Clinical, Etiological and Neuroimaging Profile of Pediatric Stroke at a Tertiary Care Center
Received: 05-Nov-2021 / Accepted Date: 19-Nov-2021 / Published Date: 26-Nov-2021
Abstract
Introduction: Stroke, defined as the sudden occlusion or rupture of cerebral arteries or veins resulting in focal cerebral damage or neurological deficits in children, differs in clinical presentation, etiology and neuroimaging from adults.
Material and Methods: This hospital based observational study aimed to assess the clinical etiological patterns and neuroimaging profile of childhood stroke evaluated 75 pediatric stroke patients between the ages of 6 months to 18 years.
Results: Early childhood is the most common period for stroke, males are affected more predominantly. CNS infection was found the most common cause of stroke, CNS T.B being the most common. Hemiplegia was the most common presentation of stroke and AIS being most common type of stroke. Causes of stroke in children are varied and differ from those seen in adults.
Conclusion: Even after many decades of initial studies, not much information is available on this aspect in India. Adequate identification and determination of etiology is absolutely necessary as stroke can be prevented in some children and treated in others. With the help of newer diagnostic facilities, probability of finding an etiology of stroke is increased for infectious and non-infectious causes.
Keywords: Pediatric stroke; Neuroimaging; Hemiplegia; AIS; CSVT; Hemorrhagic stroke; Moya-Moya disease
Introduction
Stroke, a diagnosis considered commonly in adults and elderly, is now being diagnosed frequently in pediatric patients also [1]. Definition of adult stroke as an acute onset neurological sign or symptom attributable to focal brain infarction or hemorrhage is applicable in children as well [2,3]. Ischemic stroke incidence is estimated 1.0 to 2.0 in 100 000 children (nonneonates) annually in developed countries. Incidence differs by age and sex; highest in infants and children <5 years of age and higher in boys than girls. Higher incidence is reported in Black and Asian children than white children [4].
Krishnamurthy, et al. evaluated pediatric stroke cases in different geographical regions between 1990 to 2013, and noted significant global increase in the absolute number of prevalent strokes in children of ≈35% since 1990. The mortality rate showed significant decline, with boys showing a trend toward higher childhood stroke death rates (95% CI, 1.5 [1.3-1.8] per 1, 00, 000) than girls (95% CI, 1.1 [0.9-1.5] per 1, 00,000) globally in 2013. These findings suggest that pediatric strokes are important global public health concern [5].
Accurate and timely diagnosis is often challenging and stroke is correctly diagnosed only in ≈60% of children, giving ≈40% of cases an incorrect initial diagnosis [6]. This suggests a need to develop programs of education to improve knowledge and skills, bedside clinical assessment methods and better imaging techniques for diagnosis of pediatric stroke in children with improved sensitivity and specificity and to identify modifiable stroke risk factors for preventive strategies. There is limited understanding of pathogenesis, and approximately one-quarter to one-third of all childhood strokes remain ‘idiopathic’ [7]. Also, Risk factors and causes of Pediatric stroke differ as chronic diseases such as atherosclerosis, hypertension, hypercholesteremia/ hyperlipidemia, diabetes, and smoking are more common in adults.
Materials and Methods
This hospital based, observational study aimed to assess the socioclinical and etiological patterns and neuroimaging profiles of childhood stroke was conducted at Department of Pediatrics, S.M.S. Medical College Jaipur (Rajasthan) from June 2019 to December 2019, after getting requisite clearance from institutional ethics committee. Sample size is calculated at 95% confidence level, alpha error of 0.05, at 10% absolute available error in the above mention clinical manifestation, the required sample size was 75 cases. Patients between the age group of 6 months to 18 years admitted with signs and symptoms suggestive of stroke (hemiparesis, fever, seizure, altered consciousness, etc.,) and later diagnosed as stroke by radio-imaging during the study period were included in the study. Those refusing for consent, presenting with paraplegia/paraparesis, spinal cord/brain trauma and children less than 6 months of age were excluded.
