Research Article Open Access
Clinical Experience with Lift Technique For Complex Anal Fistulas
Erdinc Cetinkaya*, Bekir Bulut, Siyar Ersoz, Cem Emir Guldogan, Ozgur Akgul, Bulent Cavit Yuksel and Ahmet Kessaf Aslar
Ankara Numune Training and Research Hospital, Turkey
- *Corresponding Author:
- Erdinc Cetinkaya
MD, Department of Colorectal Surgery
General Surgery, Ankara Numune Training and Research Hospital
S�±hhiye 06100, Post Code: 06100 Ankara, Turkey
Tel :+90 505 2918788
Fax: +90 312 3114340
E-mail: drerdinccetinkaya@gmail.com
Rec date: Mar 29, 2016; Acc date: May 11, 2016; Pub date: May 16, 2016
Citation: Cetinkaya E, Bulut B, Ersoz S, Guldogan CE, Akgul O, et al. (2016) Clinical Experience with Lift Technique For Complex Anal Fistulas. J Gastrointest Dig Syst 6:425. doi:10.4172/2161-069X.1000425
Copyright: © 2016 Cetinkaya E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Aim: In this study we aimed to assess the results of LIFT technique for the patients with complex anal fistula in our colorectal unit.
Methods: A total of 24 consecutive patients with complex anal fistula were recruited in our prospective study between January 2014 and July 2014. Outcome measures included presence of recurrence, fecal incontinence and surgical complications.
Results: We enrolled 24 patients with a mean age of 40.5 (range 16-69) years,ten of the patients had recurrent fistulas and 14 were newly diagnosed. Mean follow-up was 4 months. Successful fistula repair was achieved in the 87.5% of the patients, 3 patients had failure at the follow-up. No incontinence was observed in any of the patients.
Conclusion: Ligation of the intersphincteric tract is a novel sphincter-preserving method for complex anal fistulas. As a simple, safe, cost-effective procedure with high success rates it could be candidate for being the gold standart method for complex anal fistulas.
Keywords
Barriers to cessation; Reasons for quitting; Cigarette; Drinking; Concurrent
Introduction
An anal fistula is an abnormal pathological tract between the anal canal and the perianal skin which primarily originates from the abscess formation with crypto-glanduler infection. The estimated prevalence of anal fistula is 12 to 28/100.000 of the per year and male to female ratio is 1.8:1 [1].
The classification of the anal fistula has shown variabilities, but the simplest and the most widely used one is the Park’s classification. In this classification five main types are described according to the relationship of the fistula to the anal sphincter muscles; intersphincteric, transsphincteric, suprasphincteric, extrasphincteric and superficial fistulas [2]. This system doesn’t describe the presence of abscesses, fistulas connections to bladder or vagina, so that modified Park’s classification system had been formed. The anal fistulas are also described as simple or complex fistulas by American Gastroenterological Association. The simple fistulas originate below the dentate line (low type) and involves small part ofthe sphincter complex. Superficial, low intersphincteric or low transsphincteric fistulas are in this group. Conversely complex fistulas originate above the dentate line (high type), and involves the significant part of the sphincter mechanism. Anterior fistula in women, recurrent fistula,fistulas with multiple tracts, patients with preexisting incontinence are included in this group. And complex fistulas may be associated with local irradiation or Crohn disease [2-4].
The surgical treatment of anal fistula has been a challenge for both surgeons and patients. Simple anal fistulas can be treated by fistulotomy with low recurrence rates and the risk of sphincter damage is low as most of the sphincter mechanism is preserved [2,5,6]. However for complex and high anal fistulas, surgical treatment poses an increased risk of incontinence depending on the probable risk of damaging the sphincter muscles. Therefore ideal treatment of anal fistula is the complete healing of fistula tract while preserving the anal sphincter mechanism and preventing the recurrence.
There are variable surgical procedures for the management of anal fistula with variable risk of incontinence and recurrence. In 2006 from Thailand, Rojanasakul et al. performed a novel sphincter saving technique consisting of ligation of the intersphincteric tract (LIFT) and showed high rates of success in healing fistula tract up to 94% of the patients [7]. In this observational prospective study we aimed to assess the results of the LIFT technique for the patients with complex anal fistula in our colorectal unit.
