Case Report Open Access
Clinical Outcomes of Grade 3 Giant Cell Tumor of Bone After Extended Intralesional Curettage
Sukpanichyingyong S*and Sangkomkamhang TDepartment of Orthopedics, Khon Kaen Hospital, Khon Kaen, Thailand, 54, 56 Srichan Road, Mueang Khon Kaen-40000, Thailand
- *Corresponding Author:
- Sukpanichyingyong Scorr
Department of Orthopedics, Khon Kaen Hospital
Khon Kaen, Thailand, 54, 56 Srichan road
Mueang Khon Kaen- 40000, Thailand
Tel: (+66)866300280
E-mail: Sermsak.su@cpird.in.th
Received date: June 01, 2016; Accepted date: May 31, 2017; Published date: June 07, 2017
Citation: Sukpanichyingyong S, Sangkomkamhang T (2017) Clinical Outcomes of Grade 3 Giant Cell Tumor of Bone After Extended Intralesional Curettage. J Orthop Oncol 3:118. doi: 10.4172/2472-016X.1000118
Copyright: © 2017 Sukpanichyingyong S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Orthopedic Oncology
Abstract
Introduction: The recommended treatment of grade 3 giant cell tumor of bone (grade 3 GCTB) aims to eliminate tumor and conserve limb with extended intralesional curettage. This treatment makes patients better function of bone and joint as usual. Even it can reduce postoperative complications and replace endoprosthesis. Still, there is limited information about the outcomes of surgical treatment and recurrence of the disease. This study aimed to evaluate the clinical outcomes and recurrence of grade 3 GCTB with extended intralesional curettage. Case Description: This study performed a retrospective review of 26 consecutive patients with grade 3 GCTB treated by extended intralesional curettage at Khon Kaen hospital from June 2012 to May 2017. Clinical outcomes including, functional analysis according to Musculoskeletal Tumor Society functional classification (MSTS score), pain score, postoperative complication and recurrence rate were evaluated. Twenty out of twenty-six patients were motion as usual within 6 months after surgery while recurrence of the disease is shown only one case. However, postoperative complications have not yet been reported. Conclusion: The extended intralesional curettage of grade 3 GCTB grade is an effective treatment. Nevertheless, it have to keep recall the patient for detection of disease recurrence.
Introduction
The giant cell tumor of bone (GCTB) was described by Cooper and Travers in 1818 [1]. It is considered a locally aggressive benign bone tumor with tendency for high recurrence. GCTB represents approximately 5-10% of all primary bone tumors [2-4]. It typically occurs in 30-40 years of age and is slightly more common in female [4], also is higher incidence rate in Southeast Asia than Western [4,5]. The most common GCTB is involved in the epiphyseal regions of long bones, particularly the distal femur and the proximal tibia [6,7]. Primary malignant turn and distant lung metastasis are about 1% and 3% in GCTB patients, respectively [8].
The principal symptoms are pain and swelling which are caused by cortical bone destruction and tumor expansion. Addition, joint effusion and limited range of motion are also possible. Pathological fracture shows aggressive progression of disease. The definitive diagnosis is confirmed by histological method. This benign tumor has characteristic multinucleated osteoclast-type giant cells [9].
There is still not a consensus in surgical treatment of grade 3 GCTB between a wide excision and an extended intralesional excision which it is all about balance between eliminating the tumor and preserving the extremity’s function [10-12]. This study assesses the functional and oncological outcomes grade 3 GCTB with an extended intralesional curettage combined with adjuvant therapies comprising high-speed burring and bone cementation, instead of a wide excision, to better avoid limb salvage surgery with endoprosthetic reconstruction.
