Clinical Application Research of the Improved Mini Laparoscopic Cholecystectomy
Received: 22-May-2018 / Accepted Date: 07-Jul-2018 / Published Date: 18-Jul-2018 DOI: 10.4172/2332-0877.1000371
Keywords: Improved “mini” laparoscopic cholecystectomy; Postoperative pain; Cosmetic eوٴect Clinical application
Introduction
Gallbladder Stone (GS) is a kind of common and multiple disease in hepatobiliary surgery. The GS prevalence rate in Chinese natural population is as high as 0.9%-10.1% [1], and most patients are above 40 years old and obese women. Epidemiology shows that the prevalence rate of Gallbladder Polyps (GP) and GS is going up with the improvement of living standard of social people. Today the direction of surgery is that the best and preferred method of treatment for GP and GS benign disease is Laparoscopic Cholecystectomy (LC) together with microtrauma surgery, microtrauma functionalization and precision surgery. The idea is still that on the base of guarantee of surgery safety, the effects of minimal incision and cosmetology should be as much as possibly pursued. For the cosmetology and concealed incision, the better minimally invasive surgery should be pursued and developed, so the life quality of perioperative patients gets further improved. Surgeons are constantly seeking new improvement and breakthrough for surgical techniques, methods and instruments. Minilaparoscopic surgery means the laparoscope and instrument 5mm below. It is also called minitype laparoscopic surgery. It is developed on the base of traditional laparoscopic surgery and further minimally invasive [2-4].
Information and Method
General information
During the period from Jan. 1, 2013 to Dec. 31, 2017, 341 cases of patient medical records in our hospital were collected for the IMLC (Group A). And 107 cases of patient medical records of the same period were also collected for the Traditional Laparoscopic Cholecystectomy (TLC) and these records were as matched group (Group B). This study was approved by the ethics committee of Guizhou Medical University and adhered to the tenets of the Declaration of Helsinki. Additionally, the written informed consent was obtained from the all patients involved in this study. Institutional review board approval of our municipality was obtained for this study (Institutional review board of Tongrenmunicipality (2015) 24-8th).
Inclusion criteria and exclusion criteria
Inclusion criteria: Persons who meet the following three requirements will be the observing objects for our research group. (1) Confirmed GS and GP by abdominal ultrasound with clinical symptoms. (2) Ages of 20-60. (3) ASA (American Society of Anaesthesiologists) is rated as Level I or Level II.
Exclusion criteria: Persons who have the following cases will not be the observing objects for our research group. (1) Cardiopulmonary dysfunction. (2) Acute attack. (3) Past history of abdominal surgery. (4) Have CBDS, Acute pancreatitis, Biliary tumor and parochial, Pancreatic occupying, etc. (5) Combined hypertension, Diabetic and during perioperative period poor blood glucose control. (6) Scar diathesis.
