Case Report Open Access
Clear Cell Adenocarcinoma of Cervix: Radical Trachelectomy to Preserve the Fertility
Antoni Llueca*, Jose Luis Herraiz, Dolors Piquer, Yasmine Maazouzzi and Carmen Medina
Mutidisciplinary Unit for Abdomino-Pelvic Oncologic Surgery (MUAPOS), University General Hospital of Castellon, Department of Medicine, University Jaume I, Spain
- *Corresponding Author:
- Antoni Llueca
Mutidisciplinary Unit for Abdomino-Pelvic Oncologic
Surgery (MUAPOS), University General Hospital of Castellon
Department of Medicine, University Jaume I, Spain
Tel: 34 964 72 80 00
E-mail: antonillueca@gmail.com
Rec date: Mar 01, 2016; Acc date: Mar 22, 2016; Pub date: Mar 29, 2016
Citation: Llueca A, Herraiz JL, Piquer D, Maazouzzi Y, Medina C (2016) Clear Cell Adenocarcinoma of Cervix: Radical Trachelectomy to Preserve the Fertility. Adv Oncol Res Treat 1: 104. doi: 10.4172/2572-5025.1000104
Copyright: © 2016 Llueca A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oncology Research and Treatment
Introduction
Carcinoma of the uterine cervix is a common gynecologic malignant neoplasm all over the world. The most common histological type of malignant cervical neoplasms is squamous cell carcinoma [1,2]. Clear cell adenocarcinomas (CCAC) of the uterine cervix is a rare disease accounting for only 4% of all adenocarcinomas of the uterine cervix [3]. Primary CCAC of the uterine cervix is a rare neoplastic entity which occurs in young women exposed to DES in utero; primary CCAC without DES exposure in utero is extremely rare. Here we report a 23- years-old Spanish female with primary CCA of the uterine cervix with no maternal history of DES ingestion during pregnancy.
Case Report
A 23-year-old woman, nulligravida, without any coexisting disease, with negative familiar cancer history, presented irregular vaginal bleeding for last two months, sometimes as a menstruation and others as a spotting. Routine gynecological screening were normal (the last one was a year ago).
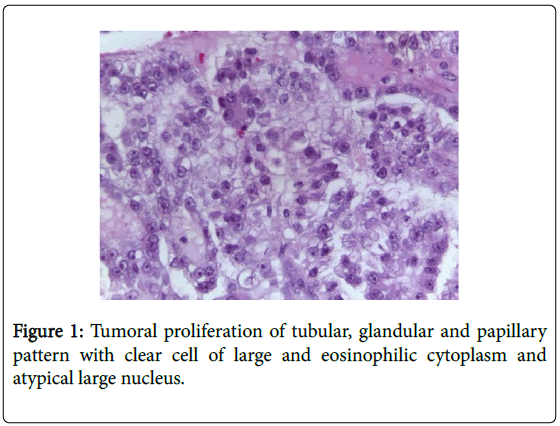
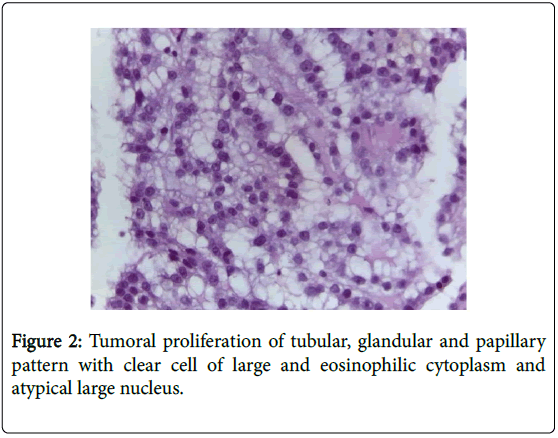
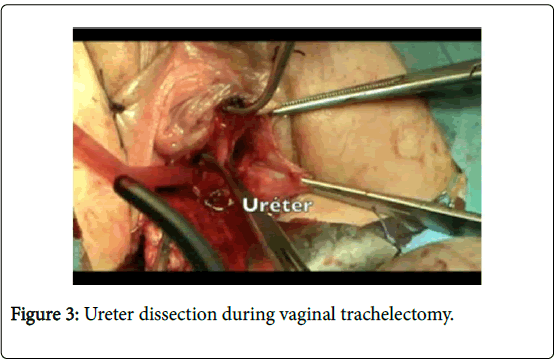
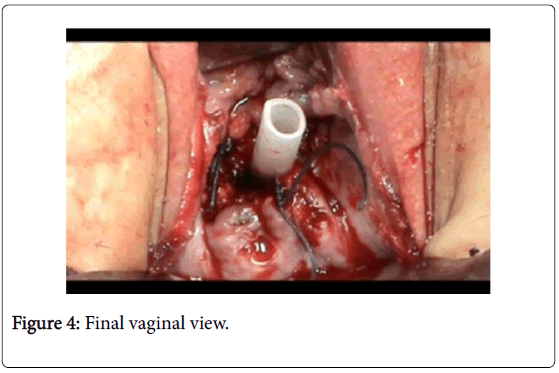
Exposure to DES was denied. Gynecological examination revealed cervical polypoid lesion of 3 x 0.5 cm. The patient underwent surgery for a cervical conization. Histopathological examination showed papilar and tubular proliferations and clear cell adenocarcinoma (Figures 1 and 2). All other biochemical, hematological and radiological tests were within normal limits. Contrast-enhanced computed