Methods
The study is a retrospective descriptive study of the clinical outcomes in grade 3 GCTB treated by extended intralesional curettage at Khon Kaen hospital, Thailand from June 2012 to May 2017. All patients with histologically and staging verified grade 3 GCTB underwent extended intralesional curettage followed by high-speed burring in some cases used of phenol. The resultant intraosseous defects were reconstructed with polymethylmethacrylate bone cement because not only provides immediate stability but also help detect local recurrence from postoperative radiograph. Addition, some patients with impending or actual pathological fractures managed with plate fixation. Patients were admitted for 5 to 10 days deciding by size and site of GCTB. The patients with the upper extremity were managed with a sling for 2 to 4 weeks postoperatively, while the lower extremities, patients were either non-weight-bearing or partial weight-bearing for 4 to 6 weeks and used crutches when they walked. Patients were followed by means of physical examination, radiographs of the extremity (to rule out local recurrence) and on the chest (to rule out lung metastasis) every 6 months from 1 to 2 years, and annually after that [8]. The clinical outcome assessment was performed using the Musculoskeletal Tumor Society (MSTS) scoring system for the upper and lower limbs. The radiographic evidence of endosteal scalloping or cortical erosion, tumor size, tumor location and soft tissue extension on MRI and patient age affect successfully treatment. The outcomes included the MSTS score, pain score, local recurrence and tumor metastasis.
Results
Oncological outcomes
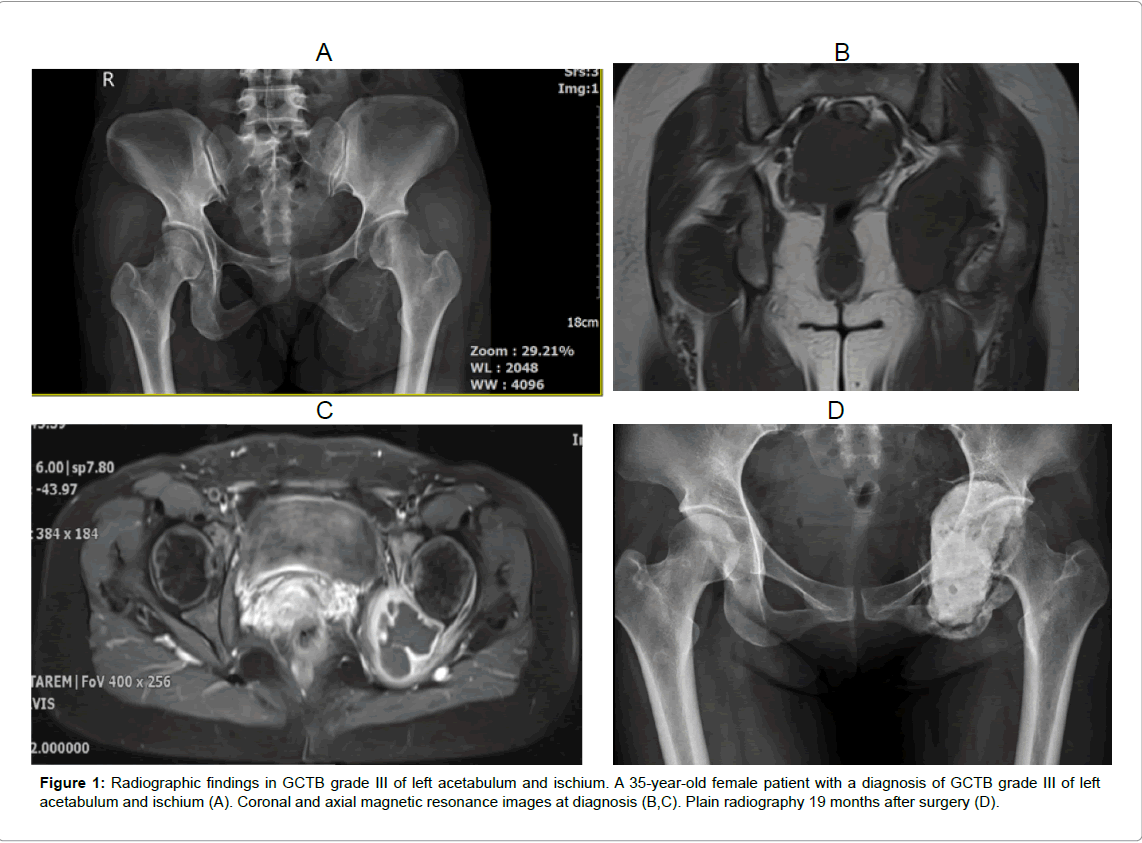
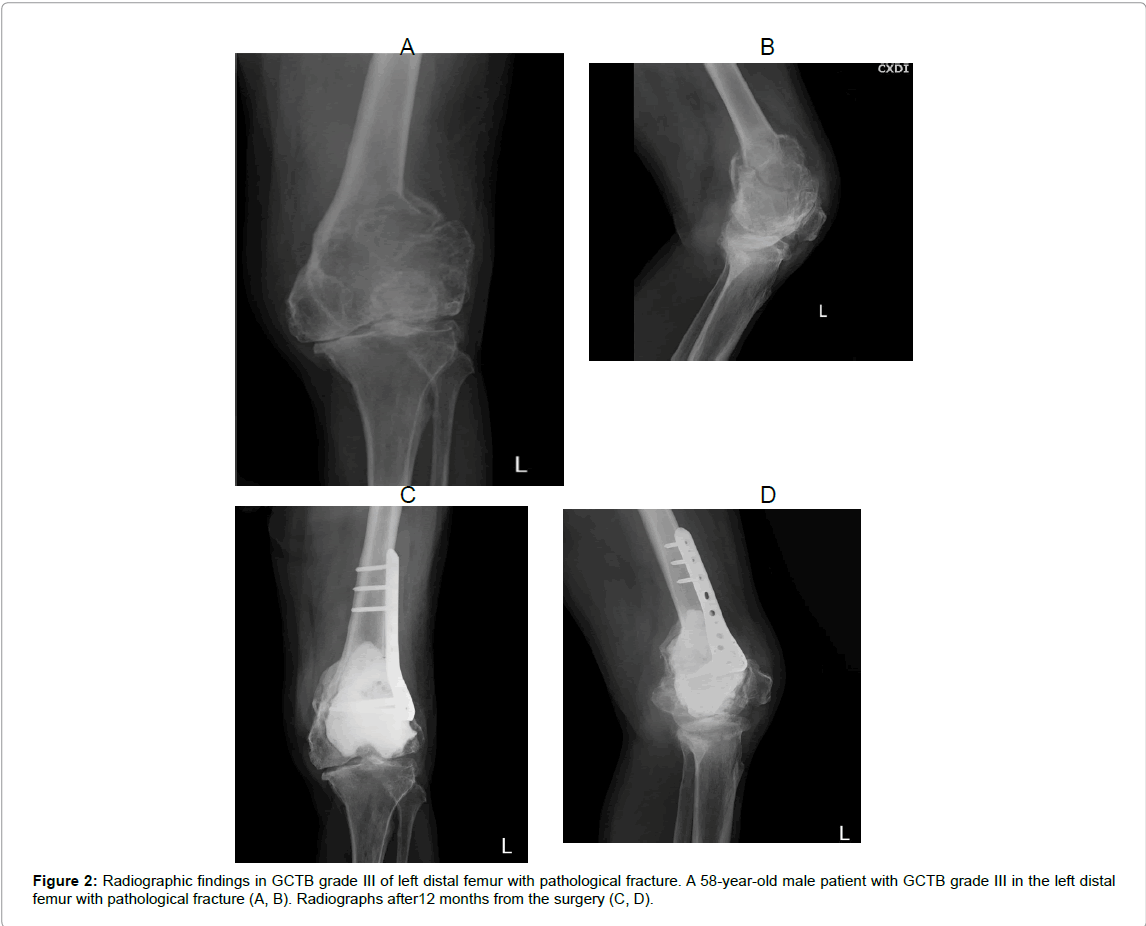
The average age of patients was 35 (range; 14 to 67) years. There were 14 male and 12 female patients. All of them do not have the family health history of cancer. The treated lesions were located in the distal femur (n=9), proximal tibia (n=6), proximal femur (n=2), distal ulnar (n=2), calcaneus (n=2) and also in ischium and acetabulum, distal radius, distal fibula, proximal humerus and distal tibia (n=1). Seven of them (26.92%) had a pathological fracture in the tumor area. All patients, who were diagnosed with GCTB, were staged according to the radiograph described by Campanacci grading system [13,14]. The mean follow-up time was 36.8 (range; 12 to 58) months after surgery (Figures 1 and 2).