Observation index and evaluation criterion: Separate records of two groups (Group A and Group B) for the operation time, intraoperative bleeding volume, are there perioperative complications, hospitalization time, the recovery time of intestinal function, pain score and cosmetic effect score on the abdominal wall. The operation time in minutes (min) and taking the recording time as the criterion which was recorded by the circuit nurse in intraoperation. The surgical bleeding volume in millilitre (ml) and taking the bleeding volume as the criterion which was recorded by the anaesthetist in intraoperation. Whether or not appear any complication refer to the recorded number of complications. If no complications, the recorded number is zero. Hospitalization time in days, less than or more than one day, follow the rounding. The recovery time of intestinal function in hours(h) and take the patient’s dictation as criterion, less than or more than the time, follow the rounding. Pain scores adopted Visual Analogue Score (VAS) [5,6]. The specific operation as follows: The incisional line length(10cm) indicates incision pain level. The left end of the line indicates painless (0 score) and the right end of the line indicates the most painful (10 scores). Six hours after the surgery, each patient describes the pain level on the incisional line. Researchers can obtain the corresponding scores by using measuring tools of straightedge and compasses to measure the length of recorded points. The length accurate to 0.1 cm. The grades of abdominal wall cosmetic effect can be: a. very dissatisfied (score 1), b. dissatisfied (score 2), c. ordinary or not sure (score 3), d. satisfied (score 4), e. very satisfied (score 5) [7,8]
Statistical analysis: Statistics were processed by adopting SPSS (Statistical Product and Service Solutions) 17.0. Measurement data were indicated by mean standard deviation (). The mean difference of two samples conforming to normal distribution would be tested by t test. Unconformity to normal distribution would be the rank sum test of two independent samples. The comparison of rates would be tested by χ2test. The data would be indicated by sample case number(n). P<0.05 means difference is statistically significant
Results
General information
| Groups | Cases (n) | Sex (Male/Female) | Age | Body Mass Index (BMI) | |
|---|---|---|---|---|---|
| Male | Female | ||||
| Group A | 341 | 120 | 221 | 42.6 ± 10.9 Δ | 23.3 ± 1.3 Δ |
| Group B | 107 | 38 | 69 | 43.1 ± 11.5 | 23.5 ± 1.4 |
| P | 0.627 | 0.541 | 0.174 | ||
Table 1: Comparison of general information between two groups
Notes: Compared with Group B, the patients in Group A had no significant statistical difference in sex, age and BMI, ΔP>0.05, between the two groups were comparable.
Research results
| Groups | Cases (n) | Operation Time (min) | Bleeding Volume (ml) | Recovery Time of Intestinal Function (h) | Time of Hospitalization (d) |
|---|---|---|---|---|---|
| Group A | 341 | 34.8 ± 6.3Δ | 4.2 ± 1.3 Δ | 20.3 ± 4.1 Δ | 5.1 ± 1.2 Δ |
| Group B | 107 | 34.2 ± 5.8 | 5.1 ± 1.4 | 22.1 ± 4.3 | 5.4 ± 1.3 |
| P | 0.732 | 0.257 | 0.641 | 0.183 |
Table 2: Comparison of various research indicators between two groups
Notes: Compared with Group B, the patients in Group A had no significant statistical difference in operation time, bleeding volume in intraoperation, the recovery time of intestinal function and the time of hospitalization, ΔP>0.05.
| Groups | Cases (n) | Complications | ||||
|---|---|---|---|---|---|---|
| Bleeding | Bile Leakage | Incision Infection | Bile Duct Injury | Total Number | ||
| Group A | 341 | 2 | 0 | 3 | 1 | 6 Δ |
| Group B | 107 | 1 | 0 | 2 | 0 | 3 |
| P | 0.064 | |||||
Table 3: Comparison of post-operation complications between two groups
Notes: Compared with Group B, the patients in Group A had no significant statistical difference in the incidence of complications, ΔP>0.05.
| Groups | Cases (n) | Pain Scores | Grades of Abdominal Wall Cosmetic Effect |
|---|---|---|---|
| Group A | 341 | 3.05 ±1.09Δ | 4.3 ± 0.5▲ |
| Group B | 107 | 4.93 ± 1.47 | 3.6 ± 0.7 |
| P | 0.037 | 0.003 |
Table 4:Comparison of the recovery time for intestinal function and grades of cosmetic effect between two groups
Notes: Compared with Group B, patients in Group A had lower pain scores of post-operations, which had statistical significance, Δ P<0.05. About grades of abdominal wall cosmetic effect, Group A was significantly higher than Group B, ▲ P<0.01.
Illustration
Compared with Traditional Laparoscopic Cholecystectomy (TLC), Improved Mini-Laparoscopic Cholecystectomy (IMLC) had no significant statistical difference (P>0.05) (Table 1) in operation time, intraoperative bleeding volume, complications around the operation, hospitalization time and intestinal function recovery time (Tables 2 and 3). The patients post-operative pain score of IMLC (Group A) was lower than that of TLC (Group B) (P>0.05). The patients’ abdominal wall cosmetic effect score in Group A was obviously higher than that of Group B (P>0.01) (Table 4).
