cues On | % Change | Effect size | 95% CI | ||
|---|---|---|---|---|---|---|
| Step Initiation (s) | T1 | 1.23 (.35) | 1.21 (.52) | -1.6 | .05 | -14.8 to 11.7 |
| Avg | 1.17 (.32) | 1.10 (.35) | -6.2* | .21 | -11.5 to -.9 | |
| Step Length (m) | T1 | .48 (.16) | .47 (.17) | -4.1* | .10 | -8.1 to -.1 |
| Avg | .50 (.16) | .49 (.17) | -2.8* | .10 | -5.1 to -.5 | |
| Walking Speed (m/s) | T1 | .83 (.29) | .80 (.30) | -5.2* | .10 | -10.3 to -.1 |
| Avg | .87 (.29) | .88 (.32) | -0.8 | .03 | -6.4 to 4.8 | |
| Cadence (steps/min) | T1 | 102.01 (15.22) | 100.72 (19.16) | -1.6 | .08 | -5.6 to 2.3 |
| Avg | 104.80 (16.31) | 103.03 (17.94) | -1.8 | .10 | -5.4 to 1.9 |
Table 2: Effect of closed-loop visual cues on the change in walking kinematics in the Hoehn & Yahr 2.5-4 group. % change is expressed as a ratio of visual cues turned On minus Off and divided by Off. T1, first trial; Avg, mean of three trials. Effect size is based on Cohen’s d [106]. *p < .05 compared to the statistical null hypothesis.
| Step Length (m) | Walking Speed (m/s) | Cadence (steps/min) | |||||
|---|---|---|---|---|---|---|---|
| T1 | Avg | T1 | Avg | T1 | Avg | ||
| Step Initiation (s) | T1 | 0.016 | -0.057 | -0.356 | -0.429 | -0.511* | 0.061 |
| Avg | 0.126 | 0.004 | -0.159 | -0.451* | -0.358 | 0.214 | |
| Step Length (m) | T1 | - | - | 0.711* | 0.392 | -0.074 | -0.148 |
| Avg | - | - | 0.454* | 0.414 | -0.181 | -0.127 | |
| Walking Speed (m/s) | T1 | - | - | - | - | 0.646* | -0.064 |
| Avg | - | - | - | - | 0.427 | 0.510* | |
Table 3: Association among the changes in walking performance as a function of the visual cues in the H&Y 2.5-4 group. T1, first trial; Avg, mean of three trials. * indicates a significant association, p < .05.
| UPDRS | H&Y | Postural Instability | MMSE | Quality of Life | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Brady | RAPID-1 | RAPID-2 | RAPID-3 | PDQ8 | PDQ8-1 | PDQ8-2 | PDQ8-3 | PDQ8-4 | PDQ8-5 | PDQ8-6 | PDQ8-7 | PDQ8-8 | ||||
| Step Initiation (s) | T1 | 0.11 | -0.06 | 0.08 | -0.15 | 0.16 | 0.04 | 0.17 | 0.23 | 0.02 | 0.09 | 0.34 | -0.13 | 0.18 | 0.20 | -0.27 | 0.41 |
| Avg | 0.02 | 0.06 | 0.04 | 0.29 | 0.14 | 0.21 | 0.21 | 0.34 | 0.31 | 0.50* | 0.59* | 0.04 | 0.21 | 0.02 | -0.50* | 0.23 | |
| Step Length (m) | T1 | 0.12 | -0.39 | -0.16 | -0.10 | 0.07 | -0.05 | 0.13 | -0.04 | -0.26 | 0.06 | -0.18 | -0.18 | -0.13 | 0.13 | -0.29 | 0.01 |
| Avg | -0.17 | -0.72* | -0.41* | -0.31 | -0.11 | -0.10 | 0.06 | -0.26 | -0.36 | 0.10 | -0.38 | -0.07 | -0.22 | 0.11 | -0.26 | -0.11 | |
| Walking Speed (m/s) | T1 | 0.09 | 0.01 | 0.09 | 0.10 | 0.21 | 0.11 | -0.09 | -0.04 | 0.00 | -0.03 | -0.12 | -0.03 | -0.20 | -0.17 | -0.09 | 0.08 |
| Avg | -0.34 | -0.15 | -0.11 | -0.12 | 0.05 | -0.06 | -0.10 | -0.38 | -0.31 | -0.28 | -0.38 | -0.23 | -0.28 | -0.33 | -0.09 | 0.03 | |
| Cadence (steps/min) | T1 | -0.02 | 0.431* | 0.16 | 0.14 | 0.13 | 0.17 | -0.32 | -0.16 | 0.20 | -0.17 | -0.14 | 0.24 | -0.30 | -0.45* | 0.13 | -0.09 |
| Avg | 0.235 | 0.05 | -0.09 | 0.173 | -0.12 | 0.13 | 0.08 | 0.18 | 0.30 | 0.36 | 0.12 | 0.40 | -0.05 | 0.07 | -0.01 | -0.12 | |