Histological findings
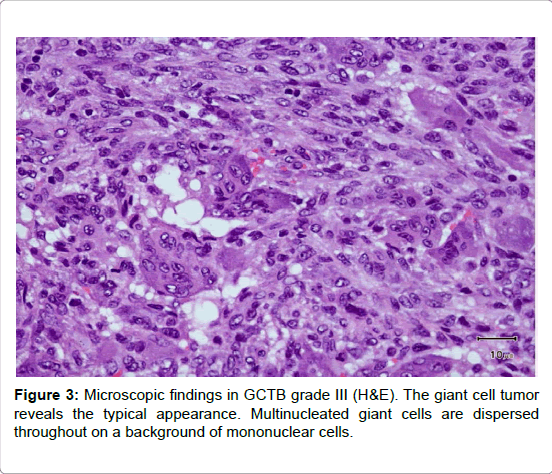
All patients were histologically verified with GCTB. Multinucleated giant cells are dispersed throughout on a background of mononuclear cells. They reveal prominent mitotic activity and rare cellular atypia. Also, they have numerous centrally located nuclei as opposed to the peripherally located nuclei of Langerhans-type giant cells seen in atypical infections. The nuclei tend to be compact and oval and contain prominent nucleoli. These are similar in appearance to those of the surrounding stromal cells, and the giant cell often appears to be a syncytium of these stromal cells (Figure 3 and Table 1).
| Patient | Sex | Age | Location | Pathological fracture | Follow-up (month) |
MSTS score (%) |
|---|---|---|---|---|---|---|
| 1 | Male | 49 | Distal femur | No | 58 | 90 |
| 2 | Male | 28 | Distal ulnar | No | 57 | 96.66 |
| 3 | Male | 50 | Proximal tibia | No | 57 | 76.66 |
| 4 | Female | 29 | Proximal femur | Yes | 52 | 90.00 |
| 5 | Male | 67 | Proximal tibia | No | 50 | 90 |
| 6 | Male | 31 | Proximal femur | No | 49 | 96.66 |
| 7 | Male | 27 | Distal radius | No | 44 | 90.00 |
| 8 | Female | 18 | Distal femur | Yes | 44 | 93.33 |
| 9 | Male | 14 | Distal fibula | No | 42 | 96.66 |
| 10 | Male | 22 | Distal femur | No | 41 | 86.66 |
| 11 | Male | 44 | Proximal tibia | No | 41 | 100 |
| 12 | Female | 30 | Distal femur | No | 40 | 100 |
| 13 | Male | 37 | Proximal tibia | No | 40 | 90 |
| 14 | Female | 49 | Proximal humerus | No | 39 | 46.66 |
| 15 | Male | 25 | Calcaneus | Yes | 36 | 93.33 |
| 16 | Female | 41 | Distal ulnar | No | 34 | 90 |
| 17 | Female | 23 | Distal femur | No | 30 | 93.33 |
| 18 | Male | 29 | Calcaneus | Yes | 29 | 100 |
| 19* | Male | 58 | Distal femur | Yes | 27 | 83.33 |
| 20 | Female | 35 | Ischium and acetabulum | No | 27 | 86.66 |
| 21 | Female | 17 | Distal femur | Yes | 24 | 90 |
| 22 | Female | 14 | Proximal tibia | No | 17 | 93.33 |
| 23 | Male | 19 | Distal femur | No | 12 | 93.33 |
| 24 | Female | 41 | Distal tibia | No | 12 | 86.66 |
| 25 | Female | 54 | Proximal tibia | No | 12 | 86.66 |
| 26 | Female | 37 | Distal femur | Yes | 12 | 83.33 |
Table1: Characteristics of the Patients.
Functional outcomes
The average MSTS score in all 26 patients at last follow-up was 89.36% (46.66% to 100%). The mean MSTS scores for the upper limb score were 81.99% (46.66% to 96.66%), whereas the mean MSTS scores for lower limb were 91.06% (76.66% to 100%). All patients were able to perform activities in their daily living and occupation. Six patients reported level of slight pain in the operation site after 12 months. There were no complications like fracture, infection or thermal injury to the skin.
Recurrence
One patient (3.84%) had developed local recurrence of the distal femur in 7 months of follow-up time postoperatively, which was resolved by re-extended intralesional curettage. Nonetheless, metastasis in GCTB occurs most commonly in the lung. All patients had chest X-ray for investigation annually, but there was no pulmonary metastasis or mortality in this study.