Results
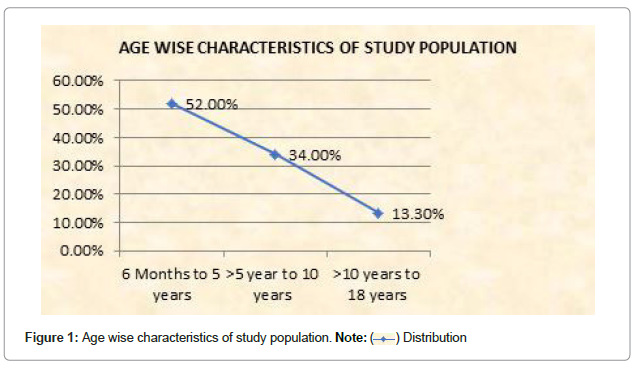
TThis study evaluated 75 pediatric stroke patients aged between 6 months to 18 years, out of which 65.3% (48) were males and 34.7% (27) were females suggesting male preponderance (M: F=1.89:1). Age group of 6 months to 5 years constituted 52% (39), age group of >5 years to 10 years 34% (26) and age group of >10 to 18 years 13.3% (10) suggesting high prevalence of stroke in early childhood (Figure 1). 42 subjects were from Hindu, 32 from Muslims and 1 from Sikh religious background.
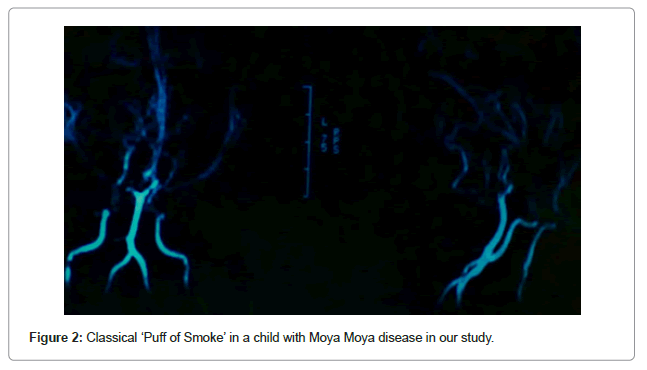
67% patients were having some co-morbidity. CNS Infections (52%, n=29; M-19, F-10) were the most common co-morbidity with pediatric stroke. Tubercular meningitis was the most common (16%, n=12; M-8, F-4) CNS infection followed by Meningo-encephalitis (12%, n=9; M-6, F-3) and Viral Encephalitis (10.6%, n=8, M-5, F-3). Vascular causes (16%, n=12, M-8, F-4) including Moya-Moya (5.3%, n=4 M-3, F-1, Figure 2), Vasculitis (6.6%, n=5, M-3, F-2) and Nonspecific vascular malformation (4%, n=3, M-2, F-1) were the second most common cause identified.
Hematological causes (13.3%, n=10, M-6, F-4) including Protein C, S deficiency (8%, n=6, M-3, F-3), Thrombocytopenia (2.6%, n=2, M-1, F-1), Sickle cell disease (2.6%, n=2, M-2) were the third most common cause identified. Cardiac causes (6.6% n=5, M-3, F-2=Acyanotic CHD 4%, DCM-2.6%) and other causes like homocystenemia (3%), mastoid sinusitis (1%) arteriopathy, ICH (1.3%) (5.3%, n=4; M-2, F-2) were identified associated.