Table 4: Association between subjects’ characteristics and change in walking performance in the H&Y 2.5-4 group. T1, first trial; Avg, mean of three trials. * indicates a significant association, p < .05. Abbreviations are the same as in Table 1.
The H&Y stages 1-2 group did not show a change in any of the walking kinematics as a function of the visual cues. Compared to the H&Y stages 2.5-4 group, average step initiation (1.13 ± .25 s versus 1.17 ± .32 s), walking speed (.91 ± .21 m/s versus .83 ± .29 m/s) and cadence (99.73 ± 9.66 steps/min versus 104.80 ± 15.31 steps/min) were similar when walking without the visual cues whereas step length was shorter (.5 ± .16 m versus .57 ± .09 m, p =.034, 1-tailed).
Discussion
The results of the study demonstrate that close-loop virtual visual cues can spontaneously change the walking kinematics in individuals with moderately severe PD. These changes occurred in the absence of explicit instructions and practice [81,82]. They did not however, translate into what one would typically consider to be better performance in terms of normalizing step length and walking speed.
Walking and other over-learned movements no longer become instinctive in PD but require effort [83-87] especially in tasks that require changing set [13,57,66,68,72,88-91]. The faster step initiation could therefore arise from the visual cues substituting the defective basal ganglia system in changing set from standing to taking the first step. Cadence is generally higher in PD [92,93] though it did not change as a function of the visual cues in the current study. Steps are typically shortened in PD, possibly because maintaining a normal step necessitates higher muscular effort and coordination [13,94]. In terms of the decreased walking speed, it did not relate with any of the disease profiles. Walking speed is a complex gait parameter that is not associated with components of motor skills such as force control, agility, or weight transfer [95].
The step length and walking speed are similar to those reported in the literature for moderate to severe PD [96,97] and higher than PD subjects who withheld their anti-PD medications [98]. The ability to modulate step initiation holds promise for improving walking in PD [99] as cognitive strategies could then be incorporated into the practice by intentionally increasing step length and speed [61,100-105].
Although the magnitudes of change were small by statistical standards [106], they are remarkable considering that subjects were completely naïve to the visual cueing device and the short distance that subjects walked during the tests. The significant decreases in walking speed and step length likely reflects a combination of the distracting visual cues and an apparent effort to walk more carefully since the cues do reduce the central visual passage. The novelty of wearing the goggle likely caused the PD subjects to engage in dual-tasking. It is known that many of them have trouble with such encounters [107-112]. The potential interference is especially illuminating considering that the visuospatio-perceptual system must process both the visual cues and the surrounding concurrently [73,113,114]. Even the instruction manual recommends walking slowly in the beginning and to stop if unsure [115].