Materials and Methods
The study was conducted between January 2014 and July 2014 after obtaining approval from Ethics Committee at Ankara Numune Training and Research Hospital ( approval no.895 at 2014). Twentyfour consecutive patients with complex anal fistula who underwent the LIFT procedure were included. The anal fistulas associated with inflammatory bowel disease and tuberculosis were excluded.
All patients were examined by colorectal surgeon in outpatient clinic. After initial investigations including the history was taken, digital rectal examination and physical examination was performed. All of the patients underwent preoperative magnetic resonance imaging (MRI). Park’s classification was used for describing the anal fistulas type according to the MRI findings. All of the anal fistulas in the study were classified as complex fistula.
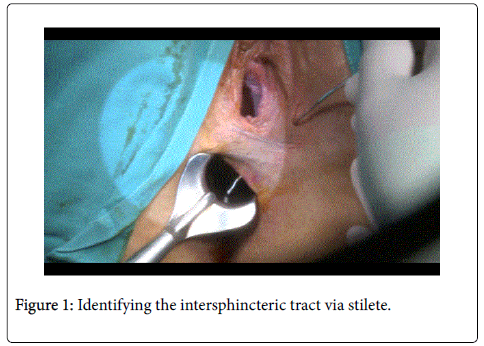
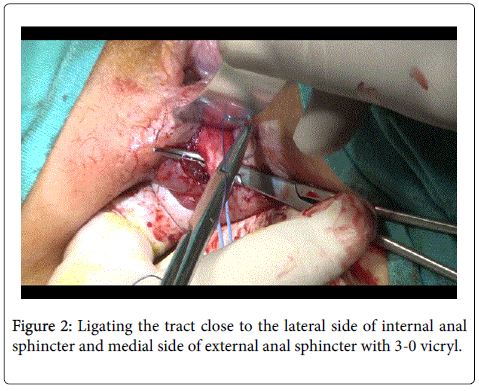
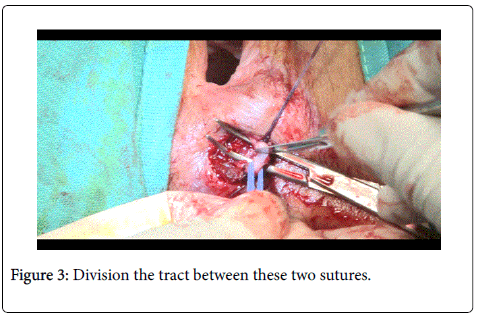
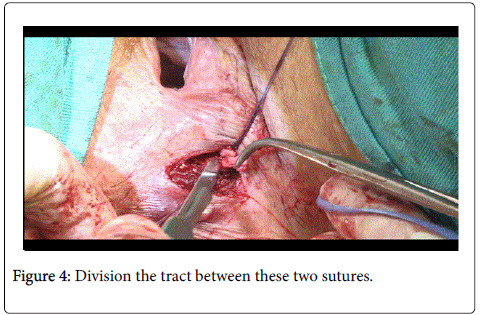
After the adequate fasting period, enema was administered for bowel preparation. The procedure was performed under general or regional anesthesia and patient was placed in the lithotomy position. Povidone iodine was used for the surgical field cleansing. The external opening of the anal fistula was identified, anoscope was placed after anal dilatation and hydrogen peroxide (H2O2) was injected through the external opening for identifying the internal opening. The stilete was forwarded through the external opening to the internal opening for identifying the intersphincteric tract (Figure 1). Then the intersphincteric groove was determined and 2 cm circumanal incision was made at the site of fistula tract to enter the intersphincteric plane. Meticulous dissection was performed via electrocautery for dissecting the intersphincteric plane to isolateintersphincteric tract. Two retractors were used. The right-angled clamp was used to isolate and circle the tract. After the stilete was removed, tract was ligated close to the lateral side of internal anal sphincter and medial side of external anal sphincter with 3-0 vicryl (Figure 2). We divided the tract between these two sutures (Figures 3 and 4). To control the closure of the internal and external fistula tract, we injected H2O2 from the internal and external openings. After the fistula tract was curetted, surgical field was irrigated with saline and H2O2. For the intersphincteric incision interrupted polyglactin 3-0 suture was used. The external orifice was left open for drainage.