In 27.7%, (n=15; M-10, F-5) cases, even after intensive diagnostic investigations and efforts, no clear etiology was found (Table 1).
| Condition | n (%) | Hindu (n=42) | Muslim (n=32) | Sikh (n=2) |
|---|---|---|---|---|
| Infection | 29 (52%) | 18 | 10 | 1 |
| T.B meningitis | 12 (16%) | 5 | 7 | 0 |
| Meningo-encephalitis | 9 (12%) | 6 | 3 | 0 |
| Encephalitis | 8 (10.6%) | 4 | 3 | 1 |
| Vascular | 12 (16%) | 7 | 5 | 0 |
| Vasculitis | 5 (6.6%) | 3 | 2 | 0 |
| Moya Moya Disease | 4 (5.3%) | 3 | 1 | 0 |
| Nonspecific vascular malformation | 3 (4%) | 1 | 2 | 0 |
| Haematological | 10 (13.3%) | 6 | 4 | 0 |
| Protien C, S deficiency | 6 (8%) | 4 | 2 | 0 |
| Thrombocytopenia | 2 (2.6%) | 1 | 1 | 0 |
| Sickle cell | 2 (2.6%) | 1 | 1 | 0 |
| Cardiac (CHD, RHD, DCM) | 5(6.6%) | 3 | 2 | 0 |
| Others | 4 (5.3%) | 2 | 2 | 0 |
| Idiopathic | 15 (27.7%) | 8 | 7 | 0 |
Table 1: Underlying/co-morbid conditions in patients with stroke.
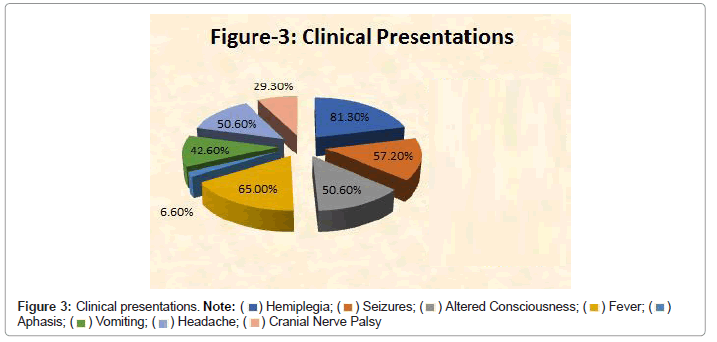
The most common clinical presentation of childhood stroke was hemiplegia (81.3%, n=61), followed by seizure (57.3%, n=43), altered consciousness (50.6%, n=38), fever (65%, n=49) and cranial nerve palsy (29.3%, n=22), and aphasia (6.6%, n=5), vomiting (42.6%, n=32) respectively (Figure 3).
Seizures were noted in 57.3% (n=43) children, seizure patterns and level of consciousness have been depicted in Table 2.
| AIS (n=54) | CSVT (n=9) | H (n=4) | Others (n=8) | Total (n=75) | |
|---|---|---|---|---|---|
| Type of seizures | |||||
| Generalized | 16 | 2 | 3 | 6 | 27 (36%) |
| Focal | 12 | 2 | 1 | 1 | 16(21.33%) |
| No seizures | 26 | 5 | 0 | 1 | 32(42.66%) |
| Level of consciousness | |||||
| Impaired | 32 | 2 | 4 | 7 | 45 (60%) |
| Conscious | 22 | 7 | 0 | 1 | 30 (40%) |
Table 2: Seizures pattern and level of consciousness in patients having stroke.
Neuroimaging findings
Out of total 75 stroke patients, 54 (72.2%) cases were diagnosed as acute ischemic stroke and 4 (5.3%) cases as a hemorrhagic stroke. CSVT diagnosed in 9 (12%) patients and others are 8 (10.6%). AIS diagnosed in 32 (42.6%) males and 22 (29.3%) females (Table 3).
| Gender | AIS | CSVT | Hemorrhagic | Others |
|---|---|---|---|---|
| Male(n=48) | 32 (42.6%) | 8 (10.6%) | 03 (4.0%) | 05 (6.6%) |
| Female (n=27) | 22 (29.3%) | 01 (1.3%) | 01 (1.3%) | 03 (4.0%) |
| Total (n=75) | 54 (72%) | 09 (12%) | 04 (5.3%) | 08 (10.6%) |
Table 3: Type of stroke.