The findings of the association among the walking gait changes and disease profiles are consistent with the cognitive mechanisms underlying the beneficial effects of visual cues. The associations between the magnitude of decrease in step length and the higher level of postural bradykinesia and severity of disease could be a reflection of the increasing difficulty in modulating muscle forces as a result of disease progression. As the disease worsens, mental states such as depression and physical impairments such as muscle fatigue, cramps or difficulty getting dressed have accumulating effects on PD patients’ overall quality of life including fear of falling [77,116-118]. These factors may hamper efforts to provide meaningful rehabilitation techniques to retain the ability to walk in these people [59].
The failure to find any effect of the visual cues in the H&Y 1-2 group was expected as hypothesized. These subjects have not yet developed overt problems with their walking. The null outcome was therefore not surprising.
In conclusion, the current study demonstrates that in the absence of instructions and practice, closed-loop virtual visual cues can spontaneously increase step initiation speed but decreased walking speed and step length in patients with moderately severe PD. The increased step length and walking speed reported in previous studies from using visual cues is probably due to cognitive strategies and practice.
Funding
This work was supported by the Augusta Chapter of the National Parkinson Foundation, Georgia, USA.
References
- Cass WA, Peters LE, Smith MP (2005) Reductions in spontaneous locomotor activity in aged male, but not female, rats in a model of early Parkinson's disease. Brain Res 1034: 153-161.
- Hanakawa T, Katsumi Y, Fukuyama H, Honda M, Hayashi T, et al. (1999) Mechanisms underlying gait disturbance in Parkinson's disease: a single photon emission computed tomography study. Brain 122: 1271-1282.
- Loy DN, Magnuson DS, Zhang YP, Onifer SM, Mills MD, et al. (2002) Functional redundancy of ventral spinal locomotor pathways. J Neurosci 22: 315-323.
- Mena-Segovia J, Bolam JP, Magill PJ (2004) Pedunculopontine nucleus and basal ganglia: Distant relatives or part of the same family? TINS 27: 585-588.
- Takakusaki K, Tomita N, Yano M (2008) Substrates for normal gait and pathophysiology of gait disturbances with respect to the basal ganglia dysfunction. J Neurol 255 Suppl 4: 19-29.
- Jacobs JV, Lou JS, Kraakevik JA, Horak FB (2009) The supplementary motor area contributes to the timing of the anticipatory postural adjustment during step initiation in participants with and without Parkinson's disease. Neurosci 164: 877-885.
- Devinsky O, Morrell MJ, Vogt BA (1995) Contributions of anterior cingulate cortex to behaviour. Brain 118: 279-306.
- Kobayashi Y, Inoue Y, Isa T (2004) Pedunculo-pontine control of visually guided saccades. Prog Brain Res 143: 439-445.
- Mathot S, Theeuwes J (2011) Visual attention and stability. Philos Trans R Soc Lond B Biol Sci 366: 516-527.
- Sawamoto N, Honda M, Hanakawa T, Fukuyama H, Shibasaki H (2002) Cognitive slowing in Parkinson's disease: a behavioral evaluation independent of motor slowing. J Neurosci 22: 5198-5203.
- Sohn YH, Kim GW, Huh K, Kim JS (1998) Dopaminergic influences on the P300 abnormality in Parkinson's disease. J Neurol Sci 158: 83-87.
- Steinmetz MA, Constantinidis C (1995) Neurophysiological evidence for a role of posterior parietal cortex in redirecting visual attention. Cereb Cortex 5: 448-456.
- Hayes AE, Davidson MC, Keele SW, Rafal RD (1998) Toward a functional analysis of the basal ganglia. J Cog Neurosci 10: 178-198.
- van Schoor NM, Smit JH, Pluijm SM, Jonker C, Lips P (2002) Different cognitive functions in relation to falls among older persons. Immediate memory as an independent risk factor for falls. J Clin Epidemiol 55: 855-862.