Discussion
Demography
The GCT accounts for 5% of all tumors. There is a high prevalence about 20% in Southern East and Southern India [13]. Although most studies have reported an increased prevalence among females, our study has shown an equal gender distribution. The three most common sites are the distal femur, proximal tibia, and proximal femur, respectively. At diagnosis, 12% of patients with GCT present with a pathological fracture [15]. However, our study has reported up to 26.92% of patients.
Treatment
Many treatment options of GCT of bone are intralesional curettage, extended intralesional curettage which either alone or combined with local adjuvant treatments, marginal resection, and en bloc resection with biologic or endoprosthetic reconstruction. However, the recurrence rates of only intralesional curettage have been relatively high, ranging from 25% to 50% [16-18,19-21]. The addition of mechanical burr drilling of the wall of the tumor and adjuvant substances have decreased the recurrence rate to as low as 6-25% for primary treatment [22]. The decision depends on the severity of the tumor extent, site of tumor, functional and morbidity [16-18]. Previously, the grade 3 GCTB is often treated with wide excision achieved by either amputation or resection of the tumor with limb salvage reconstruction [19]. Gupta et al. performed a retrospective review of 93 consecutive patients which showed there was a difference in the local recurrence rate among patients treated with intralesional resection and those treated with wide resection. 19 of 54 treated by curettage and bone grafting showed a recurrence [20]. The main reasons for the poor results of curettage and bone grafting in extensive lesions were tumor recurrence and joint surface collapse.
However, wide resection in young patient seems disproportionate because of insubstantial functional morbidity.
Recently, grade 3 GCTB approaches, which an extended curettage technique, is the edge of curettage and wide excision. It is obscure disadvantages of both. Asavamongkolkul et al. performed a study involving 30 patients treated with extended intralesional curettage and 24 patients treated with wide excision for grade 3 GCTB; no significant differences in local recurrence or metastasis were found between the two methods. The mean follow up-time was 59 months. Also, The functional analysis was excellence in the extended curettage group (94 percent) and good in wide excision group (77.6 percent) [13].
Likewise, Hsien-Chung Wang et al. study of 24 patients in 1983 to 2001. Twenty-four patients treated with extended intralesional curettage and 10 patients treated with wide excision for grade 3 GCTB. The mean follow up-time was 7.5 years (range: 2.1-20.3 years). In the extended curettage group, two patients had local recurrence. None of ten patients receiving wide excision had experienced local recurrence. Though, it has not reported clinically significant differences in both groups [24]. The average MSTS score at last follow-up was 84-93% [23]. In our study, it was 89.36%. Many studies have shown extended intralesional curettage to be an acceptable treatment in grade 3 GCT of bone because it avoids the morbidity associated with the more radical surgical procedures [11,13-15]. This study was limited by its observational and retrospective design and relatively small number of patients. We did not use a control group to compare the results. The ideal situation would be to perform a prospective, multicenter, randomized control trial. However, this study supports the aspect that extended intralesional curettage plus highspeed burring and cementation is an effective treatment strategy for grade 3 GCTB, with excellent oncological and functional results
Medicine
Recently, denosumab and bisphosphonates have been approved to treat GCTB. The new chemotherapeutic drug denosumab is a monoclonal antibody that targets the receptor activator of nuclear factor κ-B ligand and stops the osteoclastic activity of cells in GCT [24]. Bisphosphonates has anti osteoclastic effect which not only reduce the osteoclast-like behavior of GCT of bone, but also dismantle it physiology and reduce its vascularity [25]. In Tse et al. study, comparing local recurrence of the bisphosphonate treated group and control group developed 4.2% and 30%, respectively. The difference in the recurrence rate was statistically significant between the bisphosphonate treatment group and the control group (Log Rank test p=0.056). The effect of reduction of local recurrence was significant in patients with grade 3 diseases. Patients treated with bisphosphonate did not report any untoward effects [26]. In our study, we only prescribed the bisphosphonates to patient who hard to completely surgical approach such as ischium and acetabulum case.
Radiation
This study, radiotherapy is recommended which in impractical completely excision or curettage for medical or functional reasons, like lesions of the spine and sacrum or for aggressive tumors.