Middle Cerebral Artery (MCA-52%) was involved most commonly, followed by ICA (21.33%), PCA (12%) MCA+PCA (8%), ACA+MCA+PCA (4%), and ACA+PCA alone (2.67%) (Table 4).
| Age | MCA | PCA | ICA | MCA+PCA | ACA+PCA | ACA+MCA+PCA |
|---|---|---|---|---|---|---|
| 6 m to 5 yrs (n=39) | 22 | 6 | 8 | 3 | 1 | 2 |
| >5-10 yrs (n=26) | 10 | 2 | 5 | 2 | 1 | 1 |
| >10-18yrs (n=10) | 7 | 1 | 3 | 1 | 0 | 0 |
| Total=75 | 39 (52%) | 9 (12%) | 16 (21.33%) | 6 (8%) | 2 (2.67%) | 3 (4%) |
Table 4: Vascular territory involved.
Discussion
Male preponderance noted in our study was also found in other studies [4,8]. We found maximum patients in age group of 6 months to 5 years, 52% (n=39), showing high prevalence of stroke in early childhood. The study conducted by Parakh, et al. 2014 depicts maximum 24 (48%) cases in the age group of 6-24 months (mean-13.5 ± 6.19 months) and incidence of stroke was more common before 5 years. The incidence of stroke was found decreasing with increasing age of children [4,8,9].
In the present study, intracranial infection is the most common etiology, causing stroke (n=29) 52%. Out of which CNS T.B being most common cause (n=12) 16%, followed by vascular (n=12) 16%, hematological (n=10) 13.3%, cardiac (n=5) 6.6% and unknown (n=15) 27.7% for which exact etiology cannot be found.
The associated co-morbidity found in our study are similar to study conducted by Dr. Shri Ganesh Patil depicting intracranial infection to be the most common (12 children; 38.70%), cause of ischemic stroke followed by idiopathic (7 patients; 22.58%), Moya Moya Disease (6 patients; 19.53%), hematological (4 patients; 12.90%), and cardiac (2 patients; 6.45%) [10]. Another study of 130 children in turkey found that, the five most common factors were infectious diseases (18%), cardiac diseases (13%), MTHFR polymorphisms (10%), trauma (8%), and Moya Moya disease (5%) [11].
In our study, out of 75 cases, religious background of 42 patients is Hindu, 32 Muslims and 2 patients were Sikh religious background. We found that, out of 29 patients with infectious cause of stroke, Hindu (n=18), Muslim (n=10), Sikh (n=2). CNS T.B (n=12) was found in Hindu (n=5) and Muslim (n=7) religious background. These findings are not comparable with any other study; higher incidence is reported in Black and Asian children than white children [4].
The most common clinical presentation of childhood stroke was hemiplegia followed by seizure, altered consciousness, fever, cranial nerve palsy, aphasia and vomiting, in our study. Clinical presentation depends on age and type of stroke. The most common symptoms include hemiparesis and hemi facial weakness in 67% to 90%, speech or language disturbance in 20% to 50%, vision disturbance in 10% to 15%, and ataxia in 8% to 10%. Children present with non-localizing symptoms such as headache in 20% to 50% and altered mental status in 17% to 38%. Seizures at stroke onset are more common in children than adults, affecting 15% to 25%, especially in those <6 years of age [4,12,13]. Study conducted by Dr. Shri Ganesh Patil found hemiparesis (28 cases [84.84%]), followed, respectively, by seizure (19 cases [54.54%]), altered consciousness (17 cases [51.51%]), both fever and cranial nerve palsy (15 cases [45.45%] each), and finally speech abnormality [10].