- Richards M, Cote LJ, Stern Y (1993) The relationship between visuospatial ability and perceptual motor function in Parkinson's disease. J Neurol Neurosurg Psychiatry 56: 400-406.
- Rochester L, Nieuwboer A, Baker K, Hetherington V, Willems AM, et al. (2007) The attentional cost of external rhythmical cues and their impact on gait in Parkinson's disease: effect of cue modality and task complexity. J Neural Transm 114: 1243-1248.
- Rossignol S, Dubuc R, Gossard JP (2006) Dynamic sensorimotor interactions in locomotion. Physiol Rev 86: 89-154.
- Sherk H, Fowler GA (2001) Neural analysis of visual information during locomotion. Prog Brain Res 134: 247-264.
- Shi LH, Luo F, Woodward DJ, Chang JY (2004) Neural responses in multiple basal ganglia regions during spontaneous and treadmill locomotion tasks in rats. Exp Brain Res 157: 303-314.
- Azulay JP, Mesure S, Blin O (2006) Influence of visual cues on gait in Parkinson's disease: contribution to attention or sensory dependence? J Neurol Sci 248: 192-195.
- Kien J (1990) Neuronal activity during spontaneous walking--I. Starting and stopping. Comp Biochem Physiol A Comp Physiol 95: 607-621.
- Sacks O (1985) The man who mistook his wife for a hat and other clinical tales. Simon & Schuster, New York.
- Sohn MH, Ursu S, Anderson JR, Stenger VA, Carter CS (2000) The role of prefrontal cortex and posterior parietal cortex in task switching. Proc Natl Acad Sci U S A 97: 13448-13453.
- Martin JP (1967) The basal ganglia and posture. Pitman Medical, London.
- Hovestadt A, de Jong GJ, Meerwaldt JD (1987) Spatial disorientation as an early symptom of Parkinson's disease. Neurol 37: 485-487.
- Lee AC, Harris JP, Calvert JE (1998) Impairments of mental rotation in Parkinson's disease. Neuropsychologia 36: 109-114.
- Hanakawa T, Fukuyama H, Katsumi Y, Honda M, Shibasaki H (1999) Enhanced lateral premotor activity during paradoxical gait in Parkinson's disease. Ann Neurol 45: 329-336.
- Cowie D, Limousin P, Peters A, Day BL (2010) Insights into the neural control of locomotion from walking through doorways in Parkinson's disease. Neuropsychologia 48: 2750-2757.
- Rahman S, Griffin HJ, Quinn NP, Jahanshahi M (2008) The factors that induce or overcome freezing of gait in Parkinson's disease. Behav Neurol 19: 127-136.
- Ondo WG, Satija P (2007) Withdrawal of visual feedback improves micrographia in Parkinson's disease. Mov Disord 22: 2130-2131.
- Azulay JP, Mesure S, Amblard B, Blin O, Sangla I, et al. (1999) Visual control of locomotion in Parkinson's disease. Brain 122: 111-120.
- Glickstein M (2003) Subcortical projections of the parietal lobes. Adv Neurol 93: 43-55.
- Goldberg G (1985) Supplementary motor area structure and function: Review and hypotheses. Behav Brain Sci 8: 567-616.
- van Donkelaar P, Stein JF, Passingham RE, Miall RC (1999) Neuronal activity in the primate motor thalamus during visually triggered and internally generated limb movements. J Neurophysiol 82: 934-945.
- Wise SP, Boussaoud D, Johnson PB, Caminiti R (1997) Premotor and parietal cortex: corticocortical connectivity and combinatorial computations. Ann Rev Neurosci 20: 25-42.
- Shipp S, Blanton M, Zeki S (1998) A visuo-somatomotor pathway through superior parietal cortex in the macaque monkey: Cortical connections of areas V6 and V6A. Eur J Neurosci 10: 3171-3193.