All of the patients were discharged the day after the operation. All patients were recommended to perform sitz bath 2-3 times a day for 15 minutes each time. Also the patients were advisedto take antiinflammatory analgesic if they feel pain and record the need of the medication. No antibiotics were prescribed. Patients were evaluated at the surgical outpatient clinic at the first week, first and fourth month after the surgery. The need of anti-inflammatory analgesic andsponge requirement for wound discharge was questioned. For the evaluation of incontinence Wexner and Fecal Incontinence Quality of Life (FIQL) score was performed at the follow-up. Time to return the work after the surgey was noted.
Results
A total of 24 consecutive patients with complex anal fistula were recruited in our prospective study between January 2014 and July 2014. Seventeen patients (71%) were men and seven (29%) were women. The mean age was 40.5 years (range 16-69) and follow-up was 4 months. One of the patient had Behçet disease and one of them had chronic obstructive pulmonary disease, the others had no comorbidities. According to the Park’s classification and intraoperatif data, 21 patients were diagnosed with transsphincteric and 3 with intersphincteric fistula. Ten of the patients had recurrent fistulas and 14 patients were newly diagnosed. Anterior anal fistula was described in 12 patients and posterior anal fistula was in 12 patients. All of the patients were discharged home day after the surgery. No early complication as bleeding or severe pain was observed. Mean time to return to the work after surgery was 15.5 days (range 7-35 days). The time period for requirement of sponge for wound discharge was 7 - 90 days. The demographic and clinical characteristics of the patients are shown on the Table 1.
| Number of the patients | 24 |
| Male, n (%) | 17 (71%) |
| Female, n (%) | 7 (29%) |
| Mean age (range) years | 40.5 (16-69) |
| Types of fistula | |
| Transsphincteric | 21 |
| Intersphincteric | 3 |
| Localization of fistula | |
| Anterior | 12 |
| Posterior | 12 |
| Surgery history | |
| Recurrent fistulas | 10 |
| Newly diagnosed | 14 |
Table 1: Demographic and clinical characteristics of the patients.
At the first week follow-up 13 of the patients did not need antiinflammatory analgesic, 7 of the patients needed to take once a day, 4 patients more than twice a day. At the first month follow-up 21 of the patients were free of pain, three of the patients needed antiinflammatory analgesic once a day due to the pain. At the first clinical control five of the patients reported no need of sponge for wound discharge, 13 of them needed once a day, six of them more than once a day. At the first month, need of sponge for wound discharge is once a day for five patients and more than one sponge for two patients. One of the patient had persistent symptoms at the first week, clinical follow-up was recommended and surgery was recommended for recurrence at the first month, but the patient rejected to undergo surgery. One of the patient had discharge ongoing from the incision and had enduration and swelling so under the local anesthesia, incision was opened but no abscess formation was observed. And this patient was free of the symptoms at the fourth month. At the 45th day after the surgery, another patient with transsphincteric fistulawas evaluated because of the persisting wound discharge and reoperated with fistulotomy as the recurrent anal fistula was identified as simple fistula.
At the end of the follow-up, 21 patients (87.5%) had healed with recurrence free and 3 patients (12.5%) had recurrence (Table 2). No fecal or gas incontinence was observed in any of the patients at the follow-up. Postoperative we disconnect the fistula tract and it may mislead in screening tecnique. Because of that we didn't use MRI to check if the anal fistula has been screening cure. Instead of that, we emphasised the fecal incontinence and FIQL.
