Clinical Utility of EsoGuard® as a Barrett's Esophagus Triage Test for On-duty Firefighters
Received: 25-Oct-2023 / Manuscript No. JGDS-23-118183 / Editor assigned: 27-Oct-2023 / PreQC No. JGDS-23-118183 (PQ) / Reviewed: 10-Nov-2023 / QC No. JGDS-23-118183 / Revised: 15-Nov-2023 / Manuscript No. JGDS-23-118183 (R) / Published Date: 22-Nov-2023
Abstract
Background: Firefighters have frequent exposure to smoke and compounds shown to increase the risk of esophageal neoplasia. However, many are unaware of their risk for Esophageal Adenocarcinoma (EAC) or the precursor condition Barrett's Esophagus (BE), and screening endoscopy can be difficult to accommodate with shift schedules. The EsoGuard®/EsoCheck® (EG/EC) solution includes a biomarker assay (EsoGuard®/EG) and a non-endoscopic esophageal cell collection device (EsoCheck®/EC), which can be utilized with efficiency and high tolerability as a triage test for BE/EAC.
Methods: This is a retrospective analysis of prospectively collected data on use of the EG/EC solution during two large health fairs for on-duty firefighters in San Antonio, TX, in January 2023.
Results: Firefighters were evaluated by physician volunteers; among those deemed at high risk for BE/EAC, 388 firefighters agreed to EG/EC testing. Over 99% (385/388) successfully provided EC cell samples for analysis, and the EG positivity rate was 7.27% (28/385). Among those who tested EG positive, 100% (28/28) were referred by the ordering physician for confirmatory upper endoscopy. No EG negative subjects were referred for additional testing.
Conclusion: In this initial experience, EG/EC proved to be a rapid, efficient, and well-tolerated test to triage on-duty firefighters at high risk of BE/EAC to endoscopy; EG results demonstrated strong physician decision impact.
Keywords
Barrett’s Esophagus; Firefighters; Esophageal Adenocarcinoma (EAC); Endoscopy; Biomarker test
Introduction
Esophageal Adenocarcinoma (EAC) is the most common cancer of the esophagus in the United States (US), with an incidence that has been increasing over the last 40 years, particularly in white males, for whom the incidence increased more than 6-fold since the 1970’s [1-3]. Despite advances in Chemotherapy, Radiotherapy, and Surgical Therapy, the prognosis for EAC remains poor, with a 5-year survival rate of only 20% [4,5]. Barrett’s Esophagus (BE) is a direct precursor to EAC and contrary to the lethality of EAC, BE can be successfully treated using endoscopic approaches such as radiofrequency or cryotherapy ablation with upwards of 80% success rates [6-8]. As such, published guidelines from the American College of Gastroenterology (ACG) and other Gastroenterological societies recommend BE screening in patients with multiple risk factors [9]. Sadly, most individuals at elevated risk for disease do not undergo screening [10], likely due to barriers of conventional endoscopy including patient fear of complications, perception of invasiveness, and concerns about access issues/scheduling difficulties due to the need for a specialist provider and facility [11]. Most recently, to bridge this gap, non-endoscopic cell collection devices such as EsoCheck® have been developed, and when paired with a biomarker test such as EsoGuard®, have been endorsed by the updated ACG guidelines as a reasonable alternative to conventional Upper Endoscopy (UE) for BE screening [9].
Firefighters, by nature of their occupation have ongoing exposure to multiple known and suspected carcinogenic agents, such as (but not limited to) formaldehyde, benzene, asbestos, and polycyclic aromatic hydrocarbons. As such, in July of 2022, firefighting was designated a Group 1 carcinogen by the International Agency for Research on Cancer (IARC) [12]. Literature has also shown increased cancer mortality in firefighters, including excess incidence of cancers of the digestive tract such as esophageal and colorectal malignancies [13,14]. Given the incremental malignancy risks associated with their occupation, in addition to other traditional risk factors, firefighters could significantly benefit from improved education around BE/EAC and increased screening.