- Chen YC, Thaler D, Nixon PD, Stern CE, Passingham RE (1995) The functions of the medial premotor cortex. II. The timing and selection of learned movements. Exp Brain Res 102: 461-473.
- de Jong BM, Frackowiak RS, Willemsen AT, Paans AM (1999) The distribution of cerebral activity related to visuomotor coordination indicating perceptual and executional specialization. Cog Brain Res 8: 45-59.
- Thaler D, Chen YC, Nixon PD, Stern CE, Passingham RE (1995) The functions of the medial premotor cortex. I. Simple learned movements. Exp Brain Res 102: 445-460.
- Arshavsky YI, Gelfand M, Orlovsky GN (1983) The cerebellum and control of rhythmical movements. TINS 6: 417-422.
- Glickstein M, Stein J (1991) Paradoxical movement in Parkinson's disease. Trends Neurosci 14: 480-482.
- Niedermeyer E (2008) Akinesia and the frontal lobe. Clin EEG Neurosci 39: 39-42.
- Owen AM, Doyon J, Dagher A, Sadikot A, Evans AC (1998) Abnormal basal ganglia outflow in Parkinson's disease identified with PET: Implications for higher cortical functions. Brain 121: 949-965.
- Kuo SH, Kenney C, Jankovic J (2008) Bilateral pedunculopontine nuclei strokes presenting as freezing of gait. Mov Disord 23: 616-619.
- Pahapill PA, Lozano AM (2000) The pedunculopontine nucleus and Parkinson's disease. Brain 123: 1767-1783.
- Tessitore A, Hariri AR, Fera F, Smith WG, Chase TN, et al. (2002) Dopamine modulates the response of the human amygdala: A study in Parkinson's disease. J Neurosci 22: 9099-9103.
- Helmich RC, Derikx LC, Bakker M, Scheeringa R, Bloem BR, et al. (2010) Spatial remapping of cortico-striatal connectivity in Parkinson's disease. Cereb Cortex 20: 1175-1186.
- Uc EY, Rizzo M, Anderson SW, Qian S, Rodnitzky RL, et al. (2005) Visual dysfunction in Parkinson disease without dementia. Neurol 65: 1907-1913.
- Lewis SJ, Barker RA (2009) A pathophysiological model of freezing of gait in Parkinson's disease. Parkinsonism Relat Disord 15: 333-338.
- Palmer SJ, Lee PW, Wang ZJ, Au WL, McKeown MJ (2010) Theta, beta but not alpha-band EEG connectivity has implications for dual task performance in Parkinson's disease. Parkinsonism Relat Disord 16: 393-397.
- Rektor I, Balaz M, Bockova M (2010) Cognitive event-related potentials and oscillations in the subthalamic nucleus. Neurodegener Dis 7: 160-162.
- Chee R, Murphy A, Danoudis M, Georgiou-Karistianis N, Iansek R (2009) Gait freezing in Parkinson's disease and the stride length sequence effect interaction. Brain 132: 2151-2160.
- Griffin HJ, Greenlaw R, Limousin P, Bhatia K, Quinn NP, et al. (2011) The effect of real and virtual visual cues on walking in Parkinson's disease. J Neurol 258: 991-1000.
- Hausdorff JM, Schaafsma JD, Balash Y, Bartels AL, Gurevich T, et al. (2003) Impaired regulation of stride variability in Parkinson's disease subjects with freezing of gait. Exp Brain Res 149: 187-194.
- Jiang Y, Norman KE (2006) Effects of visual and auditory cues on gait initiation in people with Parkinson's disease. Clin Rehabil 20: 36-45.
- Lewis GN, Byblow WD, Walt SE (2000) Stride length regulation in Parkinson's disease: the use of extrinsic, visual cues. Brain 123: 2077-2090.
- Morris ME, Iansek R, Matyas TA, Summers JJ (1996) Stride length regulation in Parkinson's disease. Normalization strategies and underlying mechanisms. Brain 119: 551-568.