Analysis and Discussion
Surgery in 21st century is dominated by microtrauma and keeping moving forward. Under the premise of safety and effectiveness, small trauma and microtrauma is all the way the pursuit of surgeons. Relieving the patient’s suffering by minimum cost and maximum possibility [9-11].
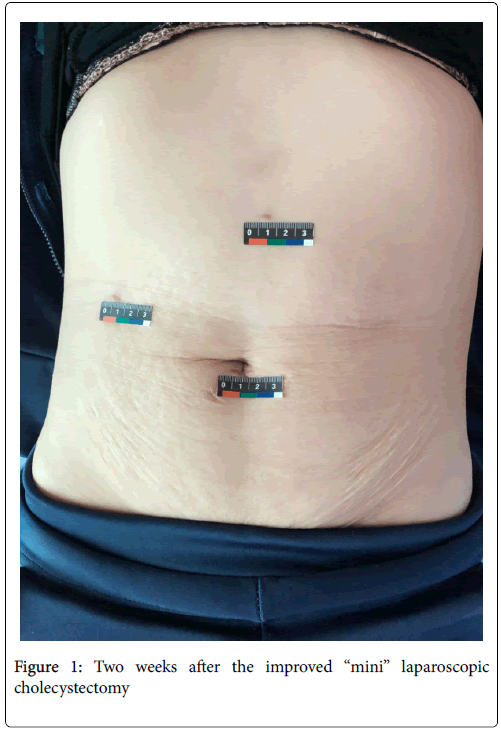
Gallbladder stones can be usually examined and accurately diagnosed by clinical symptoms, signs, abdominal colour Doppler ultrasound and imaging. Treatment approaches include conservative treatment and surgical treatment. In the past, the treatment for gallbladder stones was litholysis and smash. Yet, this treatment was almost eliminated for its unclear effect and its high risk. Now gallbladder stones and gallbladder benign lesions can be correctly diagnosed, conform to surgical indications and have no clear surgical contraindications, so surgical resection of lesions is the preferred treatment plan for them. Surgical approaches include traditional open surgery, small incision cholecystectomy and Laparoscopic Cholecystectomy (LC). Yet, LC is most popular and recommendable. Because LC has the advantage of microtrauma and better cosmetic effect, now it becomes the “gold standard” of treatment for gallbladder stones (Figure 1).
Traditional Laparoscopic Cholecystectomy (TLC) usually adopts 10mm Trocar as main operation hole for the surgery and needs post operation surgical suture, yet more obvious surgical scar will appear on the upper abdomen. Our hospital adopts Improved Mini Laparoscopic Cholecystectomy (IMLC). Its characteristics are as follows: (1) Adopting surgical tool 3mm or 5mm bellow, tiny wound, several months after surgery almost no surgical scars can be seen, good cosmetic effect and free from the intraoperative troubles of frequently loading and unloading Trocar converter. (2) In the intraoperation, using ribbon gauze and sample specimen bag, fine operation, less bleeding or almost no bleeding, gallbladder specimen sampling without incision pollution. (3) In the intraoperation, using 5mm Hemo- look clip, not the titanium clip, no metal foreign objects left in abdomen. By retrospectively analysing the information of our hospital’s hundreds of cases of cholecystectomy in the past four years, we get to know that IMLC is much better than TLC on the satisfaction of abdominal wall cosmetic effect and the postoperative pain. Pain has become the fifth vital sign after the four vital signs of temperature, pulse, breath and blood pressure [12]. Alleviating the patients’ painful discomfort is more conformable to the idea of Enhanced Recovery After Surgery (ERAS) [13], which is advocated at present. And it is more acceptable by patients.