We present data from an initial experience using the EsoGuard/EsoCheck (EG/EC) solution in testing several hundred on-duty San Antonio firefighters during two health fairs in January 2023. To our knowledge, this was the first experience of any large-scale screening for BE/EAC in U.S firefighters to date.
Materials And Methods
Population
Two large health fairs for firefighters were organized by over 40 community volunteers, including community physicians and other health care professionals, and the San Antonio Fire Department in January of 2023. The events occurred over the course of two weekends (January 14-15, and January 28-29) and focused on skin cancer and BE/EAC screening. Resources and support were also provided by Mollie’s Fund (Mollie Biggane Melanoma Foundation) for skin cancer screening, and Lucid Diagnostics Inc. (Barrett’s Esophagus and esophageal adenocarcinoma screening) provided EC device administrators for the BE/EAC screening. Only individuals identified by a physician as being high-risk for BE/EAC underwent EG/EC testing. The evaluating physician was an individual familiar with current guidelines and made the clinical decision to test/ not test individuals independently of external and/or industry influences.
Ethical Considerations
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the WCG Institutional Review Board (study number 1350589, approved on 03-March-23). Given the retrospective nature of the analysis, limited extent of health information being collected, and satisfactory plan for protecting patient identifiers from improper use and disclosure, patient informed consent was waived.
EsoCheck® and EsoGuard®
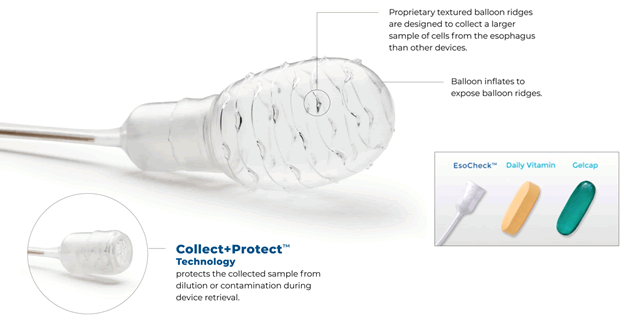
EsoCheck® (EC) is an FDA cleared, non-endoscopic cell collection device (Figure 1) designed to circumferentially sample cells from a targeted region of the esophagus (Figure 2); EsoGuard® (EG) is a Laboratory Developed Test (LDT) performed in a Clinical Laboratory Improvement Amendment (CLIA) certified and College of American Pathologists (CAP) accredited lab that utilizes a set of genetic assays and algorithms which examines the presence of cytosine methylation at 31 different genomic locations on the vimentin (VIM) and Cyclin-A1 (CCNA1) genes. EsoGuard has been clinically validated in a developmental study published in 2018 and shown to have a >90% sensitivity and >90% specificity in detection of disease along the full BE to EAC progression spectrum [15].
EsoCheck administration is a simple, non-invasive, non-endoscopic, office-based procedure that can be performed by a variety of healthcare providers including physicians, nurse practitioners, physician assistants, nurses, or other trained personnel usually in less than 5 minutes and without sedation or significant pre-procedure preparation.
Non endoscopic cell-collection devices paired with a biomarker test (e.g., EsoCheck/EsoGuard) are deemed an acceptable alternative to UE to screen for BE, according to the 2022 ACG guidelines for screening of Barrett’s Esophagus [9].
Testing and Follow-up from the San Antonio Firefighter Health Fairs
Firefighters deemed by the evaluating physician as appropriate for EG/ EC screening were educated about BE/EAC, risk factors, and the EG/ EC solution; after appropriate counseling they were given the option to undergo testing. Patients identified to have concerning symptoms such as dysphagia, or escalation of pre-existing symptoms were automatically referred for diagnostic upper endoscopy rather than screening. The EC cell collections were performed by Lucid personnel who are trained and certified according to the Laboratory’s Standard Operating Procedures (SOPs), and in accordance with the device Instructions for Use (IFU). Samples were then sent to the Central Lab for analysis (LucidDx Labs, Inc, Lake Forest, California). EG results were available within two weeks of cell collection and sent directly to the ordering physician. The physician then made an independent determination of the next step(s) in patient management and conveyed both the test results and management plan to the patient.