- Picelli A, Camin M, Tinazzi M, Vangelista A, Cosentino A, et al. (2010) Threedimensional motion analysis of the effects of auditory cueing on gait pattern in patients with Parkinson's disease: a preliminary investigation. Neurol Sci 31: 423-430.
- Rochester L, Hetherington V, Jones D, Nieuwboer A, Willems AM, et al. (2005) The effect of external rhythmic cues (auditory and visual) on walking during a functional task in homes of people with Parkinson's disease. Arch Phys Med Rehabil 86: 999-1006.
- Suteerawattananon M, Morris GS, Etnyre BR, Jankovic J, Protas EJ (2004) Effects of visual and auditory cues on gait in individuals with Parkinson's disease. J Neurol Sci 219: 63-69.
- Zijlstra W, Rutgers AW, Van Weerden TW (1998) Voluntary and involuntary adaptation of gait in Parkinson's disease. Gait Posture 7: 53-63.
- Baram Y (1999) Walking on tiles. Neural Proc Lett 10: 81-87.
- Baram Y (2002) Walking on virtual tiles. Neural Proc Lett 16: 227-233.
- Ferrarin M, Brambilla M, Garavello L, Di Candia A, Pedotti A, et al. (2004) Microprocessor-controlled optical stimulating device to improve the gait of patients with Parkinson's disease. Med Biol Eng Comput 42: 328-332.
- Bronstein AM, Hood JD, Gresty MA, Panagi C (1990) Visual control of balance in cerebellar and parkinsonian syndromes. Brain 113: 767-779.
- Chong RK, Horak FB, Frank J, Kaye J (1999) Sensory organization for balance: Specific deficits in Alzheimer's but not in Parkinson's disease. J Gerontol A Biol Sci Med Sci 54: M122-M128.
- Chong RK, Jones CL, Horak FB (1999) Postural set for balance control is normal in Alzheimer's but not in Parkinson's disease. J Gerontol A Biol Sci Med Sci 54: M129-M135.
- Chong RK, Horak FB, Woollacott MH (2000) Parkinson's disease impairs the ability to change set quickly. J Neurol Sci 175: 57-70.
- Hacisalihzade SS, Kuster F, Albani C (1986) Computer-aided measuring of motor functions using pursuit tracking. Computer Meth Prog Biomed 23: 19- 28.
- Maurer C, Mergner T, Xie J, Faist M, Pollak P, et al. (2003) Effect of chronic bilateral subthalamic nucleus (STN) stimulation on postural control in Parkinson's disease. Brain 126: 1146-1163.
- Teravainen H, Calne DB (1980) Studies of parkinsonian movement: 1. Programming and execution of eye movements. Acta Neurol Scand 62: 137- 148.
- Packard MG, Knowlton BJ (2002) Learning and memory functions of the basal ganglia. Ann Rev Neurosci 25: 563-593.
- Chong RK, Mills B, Dailey L, Lane E, Smith S, et al. (2010) Specific interference between a cognitive task and sensory organization for stance balance control in healthy young adults: visuospatial effects. Neuropsychologia 48: 2709- 2718.
- Goetz CG, Poewe W, Rascol O, Sampaio C, Stebbins GT, et al. (2004) Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. Mov Disord 19: 1020-1028.
- (2009) GaitAid Virtual Walker
- Movement Disorder Society Task Force on Rating Scales for Parkinson's Disease. (2003) The Unified Parkinson's Disease Rating Scale (UPDRS): status and recommendations. Mov Disord 18: 738-750.
- Chong RK, Morgan J, Mehta SH, Pawlikowska I, Hall P, et al. (2011) Rapid assessment of postural instability in Parkinson's disease (RAPID): A pilot study. Eur J Neurol 18: 260-265.
- Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N (1997) The Parkinson's Disease Questionnaire (PDQ-39): Development and validation of a Parkinson's disease summary index score. Age Ageing 26: 353-357.