Recurrence
The overall recurrence-free survival at years 1, 2, and 3 were 86%, 79%, and 72%, respectively. Recurrence did not correlate with patient age (p=0.20), primary or recurrent tumor at presentation (p=0.12), Campanacci grade (p=0.10), Enneking stage (p=0.54), or presence of pathological fracture (p=0.28) [27,28]. We have recall system for early detection of recurrence by physical examination, radiographs of the extremity (to rule out local recurrence) and on the chest (to rule out lung metastasis) every 6 months from 1 to 2 years, and annually. Unfortunately, we found one case with local recurrence on the distal femur within 7 months after surgery.
Lung metastases have been reported in 1%–6% of cases. These lesions are thought to arise from hematogenous seeding of GCTB [29]. The interval within the occurrence of pulmonary metastasis can be as little as several months or more than 10 years. However, in most cases metastases were found within 3 years after the surgical treatment of the initial lesion [30,31]. In addition, malignancy in GCT has reported approximately 2% of all cases, which ratio M: F equal 3:1 [32].
Conclusion
The treatment outcomes of extended intralesional curettage in grade 3 GCTB showed a safe and efficient technique. We propose this limb-preservative treatment option as the first choice more radical procedures because it makes better function, has low morbidity, is costeffective, and appear less adverse effect on outcomes.
References
- Cooper AS, Travers B (1818) Surgical essays. London, England: Cox Longman & Co, 178-179.
- Li D, Zhang J, Li Y, Xia J, Yang Y, et al. (2016) Surgery methods and soft tissue extension are the potential risk factors of local recurrence in giant cell tumor of bone. World Journal of Surgical Oncology 14: 114-119.
- Chanchairujira K, Jiranantanakorn T, Phimolsarnti R, Asavamongkolkul A, Waikakul S (2011) Factors of local recurrence of giant cell tumor of long bone after treatment: plain radiographs, pathology and surgical procedures. Journal of the Medical Association of Thailand 94: 1230-1237.
- Arbeitsgemeinschaft K, Becker WT, Dohle J, Bernd L, Braun A, et al. (2008) Local recurrence of giant cell tumor of bone after intralesional treatment with and without adjuvant therapy. The Journal of Bone and Joint Surgery American volume 90: 1060-1067.
- Lim YW, Tan MH (2005) Treatment of benign giant cell tumours of bone in Singapore. Ann Acad Med Singapore 34: 235-237.
- Balke M, Schremper L, Gebert C, Ahrens H, Streitbuerger A, et al. (2008) Giant cell tumor of bone: Treatment and outcome of 214 cases. J Cancer Res ClinOncol 134: 969-978.
- Blackley HR, Wunder JS, Davis AM, White LM, Kandel R, et al. (1999) Treatment of giant-cell tumors of long bones with curettage and bone-grafting. J Bone Joint Surg Am 81: 811-820.
- Aikeremujiang M, Xiaohui N (2014) Pulmonary metastasis of giant cell tumor of bones. World Journal of Surgical Oncology 12: 261-270.
- Yip KM, Leung PC, Kumta SM (1996) Giant cell tumor of bone. ClinOrthopRelat Res 323: 60-80.
- Amanatullah DF, Clark TR, Lopez MJ, Borys D, Tamurian RM (2014) Giant cell tumor of bone. Orthopedics 37: 112-120.
- Li X, Guo W, Yang Y, Wei R, Du ZY (2013) Surgical treatment for long bone giant cell tumor of extremity with pathologic fracture. Beijing da xuexuebao Yi xue ban. Journal of Peking University Health sciences 45: 745-751.
- Puthoor DK, Puthezhath K (2012) Management of giant cell tumor of bone: computerized tomography based selection strategy and approaching the lesion through the site of cortical break. OrthopaedicSurgery 4: 76-82.
- Asavamongkolkul A, Eamsobhana P, Waikakul S, Phimolsarnti R (2012) The outcomes of treatment of giant cell tumor of bone around the knee. Journal of the Medical Association of Thailand.Chotmaihetthangphaet 95 Suppl 9: S122-128.
- Campanacci M, Baldini N, Boriani S, Sudanese A (1987) Outcomes of Orthopedics. J Bone Joint Surg Am 69: 106-114.