Data Collection and Statistical Analysis
This is a retrospective analysis of prospectively collected data. Given the nature of the health fairs (staffed by volunteers and located on-site at the firefighter training academy), only a limited data set was collected and reviewed due to the absence of Electronic Medical Record (EMR) documentation; this consisted of patient demographic information, EG test results, and physician referral patterns. All data was compiled in an Excel file. No statistical software was utilized for data analysis, and calculations were performed with Excel. The results for continuous variables are shown as medians with Interquartile Range (IQR). Categorical variables are presented as counts and percentages. No comparative tests were performed.
Results
Over both weekends, a total of 388 San Antonio firefighters were sent for EG/EC testing by the physician leading the health events. An overview of basic patient characteristics is provided in Table 1. The rate of successful EC cell collection was 99.22% (385/388). Males accounted for 92.99% (358/385) of the tested population, and median age was 41.49 years old [IQR 14.45].
Table 1: Testing numbers and patient characteristics
| Characteristic | n | % | |
|---|---|---|---|
| Firefighters participating in EsoCheck/EsoGuard BE/EAC screening | 388 | 100 | |
| Firefighters unable to swallow EsoCheck (i.e., unable to provide cell samples for EsoGuard) | 3 | 0.1 | |
| Firefighters who successfully swallowed EsoCheck | 385 | 99.2 | |
| Full Analysis Cohort | 385 | ||
| Median age (years) | 41.5 | IQR: 14.5 | Min, max: 21.6, 77.5 |
| Cohort by sex | n | % | |
| Male | 358 | 93.0 | |
| Median age (years) | 41.5 | IQR: 14.5 | Min, max: 21.6, 77.5 |
| Female | 27 | 7.0 | |
| Median age (years) | 42.3 | IQR: 12.7 | Min, max: 29.6, 63.9 |
The successful EG analysis rate was 96.62% (372/385), meaning 372 of the 385 cell samples sent to the lab had binary EG results (positive or negative). Only 13 cell samples (3.37%) had DNA ‘quantity not sufficient’ (QNS) to complete EG analysis. A total of 28 patients tested positive (7.27%), and 344 patients tested negative (89.35%); (Table 2). Among those who tested EG positive, 100% (28/28) were referred by the ordering physician for confirmatory upper endoscopy. No EG negative subjects were referred for additional testing.
Table 2: EsoGuard® results
| EG Result | n | % |
|---|---|---|
| Total | 385 | 100% |
| Positive | 28 | 7.3 |
| Male | 26 | 92.9 |
| Female | 2 | 7.1 |
| Negative | 344 | 89.4 |
| Male | 319 | 92.7 |
| Female | 25 | 7.3 |
| DNA Quantity Not Sufficient (QNS) | 13 | 3.4 |
| Male | 13 | 100.0 |
| Female | 0 | 0 |
Among the EG (+) firefighters, two (7.14%) were female and the remainder were male. All QNS results were from males. When the EsoGuard (+) results are analyzed based on characteristics of patient sex and age (Table 3), it was noted that the EG (+) rate was similar among females and males, at 7.41% and 7.26%, respectively. However, the sample size of females is too small to draw statistical conclusions.
Table 3: EsoGuard® positive results by age and sex
| Characteristic | n EsoGuard (+) | Total n | Positive rate (%) |
|---|---|---|---|
| Male sex | 26 | 358 | 7.3 |
| Female sex | 2 | 27 | 7.4 |
| Age<30 years | 0 | 37 | 0 |
| Age<50 years | 15 | 295 | 5.1 |
| Age 50 years or greater | 13 | 90 | 14.4 |
| Age 70 years of greater | 3 | 6 | 50 |
Discussion
One of the earliest suggestions of an association between firefighters and esophageal malignancy arose from a registry-based case-control study published in 2007. Based on records of 3,659 California firefighters, there was evidence that firefighting could be a risk factor for esophageal cancer, with an odds ratio of 1.48 (95% CI 1.14- 1.91) [16]. In a pooled cohort of U.S firefighters from San Francisco, Chicago, and Philadelphia, evaluating mortality and cancer incidence from 1950 to 2009 (later with updated mortality data through 2016), the standardized mortality ratio (ratio of observed to expected number of deaths) was 1.31-1.39 for esophageal cancer; the standardized incidence ratio (ratio of observed malignancies to the expected number of cases estimated using U.S incidence rates) was 1.62 [13,14]. Similar results were found by the National Institute for Occupational Safety and Health (NIOSH) in their study of California firefighters from 1988-2007 with an odds ratio of 1.6 for esophageal cancer [17]. In Western countries, the most common type of esophageal cancer is EAC, which is known to arise from the pre-malignant condition of BE [18].