- Jenkinson C, Fitzpatrick R (2007) Cross-cultural evaluation of the short form 8-item Parkinson's Disease Questionnaire (PDQ-8): Results from America, Canada, Japan, Italy and Spain. Parkinsonism Relat Disorders 13: 22-28.
- Folstein MF, Folstein SE, McHugh PR (1975) "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. Journal of psychiatric research 12: 189-198.
- Canning CG (2005) The effect of directing attention during walking under dual-task conditions in Parkinson's disease. Parkinsonism Relat Disord 11: 95-99.
- Galletly R, Brauer SG (2005) Does the type of concurrent task affect preferred and cued gait in people with Parkinson's disease? Aust J Physiother 51: 175- 180.
- Bradshaw JL, Waterfall ML, Phillips JG, Iansek R, Mattingley JB, et al. (1993) Re-orientation of attention in Parkinson's disease: an extension to the vibrotactile modality. Neuropsychologia 31: 51-66.
- Brown RG, Marsden CD (1988) Internal versus external cues and the control of attention in Parkinson's disease. Brain 111: 323-345.
- Hsieh S, Lee CY, Tai CT (1995) Set-shifting aptitude in Parkinson's disease: External versus internal cues. Psychol Rep 77: 339-349.
- Wu T, Hallett M (2005) A functional MRI study of automatic movements in patients with Parkinson's disease. Brain 128: 2250-2259.
- Yogev G, Giladi N, Peretz C, Springer S, Simon ES, et al. (2005) Dual tasking, gait rhythmicity, and Parkinson's disease: Which aspects of gait are attention demanding? Eur J Neurosci 22: 1248-1256.
- Chong RK, Horak FB, Woollacott MH (1999) Time-dependent influence of sensorimotor set on automatic responses in perturbed stance. Exp Brain Res 124: 513-519.
- Kaji R (2001) Basal ganglia as a sensory gating devise for motor control. J Med Invest 48: 142-146.
- Page D, Jahanshahi M (2007) Deep brain stimulation of the subthalamic nucleus improves set shifting but does not affect dual task performance in Parkinson's disease. IEEE Trans Neural Syst Rehabil Eng 15: 198-206.
- Tamura I, Kikuchi S, Otsuki M, Kitagawa M, Tashiro K (2003) Deficits of working memory during mental calculation in patients with Parkinson's disease. J Neurol Sci 209: 19-23.
- Morris ME, Iansek R, Matyas TA, Summers JJ (1994) Ability to modulate walking cadence remains intact in Parkinson's disease. J Neurol Neurosurg Psychiatry 57: 1532-1534.
- Rochester L, Hetherington V, Jones D, Nieuwboer A, Willems AM, et al. (2004) Attending to the task: interference effects of functional tasks on walking in Parkinson's disease and the roles of cognition, depression, fatigue, and balance. Arch Phys Med Rehabil 85: 1578-1585.
- Keele SW (1981) Behavioral analysis of movement. In: Brooks V (ed) Handbook of Physiology: Sec. 1: The Nervous System. Williams & Wilkins, Baltimore: MD, 1391-1414.
- Chong RK (2008) Factor analysis of the functional limitations test in healthy individuals. Gait Posture 28: 144-149.
- Mitoma H, Hayashi R, Yanagisawa N, Tsukagoshi H (2000) Characteristics of parkinsonian and ataxic gaits: A study using surface electromyograms, angular displacements and floor reaction forces. J Neurol Sci 174: 22-39.
- Murray MP, Sepic SB, Gardner GM, Downs WJ (1978) Walking patterns of men with parkinsonism. Am J Phys Med 57: 278-294.
- RK, Barbas J, Garrison K, Herolz A, Teheng R, et al. (2001) Does balance control deficit account for walking difficulty in Parkinson's disease? Int J Clin Prac 55: 411-412.