Discussion
In this study our experience showed that LIFT technique can be preferred treatment option for complex anal fistulas with preventing the recurrence and preserving the incontinence. The surgical treatment of anal fistula aims to eradicate septic focus and fistula tract while preserving anal sphincter function, preventing recurrence, providing comfort and allowing patients to return the normal daily activities as early as they can. LIFT technique could achieve these goals as in the recent metanalysis over 24 articles showed that during the 10.3 monthof follow-up, mean succeess rate was 76.4%, no incontinence was observed, intraoperative and postoperative complication rates were 0 and 5.5%respectively [8].
It is important to consider that no single technique is the best for the treatment for all types of anal fistula. Most of the anal fistulas are simple or superficial and can be treated by fistulotomy with a little incontinence and with an approximately 100% high success rate [9]. Also for complex fistulas, there are many sphincter sparing treatment options but the recurrence and incontinence risk after these procedures should be kept in mind. The recurrence and incontinence rates were reported as 0-63% and 0-32% respectively according to the surgical technique [10,11]. Seton techniques have been used in the management of fistulas which are simple and safe methods. Inserting a foreign material through the tract and providing the tract to be open, prevents closed space infections and allows the drainage [12]. But this is a painful and uncomfortable technique for the patients with incontinence being reported to be as high as 60% [13]. Advancement flap is technically more difficult method especially on posteriorly located fistulas and risk of devascularization and loss of the larger portion of rectal wall exists. Although it is stil considered to be the gold standart method for treating complex anal fistulas, successful healing rates range from 55 to 98% [13-18]. And this procedure has an incontinence risk up to 35% [18]. Fibrin glue injection for the management of complex anal fistula was first published by Hjortup et al. in 1991 with promising results but further reports showed success rates varying from as low as 14% [19] to as high as 74% [20]. Similarly the anal fistula plug is a novel method with success rates varying between 29% and 87% [21-23]. Fistula laser closure and video assisted anal fistula treatment procedures are new and expensive and further studies are required for both of these techniques use in clinical practice [24].
Since the first description in 2006 by Rojanasakul [7], LIFT technique has taken interest because of its high success rate and no impact on continence. This simple, safe, sphincter preserving procedure with short healing time has became more popular from 2010. According to the recent metaanalysis published in 2014, pooled results of LIFT indicate that mean success, incontinence, intraoperative and postoperative complication rates were 76.4, 0, 0, 5.5% respectively. It was indicated that, due to the variability of the studies, the pooled success rate should be interpreted with caution. The follow-up time, study size and combining procedures with LIFT could affect the results [8]. In our study the success rate of 87.5% is comparable to the healing rates with other studies, and no fecal or gas incontinence was observed in any of the patients.
Bleir et al., represented the first North America experience with LIFT, including 39 patients with complex anal fistulas. The healing rate was 57% and 4 of the patients failed recurrence. Although no continence scoring questionnaire was performed in that study, none of the patients reported subjective incontinence. The low success rates compared to the other studies were attributed to the high percentage of the patients (74%) who had previous procedures with a median of 2 failed repairs [25]. Sileri et al., reported 83.3% success rate with no recurrence, and 3 patients required drainage seton insertion and delayed LIFT. And they stated that no continence change was observed in their study [26].
The metanalysis included one randomized controlled trial, three case control studies and 20 prospective or retrospective case series [8]. We designed our study as prospective case series with 24 patients. In our clinic before the initiation of the study we had experienced LIFT technique for 20 consecutive patients. And according to the literature search, our study represents the largest published case series from our country, Turkey. The healing rate was similar to the literature. Most of the studies evaluated the continence in clinic subjectively, but different scoring systems were performed in some studies. For example, Fecal Incontinence Severity Index (FISI) was used by Sileri et al. [26], Mushaya et al. [27] and Ooi et al. [28] used Cleveland Clinic Florida Fecal Incontinence Score (CCF-FI). No incontinence was documented in these studies. The other scoring systems used wereWexner and Rookwood score. We evaluated patients with Wexner and Fecal Incontinence Quality of Life (FIQL) scores and we did not observe incontinence at the follow-up period.