We present an initial experience with a non-endoscopic cell collection device (EsoCheck) paired with a biomarker test (EsoGuard) for BE/EAC screening within a high-risk firefighter population. In the commercial setting the EG/EC solution is utilized as a triage test to aid physicians in identifying individuals who would warrant more invasive, endoscopic work-up for BE/EAC. The solution was designed to bridge the known diagnostic gap of numerous high-risk individuals who don’t undergo recommended ‘traditional’ screening evaluations [10]. Given the 90% sensitivity and specificity of EG for detection of disease along the full BE to EAC spectrum, a negative EG result indicates a low probability of disease and may serve as a better-tolerated alternative to screening endoscopy for ‘ruling out’ individuals [15]. This is supported by findings from the San Antonio health fairs, as no EG negative firefighters were referred by the physician for additional endoscopic workup. In contrast, all 28 EG positive firefighters were referred to an endoscopist for confirmatory evaluation.
EC was successfully swallowed in >99% of patients with no complications reported, suggesting excellent tolerability. All firefighters were able to immediately return to their shifts following the EC cell collection, as the absence of sedation meant no post-procedure observation period was required. The observed EG positivity rate of 7.27% is also consistent with BE prevalence rates from the literature (5-15%) [19]. As seen in this firefighter screening experience, EC can be administered to many patients (nearly 400 firefighters over only four days) in an efficient and welltolerated fashion.
This study was also not intended to validate the EG assay performance, but rather to demonstrate the clinical utility of the EG/EC solution as a triage test to endoscopy for detection of BE/EAC. Our experience demonstrates the EG/EC solution can be readily implemented in even non-traditional (i.e., non-office) settings like health fairs, and rapidly executed for busy individuals like on-duty firefighters. Future directions for study would include evaluation of an even larger and geographically diverse population of firefighters, more comprehensive collection of individual risk factors, and longitudinal follow-up which could be powered for subgroup analysis.
Conclusion
We present the largest experience to date of BE/EAC screening in on-duty firefighters. This was done by utilizing EG/EC, a non-endoscopic solution, to triage high-risk individuals to upper endoscopy. This enabled effective and efficient management of nearly 400 firefighters who might otherwise not have been screened. Overall, the test was well tolerated, had high result yield, and effectively drove physician management decisions.
Author Contributions
Hamblin R, Lee VT, DeGuzman BJ, Verma S, and Aklog L conceived and designed this project. Hamblin R collected the data. Hamblin R and Lee VT analyzed and interpreted the data. Hamblin R and Lee VT wrote the first draft of the manuscript. Hamblin R, Lee VT, DeGuzman BJ, Verma S, and Aklog L reviewed and edited the manuscript.
Acknowledgement
None.
Conflicts of Interest
Hamblin R declares no conflict of interest. Lee VT, DeGuzman BJ, and Aklog L, are executive members of PAVmed Inc., of which Lucid Diagnostics Inc. is a subsidiary, and owns stock and/or options in the parent company. Verma S is an executive member of Lucid Diagnostics Inc. and owns stock and/or options in the company.
Funding
This project received no external funding. EsoCheck cell collections performed by Lucid Diagnostics personnel are a standard, optional service provided to customers in the commercial setting.
References
- Pohl H, Welch HG (2005) The role of overdiagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst 97(2): 142-146.
- Devesa SS, Blot WJ, Fraumeni JF (1998) Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer 83(10): 2049-2053.