- Morris ME, Iansek R, Matyas TA, Summers JJ (1994) The pathogenesis of gait hypokinesia in Parkinson's disease. Brain 117: 1169-1181.
- Baker K, Rochester L, Nieuwboer A (2007) The immediate effect of attentional, auditory, and a combined cue strategy on gait during single and dual tasks in Parkinson's disease. Arch Phys Med Rehabil 88: 1593-1600.
- Canning CG, Ada L, Johnson JJ, McWhirter S (2006) Walking capacity in mild to moderate Parkinson's disease. Arch Phys Med Rehabil 87: 371-375.
- Cunnington R, Iansek R, Bradshaw JL (1999) Movement-related potentials in Parkinson's disease: external cues and attentional strategies. Mov Disord 14: 63-68.
- Fok P, Farrell M, McMeeken J (2010) Prioritizing gait in dual-task conditions in people with Parkinson's. Hum Mov Sci 29: 831-842.
- TE, Tsai CS, Semmler J, Brophy BP, Thompson PD (1999) Voluntary movement after pallidotomy in severe Parkinson's disease. Brain 122: 895- 906.
- Nieuwboer A, Kwakkel G, Rochester L, Jones D, van Wegen E, et al. (2007) Cueing training in the home improves gait-related mobility in Parkinson's disease: the RESCUE trial. J Neurol Neurosurg Psychiatry 78: 134-140.
- Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, Hillsdale, NJ.
- Bloem BR, Valkenburg VV, Slabbekoorn M, van Dijk JG (2001) The multiple tasks test. Strategies in Parkinson's disease. Exp Brain Res 137: 478-486.
- Brown RG, Marsden CD (1991) Dual task performance and processing resources in normal subjects and patients with Parkinson's disease. Brain 114: 215-231.
- Dujardin K, Degreef JF, Rogelet P, Defebvre L, Destee A (1999) Impairment of the supervisory attentional system in early untreated patients with Parkinson's disease. J Neurol 246: 783-788.
- Marchese R, Bove M, Abbruzzese G (2003) Effect of cognitive and motor tasks on postural stability in Parkinson's disease: a posturographic study. Mov Disord 18: 652-858.
- Morris M, Iansek R, Smithson F, Huxham F (2000) Postural instability in Parkinson's disease: A comparison with and without a concurrent task. Gait Posture 12: 205-216.
- O'Shea S, Morris ME, Iansek R (2002) Dual task interference during gait in people with Parkinson disease: effects of motor versus cognitive secondary tasks. Phys Ther 82: 888-897.
- Kemps E, Szmalec A, Vandierendonck A, Crevits L (2005) Visuo-spatial processing in Parkinson's disease: evidence for diminished visuo-spatial sketch pad and central executive resources. Parkinsonism Relat Disord 11: 181-186.
- Chong RKY, Gibson B, Horton S, Lee A, Mellinger J, et al. (2011) Spatial orientation during eyes closed versus open in the dark: Are they the same? : In review.
- (2011) GaitAid operating instructions.
- Ashburn A, Stack E, Pickering RM, Ward CD (2001) Predicting fallers in a community-based sample of people with Parkinson's disease. Gerontology 47: 277-281.
- Hobson JP, Edwards NI, Meara RJ (2001) The Parkinson's Disease Activities of Daily Living Scale: A new simple and brief subjective measure of disability in Parkinson's disease. Clin Rehabil 15: 241-246.
- Kleiner-Fisman G, Stern MB, Fisman DN (2010) Health-related quality of life in Parkinson disease: correlation between Health Utilities Index III and Unified Parkinson's Disease Rating Scale (UPDRS) in U.S. male veterans. Health Qual Life Outcomes 8: 91.
- GaitAid device (2011)
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 12045
- [From(publication date):
December-2011 - Jul 11, 2025] - Breakdown by view type
- HTML page views : 7336
- PDF downloads : 4709