In our study, AIS was diagnosed in 32 (42.6%) males and 27 (29.2%) females. CSVT diagnosed in 8 males and 1 female and Hemorrhagic in 3 males and 1 female. Others causes were noted in 5 males and 3 females. Based on recent advancements in MRI and radio-imaging, we can diagnose stroke in early stages which help clinicians to prevent long term morbidity and mortality in patients. AIS resulting from cardiac disease affect younger children, with a median age of 6 months to 3 years [14]. Braun, et al. noted that, cardioembolic stroke may present with abrupt onset in contrast to fluctuating presentation of stroke caused by arteriopathy [15]. A 7-year single-center cohort study included 54 children with Moya Moya arteriopathy (median age at diagnosis, 7.5 years), and depicted TIAs in 70% and acute AIS in 48% [16]. Study conducted by IPSS found that Focal features, in particular hemiparesis were the most common presenting features of arterial ischemic stroke and hemiparesis was the most common presenting feature of pediatric stroke [17].
The study of 130 children with stroke in turkey depicted Focal neurological signs (87%) as the most common presentation and hemiplegia and/or hemiparesis as most common focal sign followed by Focal or generalized convulsions as second most common presentation (58%) [11]. Study conducted by Ramaswamy Ganesh found that, 83% of children presented with hemiplegia/hemiparesis, 33% with seizures, and 8% with ataxia.
In our study, Middle Cerebral Artery (MCA-52%) was involved most commonly, followed by ICA (21.33%), PCA (12%) MCA+PCA (8%), ACA+MCA+PCA (4%), and ACA+PCA alone (2.67%). Study conducted by Manish parakh found that, MCA was the most common territory involved at all ages (45.6%) followed by ICA (19.6%), MCA+PCA (13%), ACA+MCA+PCA (10.9%), and PCA alone (8.7%). A study of 60 children with Moya Moya, 55 children (92%) had recurrent TIAs [18].
Posterior circulation (vertebral artery and its branches) stroke affects previously healthy, mostly male (67% to 77%) children at a median age of 7 to 8 years. Presenting signs and symptoms are hemiparesis, ataxia, dysarthria, visual field deficits, and oculomotor deficits. Nonlocalizing symptoms like headache, vomiting, and altered mental status occur in 60% to 70%. Vertebral Artery (VA) dissection is the most common underlying cause (25%-50%) [19].
Conclusion
The current study has provided valuable information about clinic- etiological profile of pediatric stroke. Early childhood is the most common period for stroke, males are affected more predominantly. CNS infection was found the most common cause of stroke, CNS T.B being the most common. Hemiplegia was the most common presentation of stroke and AIS being most common type of stroke. Causes of stroke in children are varied and differ from those seen in adults. One or more risk factors can be identified in up to three fourths of children with ischemic stroke and an even greater percentage in children with hemorrhagic stroke. Even after many decades of initial studies on etiology and outcome of stroke in pediatric population not much information is available on this aspect in India. Adequate identification and determination of etiology is absolutely necessary as stroke can be prevented in some children and treated in others.
Many patients of stroke completely recovered. With the help of newer diagnostic facilities, probability of finding an etiology of stroke is increased for infectious and non-infectious causes. Neuroimaging has the most important role. Newer modalities of treatment increased chances of recovery many folds from previous times. We suggest prompt identification of stroke and early diagnosis and prompt treatment in stroke to prevent long term morbidity and mortality also.
References
- Ferriero DM, Fullerton HJ, Bernard TJ, Billinghurst L, Daniels SR, et al. (2019) Management of stroke in neonates and children: A scientific statement from the American Heart Association/American Stroke Association. Stroke 50: e51-96.
- Grinnon ST, Miller K, Marler JR, Lu Y, Stout A, et al. (2012) National Institute Of Neurological Disorders And Stroke Common Data Element Project: Approach and methods. Clin Trials 9: 322-329.
- Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, et al. (2013) An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44: 2064-2089.
- Mallick AA, Ganesan V, Kirkham FJ, Fallon P, Hedderly T, et al. (2014) Childhood arterial ischaemic stroke incidence, presenting features, and risk factors: A prospective population-based study. Lancet Neurol 13: 35-43.