- Sobti A, Agrawal P, Agarwala S, Agarwal M (2016) Giant Cell Tumor of Bone - An Overview. Arch Bone JtSurg 4: 2-9.
- Kamer S, Anacak Y, Savas R, Doganavsargil B, Haydaroglu A (2006) Giant cell tumor of the bone with an asymptomatic huge solitary lung metastasis; case presentation and literature review. Journal of BUON :official. Journal of TheBalkan Union of Oncology 11: 87-90.
- Amanatullah DF, Clark TR, Lopez MJ, Borys D, Tamurian RM (2014) Giant cell tumor of bone. Orthopedics 37: 112-120.
- Puthoor DK, Puthezhath K (2012) Management of giant cell tumor of bone: computerized tomography based selection strategy and approaching the lesion through the site of cortical break. OrthopaedicSurgery 4: 76-82.
- Dunham WK, Calhoun JC (1985) The surgical treatment of giant cell tumor of bone. The Alabama Journal of Medical Sciences 22: 258-265.
- Gupta A, Nath R, Mishra M (2007) Giant cell tumor of bone: Multimodal approach. Indian Journal of Orthopaedics 41: 115-120.
- Balke M, Schremper L, Gebert C, et al. (2008) Giant cell tumor of bone: treatment and outcome of 214 cases. J Cancer Res ClinOncol 134: 969-978.
- Malawer MM, Bickels J, Meller I, Buch RG, Henshaw RM, (1999) Cryosurgery in the treatment of giant cell tumor: a long-term follow up study. ClinOrthopRelat Res 359: 176-188.
- Wang HC, Chien SH, Lin GT (2005) Management of grade III giant cell tumors of bones. Journal of Surgical Oncology 92: 46-51.
- Nishisho T, Hanaoka N, Miyagi R, Sakai T, Toki S, et al. (2015) Local administration of zoledronic acid for giant cell tumor of bone. Orthopedics 38: e25-30.
- Tse LF. Wong KC, Kumta SM (2008) Bisphosphonates reduce local recurrence in extremity giant cell tumor of bone: A case-control study Bone 42: 68
- Mashfiqul A, Chusheng S, Hong Tan M (2014) Risk Factors for Recurrence of Giant Cell Tumors of Bone. J OrthopSurg (Hong Kong) 22: 108-113.
- Okamoto Y, Mathew S, Daw NC (2003) Giant cell tumor of bone with pulmonary metastases. Med PediatrOncol 41: 454-459.
- Dominkus M, Ruggieri P, Bertoni F, Briccoli A, Picci P, (2006) Histologically verified lung metastases in benign giant cell tumours-1 cases from a single institution. IntOrthop 30: 499-504.
- Jacopin S, Viehweger E, Glard Y, Launay F, Jouve JL, et al. (2010) Fatal lung metastasis secondary to index finger giant cell tumor in an 8-year-old child. OrthopTraumatolSurg Res 96: 310-313.
- Raskin KA, Schwab JH, Mankin HJ, Springfield DS, Hornicek FJ (2013) Giant cell tumor of bone. The Journal of the American Academy of Orthopaedic Surgeons 21: 118-126.
Relevant Topics
- 3D Printing in Limb-Sparing Surgery
- Adamantinoma
- Aneurysmal Bone Cysts
- Chondrosarcoma
- Chordomas
- Cryosurgery
- Enchondroma
- Ewing’s Sarcoma
- Fibrous Dysplasia
- Giant Cell Tumor of Bone
- Immunotherapy for Osteosarcoma
- Liquid Biopsy in Orthopedic Oncology
- Malignant Osteoid
- Metastatic Bone Cancer
- Molecular Profiling of Bone Tumors
- Multilobular Tumour of Bone
- Orthopaedic Oncology
- Osteocartilaginous Exostosis
- Osteochondrodysplasia
- Osteoma
- Osteonecrosis
- Osteosarcoma
- Primary Bone Tumors
- Sarcoma
- Secondary Bone Tumours
- Targeted Therapy in Bone Sarcomas
- Tumours of Bone
Recommended Journals
Article Tools
Article Usage
- Total views: 4840
- [From(publication date):
June-2017 - Jun 30, 2025] - Breakdown by view type
- HTML page views : 3924
- PDF downloads : 916