tomographic scan did not reveal any suggestive lesion of malignancy. The patient was therefore diagnosed as a case of CCAC of cervix, FIGO stage IBI. She underwent radical trachelectomy of cervix (Figures 3 and 4) with bilateral pelvic lymph node dissection and both interiliac sentinel node. Sentinel node intraoperative results were negative. Histologically results were negative and there was no residual tumor at the cervix. FIGO stage IBI was confirmed. 18 months after the surgery, no signs of recurrence have been detected.
Discussion
Most cancers of the uterine cervix are squamous cell carcinomas, but the incidence of adenocarcinoma is rising in recent years and adenocarcinoma now accounts for about 20% of incidental invasive cervical cancers in screened populations worldwide [3,4]. CCAC of the cervix is a rare tumor accounting for only 4% of all adenocarcinomas of the uterine cervix.
There were an increased incidence between 1970-1980 of CCAC and a causal association was established with DES exposure. DES was used to reduce the complications of pregnancy like toxaemia (bleeding, premature birth and neonatal death) [5]. Median age of DES related clear cell carcinoma is 18.9 years. Primary clear cell carcinoma without any previous history of DES exposure is an extremely rare neoplasm. Median age of clear cell carcinoma non- associated with DES exposure is 53 years and it commonly presents with irregular vaginal bleeding (80%) [6].
The absence of specific symptoms, as in our patient, makes the diagnosis more difficult. The current diagnostic methods could be less effective. These factors together could delay the correct diagnosis and worsen the prognosis for patients [2,7].
Surgical resection is important for survival. Although radiotherapy is commonly used instead of surgery to treat adults with cervical cancer, surgery should be considered the treatment of choice for children or young adolescents due to the risk of radiation brosis of the bladder and bowel loop [8]. Carboplatin and paclitaxel regimens have comparable response rates for the treatment of advanced adenocarcinoma of the cervix without toxicity [9].
The selection criteria for radical trachelectomy are a desire for pregnancy, confirmed diagnosis of cervical cancer (any histological type except for neuroendocrine tumour and sarcoma), tumour size equal to or less than 2 cm, less than 50% stromal invasion, FIGO stage IA1 with LVI, IA2 or IB1, absence of any evidence of metastasis in or away from the pelvic lymph nodes, and age under 40 years [10,11].