The follow-up time after the surgery varies between the studies. The mean follow-up time was 10.3 months in the review published in 2014. It was stated that short-term follow-up may overestimate the real success rate. Although most of the studies had follow-up period lower than one year, as the failures would occur after this time, longer followup is recommended [8]. Bleier et al. reported two patients recurred after 30 weeks, although their median time of failure was 10 weeks [26]. In our study we identified this period as 4 months which may be a short time to observe the recurrences however in this time two of the patients had failure.
In the literature there are two studies comparing the LIFT and endorectal advancement flap (ERAF). One of them is a retrospective study from Singapore which aimed to compare the outcomes of ERAF with LIFT approach in patients with complex anal fistulas who had seton insertion previously. After a median follow-up of 13 months, success rate was 62.5% for LIFT group, after 6 months 93.5% for ERAF group. The higher failure rate for LIFT was attributed to the scarring result in the obliteration of the intersphincteric space, complicate the identification of the fistula tract and different duration of the follow-up of these two techniques [29]. Mushaya et al. designed a randomized controlled study in 2012 which the patients treated with LIFT or anorectal advancement flap (ARAF). They reported low recurrence rates of 8% for LIFT and 7% for ARAF. They did not find difference in continence scores between the two groups. It was stated that LIFT was simpler, results in better quality of life for patients and less painful [28].
In our study we experienced high success rates compatible with the published studies. Low recurrence risk and undamaged sphincter mechanism will support the choice of the surgery modality for complex anal fistulas. The major limitations of our study were In our study we experienced high success rates compatible with the published studies. Low recurrence risk and undamaged sphincter mechanism will support the choice of the surgery modality for complex anal fistulas. The major limitations of our study were relatively small numbers of patients and the shorter follow-up time. But with the help of our study, we consider to choose LIFT for patients with complex anal fistula as a simple, cost-effective and safe treatment option. As the other sphincter-preserving procedures exist, further randomized controlled trials are needed to evaluate the effectiveness of LIFT compared to others. In conclusion LIFT seems to be candidate for being the gold standart surgery option as the features mentioned above.
References
- Zanotti C, Martinez-Puente C, Pascual I, Pascual M, Herreros D, et al. (2007) An assessment of the incidence of fistula-in-ano in four countries of the European Union.Int J Colorectal Dis 22: 1459-1462.
- Parks AG, Gordon PH, Hardcastle JD (1976) A classification of fistula-in-ano.Br J Surg 63: 1-12.
- Sandborn WJ, Fazio VW, Feagan BG, Hanauer SB; American Gastroenterological Association Clinical Practice Committee (2003) AGA technical review on perianal Crohn's disease.Gastroenterology 125: 1508-1530.
- Vasilevsky CA, Beck DE, Roberts PL (2011) Anorectal abscess and fistula. The AS-CRS (Text book) of colon and rectal surgery (2nd edn) Springer, New York, 219-244.
- Whiteford MH, Kilkenny J, Hymann N (2005) The standarts practice task force, American Society of Colon and Rectal Surgeons. Practice parameters for the treatment of perianal abscess and fistulo-in-ano. Dis Colon Rectum 48: 1337.
- Seow-Choen F, Nicholls RJ (1992) Anal fistula.Br J Surg 79: 197-205.
- Rojanasakul A, Pattanaarun J, Sahakitrungruang C, Tantiphlachiva KJ (2007)Total anal sphincter saving technique for fistula-in-ano; the ligation of intersphincteric fistula tract. Med Assoc Thai 90: 581-586.
- Hong KD, Kang S, Kalaskar S, Wexner SD (2014) Ligation of intersphincteric fistula tract (LIFT) to treat anal fistula: systematic review and meta-analysis.Tech Coloproctol 18: 685-691.
- Rizzo JA, Naig AL, Johnson EK (2010) Anorectal abscess and fistula-in-ano: evidence-based management.Surg Clin North Am 90: 45-68, Table of Contents.
- Rojanasakul A (2009) LIFT procedure: a simplified technique for fistula-in-ano.Tech Coloproctol 13: 237-240.