Yet, IMLC still has its limitations and inadequacies. If the surgical instruments are more refined, it is more difficult to deal with the bleeding in intraoperation. Therefore, performing this operation needs a certain foundation of TLC. Carefully perform the operation to guarantee successful surgery and patient’s safety. Secondly, for some patients with cystic duct dilatation, the 5mm Hem-o-Lok clip can’t meet the requirements of clipping cystic duct. At this time, adopting the method of threading knotting to clip cystic duct, and this requires the surgeon to have enough technique of instruments performance and threading knotting under laparoscope. Special threading gauze and threading specimen bag are needed in intraoperation for using gauze strip and getting out gallbladder specimen and it increases the preparation time for surgery. At present, our hospital adopts homemade threading gauze and threading specimen bag, and now we are applying for national patent for them. We believe the finished products will come into market pretty soon and they will provide better material support for IMLC. We believe that with the improvement of the equipment’s and instruments and with the upgrade of surgeons’ surgical skills and experience, the technical adaptability of improved mini laparoscope will be gradually expanded promoted.
Authors Contribution
Zhang Feng and Qiao Song conceived and designed the research. Jiang Dayong, Ma Zhengbing, Bai Yuling and Teng Hong performed the operations. Zhang Feng wrote the paper. Jiang Dayong and Qiao Song reviewed and edited the manuscript. All authors are in agreement with the content of the manuscript
Funding
This research is funded by the general project of Tongren science and technology program(Scientific research of Tongren municipality (2017)47-4th).
References
- Yoo EH, Lee SY (2009) The prevalence and risk factors for gallstone disease. Clin Chem Lab Med 47: 795-807.
- CarusT (2013) Current advances in single port laparoscopic surgery. Langenbecks Arch Surg 398: 925-929.
- Culp BL, Cedillo VE, Arnold DT (2012) Single—incision laparoscopic cholecystectomy versus traditional four—port cholecystectomy. Proc(BaylUniv Med Cent). 25(4): 319-23.
- Beals DA(2002) Does minimal access mean minimal relationship? Defining the physician-patient relationship in postmodern culture.SeminLaparoscSurg9: 218-221.
- Kim BS, Choi WJ, Kim J, Lee JW (2013) Residual pain due to soft-tissue impingement after uncomplicated total ankle replacement. BoneJoint J 95: 378-83.
- Li Xing, Zhou Zhiying (2015) Evaluation of the Response of Adults and Adolescents toOrthodontic Tooth Pain by Visual Analogue Scale. China Continuing Medical Education 7: 150-151.
- Huang Chih-Kun (2010) Single-incision Trans-umbilical vs. Five-port Laparoscopic Roux-en-Y Gastric Bypass. Chin J Min InvSurg10:969-972.
- Li Dong, Zhou Xukun, Li Ping, Chengjun Wu, Shi Wang, et al. (2012) Comparison between Transumbilical Single-port and Three-port Laparoscopic Cholecystectomy for Calculous Cholecystitis. Chin J Min InvSurg12:20-23.
- Mouret P (1996) How I developed laparoscopic cholecystectomy. Ann Aead Med Singapore 25: 744-747.
- Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter D(2007) Surgery withoutscars:report of transluminal cholecystectomy in a human being. Arch Surg 142: 823-826.
- del Prete F, Nizegorodcew T,Regazzoni E (2012) Quantification ofsurgical trauma:comparison of conventional and minimallyinvasive surgical techniques for pertrochanteric fracture surgery based on markers of inflammation(interleukins).J OrthopTraumat01 13: 125-30.
- Levy N, Sturgess J, Mills P (2018) "Pain as the fifth vital sign" and dependence on the "numerical pain scale" is being abandoned in the US: Why? Br J Anaesth 120: 435-438.
- Wang Hui, Wang Jian (2017) Ambulatory laparoscopic cholecystectomy guided by enhanced recovery after surgery theory: areport of 1400 cases. J Hepatopancreatobiliary Surgery 29(1):6-9.
Citation: Dayong J, Feng Z, Song Q, Zhengbing M, Yuling B, et al. (2018) Clinical Application Research of the Improved “Mini” Laparoscopic Cholecystectomy. J Infect Dis Ther 6:371. DOI: 10.4172/2332-0877.1000371
Copyright: © 2018 Dayong J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3679
- [From(publication date): 0-2018 - Apr 19, 2025]
- Breakdown by view type
- HTML page views: 2874
- PDF downloads: 805