Dargent et al. [12] first described “fertility sparing” trachelectomy for women with cervical cancers less than 2 cm [12]. Our patient is in her reproductive years so conservative management of early-stage cervical carcinoma is the best option. Recurrence and death rates (4.2% and 2.8%, respectively) of radical vaginal trachelectomy (RVT) seem to be comparable to classical radical abdominal hysterectomy. It appears that RVT's overall recurrence and death rates were similar to early-stage cervical cancer treated by radical hysterectomy or radiotherapy. Furthermore fertility results of RVT seem to be promising. A 70% pregnancy rate was reported in the women who wanted to conceive following RVT, though such patients should be informed about the risk of second trimester loss and preterm delivery [13-16].
In conclusion, in young patients with early stages CCAC of the cérvix without risk factors a fertility sparing approach could be considered as one of the options of treatment.
References
- Chaudhuri T, Sharma D (2012) Primary clear cell adenocarcinoma of the uterine cervix in young woman not associated with dietylestilbestrol: A case report and review of literature. Clin Cancer Investig J 1:239-241
- Gottwald L (2012) Clear cell adenocarcinoma of the uterine cervix in a 24-year-old woman. Case report and review of the literature. Arch Med Sci 8:578-581
- Young-Lan L (2012) A case of clear cell adenocarcinoma in the uterine cervix of 52- year-old virgin. Korean J Obstet Gynecol 55: 192-196.
- Herbst AL, Anderson D (1992) Clear cell adenocarcinoma of cervix and vagina and DES-related abnormalities. In: Coppleson M (2ndedn) Gynecologic oncology. London, pp: 1-523.
- Herbst AL, Ulfelder H, Poskanzer DC (1971) Adenocarcinoma of the vagina. Association of maternal stilbestrol therapy with tumor appearance in young women. N Engl J Med 284: 878-881.
- Lee YL, Chang KH, Kyung MS, Kim HB, Park SH (2012) A case of clear cell adenocarcinoma in the uterine cervix of 52 year old virgin. Korean J Obstet Gynecol 55: 192-196.
- Quinn MA (1998) Adenocarcinoma of the cervix. Ann Acad Med Singapore 27: 662-665.
- Choi SJ, Kim JE, Kim HM, Choi HY (2013) Clear Cell Adenocarcinoma of the Uterine Cervix in a 15-Year-Old Girl: A Case Report. J Korean Soc Radiol 69: 321-325.
- Singh P, Nicklin J, Hassall T (2011) Neoadjuvant Chemotherapy followed by radical vaginal trachelectomy and adjuvant che-motherapy for clear cell cancer of the cervix: a feasible ap- proach and review. Int J Gynecol Cancer 21:137-140
- Iacoponi S, Diestro MD, Zapardiel I, Serrano M, Santiago JE (2013) Vaginal laparoscopically assisted radical trachelectomy in cervical clear cell adenocarcinoma. Ecancermedicalscience 7: 373-380.
- Ashton E, Brown A, Hoffman J, Khutti S (2013) Clear cell adenocarcinoma of the uterine cervix in an 18 year-old pregnant female. Gynecologic Oncology Case Reports 5: 49-51.
- Dargent D, Brun JL, Roy M (1994) La trachelectomie elargie (TE), une alternatie a l'hysterectomie radical dans le treatment des cancers infiltrants develops sur la face extreme du col uterin. J Obstet Gynaecol 2: 285-292.
- Dursum P, LeBlanc E, Nogueira MC (2007) Radical vaginal trachelectomy (Dargent’s operation): A critical review of the literature. EJSO 33: 933-941.
- Plante MC, Renaud IA Hoskins F (2005) Vaginal radical trachelectomy: a valuable fertility-preserving option in the management of early-stage cervical cancer: a series of 50 pregnancies and review of the literature. Gynecol Oncol 98: 3-10.
- Kim CH (2012) Reproductive outcomes of patients undergoing radical trachelectomy for early-stage cervical cancer. Gynecologic Oncology 125: 585-588
- Korhonen MO (1984) Adenocarcinoma of the uterine cervix. Prognosis and prognostic significance of histology. Cancer 53: 1760- 1781.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13439
- [From(publication date):
June-2016 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 12470
- PDF downloads : 969