- Garcia-Aguilar J, Belmonte C, Wong WD, Goldberg SM, Madoff RD (1996) Anal fistula surgery. Factors associated with recurrence and incontinence.Dis Colon Rectum 39: 723-729.
- Bleier JI, Moloo H (2011) Current management of cryptoglandular fistula-in-ano.World J Gastroenterol 17: 3286-3291.
- García-Aguilar J, Belmonte C, Wong DW, Goldberg SM, Madoff RD (1998) Cutting seton versus two-stage seton fistulotomy in the surgical management of high anal fistula.Br J Surg 85: 243-245.
- Parks AG, Stitz RW (1976) The treatment of high fistula-in-ano.Dis Colon Rectum 19: 487-499.
- Mizrahi N, Wexner SD, Zmora O, Da Silva G, Efron J, et al. (2002) Endorectal advancement flap: are there predictors of failure?Dis Colon Rectum 45: 1616-1621.
- Zimmerman DD, Briel JW, Gosselink MP, Schouten WR (2001) Anocutaneous advancement flap repair of transsphincteric fistulas.Dis Colon Rectum 44: 1474-1480.
- Sonoda T, Hull T, Piedmonte MR, Fazio VW (2002) Outcomes of primary repair of anorectal and rectovaginal fistulas using the endorectal advancement flap.Dis Colon Rectum 45: 1622-1628.
- Zimmerman DD, Delemarre JB, Gosselink MP, Hop WC, Briel JW, et al. (2003) Smoking affects the outcome of transanal mucosal advancement flap repair of trans-sphincteric fistulas.Br J Surg 90: 351-354.
- Buchanan GN, Bartram CI, Phillips RK, Gould SW, Halligan S, et al. (2003) Efficacy of fibrin sealant in the management of complex anal fistula: a prospective trial.Dis Colon Rectum 46: 1167-1174
- Patrlj L, Kocman B, Martinac M, Jadrijevic S, Sosa T, et al. (2000) Fibrin glue-antibiotic mixture in the treatment of anal fistulae: experience with 69 cases.Dig Surg 17: 77-80.
- Christoforidis D, Etzioni DA, Goldberg SM, Madoff RD, Mellgren A (2008) Treatment of complex anal fistulas with the collagen fistula plug.Dis Colon Rectum 51: 1482-1487.
- Johnson EK, Gaw JU, Armstrong DN (2006) Efficacy of anal fistula plug vs. fibrin glue in closure of anorectal fistulas.Dis Colon Rectum 49: 371-376.
- Lawes DA, Efron JE, Abbas M, Heppell J, Young-Fadok TM (2008) Early experience with the bioabsorbable anal fistula plug.World J Surg 32: 1157-1159.
- Limura E, Giordano P (2015) Modern management of anal fistula.World J Gastroenterol 21: 12-20.
- Bleier JI, Moloo H, Goldberg SM (2010) Ligation of the intersphincteric fistula tract: an effective new technique for complex fistulas.Dis Colon Rectum 53: 43-46.
- Sileri P, Franceschilli L, Angelucci GP, D'Ugo S, Milito G, et al. (2011) Ligation of the intersphincteric fistula tract (LIFT) to treat anal fistula: early results from a prospective observational study.Tech Coloproctol 15: 413-416
- Mushaya C, Bartlett L, Schulze B, Ho YH (2012) Ligation of intersphincteric fistula tract compared with advancement flap for complex anorectal fistulas requiring initial seton drainage.Am J Surg 204: 283-289.
- Ooi K, Skinner I, Croxford M, Faragher I, McLaughlin S (2012) Managing fistula-in-ano with ligation of the intersphincteric fistula tract procedure: the Western Hospital experience.Colorectal Dis 14: 599-603.
- Tan KK, Alsuwaigh R, Tan AM, Tan IJ, Liu X, et al. (2012) To LIFT or to flap? Which surgery to perform following seton insertion for high anal fistula?Dis Colon Rectum 55: 1273-1277.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 21142
- [From(publication date):
June-2016 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 20267
- PDF downloads : 875