- Krishnamurthi RV, deVeber G, Feigin VL, Barker-Collo S, Fullerton H, et al. (2015) Stroke prevalence, mortality and disability-adjusted life years in children and youth aged 0-19 years: Data from the Global and Regional Burden of Stroke 2013. Neuroepidemiology 45: 177-189.
- Mackay MT, Monagle P, Babl FE (2017) Improving diagnosis of childhood arterial ischaemic stroke. Expert Rev Neurother 17: 1157-1165.
- Fullerton HJ, Wu YW, Sidney S, Johnston SC (2007) Risk of recurrent childhood arterial ischemic stroke in a population-based cohort: The importance of cerebrovascular imaging. Pediatrics 119: 495-501.
- Parakh M, Arora V, Khilery B (2014) A prospective study evaluating the clinical profile of pediatric stroke in Western Rajasthan. J Neurol Disord 2: 187.
- Ganesh R, Deenadayalan M, Janakiraman L, Viswanathan V (2015) Pediatric strokes: A hospital-based observation. J Pediatr Neurol 4: 041-044.
- Patil S, Adhikari-Thakker A, Gajre M, Garegrat R (2019) Clinico-etiological profile of childhood stroke in a tertiary care hospital in Mumbai. Int J Health Sci Res 9: 25-30.
- Bozpolat A, Unal E, Topaloglu T, Taheri S, Bayram AK, et al. (2019) The relationship between the prognosis of children with acute arterial stroke and polymorphisms of CDKN2B, HDAC9, NINJ2, NAA25 genes. J Thromb Thrombolysis 47: 578-584.
- Yock-Corrales A, Mackay MT, Mosley I, Maixner W, Babl FE (2011) Acute childhood arterial ischemic and hemorrhagic stroke in the emergency department. Ann Emerg Med 58:156-163.
- Wintermark M, Hills NK, DeVeber GA, Barkovich AJ, Bernard TJ, et al. (2017) Clinical and imaging characteristics of arteriopathy subtypes in children with arterial ischemic stroke: Results of the VIPS study. AJNR Am J Neuroradiol 38: 2172-2179.
- Cheng HH, Rajagopal S, McDavitt E, Wigmore D, Williams K, et al. (2016) Stroke in acquired and congenital heart disease patients and its relationship to hospital mortality and lasting neurologic deficits. Pediatr Crit Care Med 17: 976-983.
- Braun KP, Rafay MF, Uiterwaal CS, Pontigon AM, DeVeber G (2007) Mode of onset predicts etiological diagnosis of arterial ischemic stroke in children. Stroke 38: 298-302.
- Amlie-Lefond C, Ellenbogen RG (2015) Factors associated with the pre-sentation of moyamoya in childhood. J Stroke Cerebrovasc Dis 24: 1204-1210.
- Mallick AA, Ganesan V, Kirkham FJ, Fallon P, Hedderly T, et al. (2014) Childhood arterial ischaemic stroke incidence, presenting features, and risk factors: A prospective population-based study, The Lancet Neurol 13: 35-43.
- Zhao M, Zhang D, Wang S, Zhang Y, Wang R, et al. (2017) Transient ischemic attack in pediatric patients with moyamoya disease: Clinical features, natural history, and predictors of stroke. Pediatr Neurol 75: 48-54.
- McCrea N, Saunders D, Bagkeris E, Chitre M, Ganesan V (2016) Diagnosis of vertebral artery dissection in childhood posterior circulation arterial ischaemic stroke. Dev Med Child Neurol 58: 63-69.
Citation: Kumar A, Bagri DR, Sharma JN (2021) Clinical, Etiological and Neuroimaging Profile of Pediatric Stroke at a Tertiary Care Center. J Alzheimers Dis Parkinsonism S8: 031.
Copyright: © 2021 Kumar A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1852
- [From(publication date): 0-2021 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 1311
- PDF downloads: 541