- Pera M, Cameron AJ, Trastek VF, Carpenter HA, Zinsmeister AR (1993) Increasing incidence of adenocarcinoma of the esophagus and esophagogastric junction. Gastroenterology 104(2): 510-513.
- National Cancer Institute: Surveillance, e., and end results program. esophageal cancer-cancer stat facts. (2023).
- Siegel RL, Miller KD, Jemal A (2015) Cancer statistics, 2015. CA Cancer J Clin 65(1): 5-29.
- Stawinski PM, Dziadkowiec KN, Kuo LA, Echavarria J, Saligram S (2023) Barrett's esophagus: An updated review. Diagnostics 13(2): 321.
- Rastogi A, Puli S, El-Serag HB, Bansal A, Wani S, et al. (2008) Incidence of esophageal adenocarcinoma in patients with Barrett's esophagus and high-grade dysplasia: A meta-analysis. Gastrointest Endosc 67(3): 394-398.
- Phoa KN, Vilsteren FG, Weusten BL, Bisschops R, Schoon EJ, et al. (2014) Radiofrequency ablation vs endoscopic surveillance for patients with Barrett esophagus and low-grade dysplasia: A randomized clinical trial. Jama 311(12): 1209-1217.
- Shaheen NJ, Falk GW, Iyer PG, Souza RF, Yadlapati RH, et al. (2022) Diagnosis and management of barrett's esophagus: An updated ACG guideline. Am J Gastroenterol 117(4): 559-587.
- Vaughan TL, Fitzgerald RC (2015) Precision prevention of oesophageal adenocarcinoma. Nat Rev Gastroenterol Hepatol 12(4): 243-248.
- Kolb JM, Mindy C, Anna T, Jazmyne G, Jazmyne O, et al. (2023) Patient knowledge, risk perception, and barriers to Barrett's esophagus screening. Am J Gastroenterol 118(4): 615-626.
- Demers PA, DeMarini DM, Fent KW, Glass DC, Hansen J, et al. (2022) Carcinogenicity of occupational exposure as a firefighter. Lancet Oncol 23(8): 985-986.
- Daniels RD, Kubale TL, Yiin JH, Dahm MM, Hales TR, et al. (2014) Mortality and cancer incidence in a pooled cohort of US firefighters from San Francisco, Chicago and Philadelphia (1950-2009). Occup Environ Med 71(6): 388-397.
- Pinkerton L, Bertke SJ, Yiin J, Dahm M, Kubale T, et al. (2020) Mortality in a cohort of US firefighters from San Francisco, Chicago and Philadelphia: An update. Occup Environ Med 77(2): 84-93.
- Moinova HR, Lutterbaugh JD, Chandar AK, Dumot J, Faulx A, et al. (2018) Identifying DNA methylation biomarkers for non-endoscopic detection of Barrett's esophagus. Sci Transl Med 10(424): 1-11.
- Bates MN (2007) Registry-based case-control study of cancer in California firefighters. Am J Ind Med 50(5): 339-344.
- Tsai RJ, Luckhaupt SE, Schumacher P, Cress RD, Deapen DM, et al. (2015) Risk of cancer among firefighters in California, 1988-2007. Am J Ind Med 58(7): 715-729.
- Delforge M, Plomteux O, Delfosse V, Fontaine F, Louis E, et al. (2002) Barrett's esophagus: Overview. Rev Med Liege 57(8): 535-545.
- Runge TM, Abrams JA, Shaheen NJ (2015) Epidemiology of Barrett's esophagus and esophageal adenocarcinoma. Gastroenterol Clin North Am 44(2): 203-231.
Citation: Hamblin R, Lee VT, DeGuzman BJ, Verma S, Aklog L (2023) Clinical Utility of EsoGuard® as a Barrettâs Esophagus Triage Test for On-duty Firefighters. J Gastrointest Dig Syst 13: 764.
Copyright: © 2023 Hamblin R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2785
- [From(publication date): 0-2023 - Nov 24, 2025]
- Breakdown by view type
- HTML page views: 2434
- PDF downloads: 351