Chronic Pain Pre-Surgical Assessments and Follow-Up Case Study
Received: 31-Jul-2017 / Accepted Date: 21-Aug-2017 / Published Date: 28-Aug-2017 DOI: 10.4172/2155-6105.1000341
Abstract
The case of a 47 year old male that was assessed for readiness for a spinal cord stimulator trial procedure is presented to illustrate alternatives to narcotic medication treatment for chronic pain. An overview of the assessments administered is given. Twelve weeks of cognitive behavioral treatment is summarized. Summary comments highlighting the advantage of consideration of alternatives to narcotic prescriptions for chronic pain treatment are made.
Keywords: Non-pharmacological treatment of chronic pain; Cognitive behavior therapy for pain management; Alternatives to pharmacological treatment of chronic pain; Chronic pain
Introduction
Traditional treatments for chronic pain are pharmacological interventions. Over the counter medications such as acetaminophen and NSAIDs are used initially as a pharmacological treatment for pain. However, when the pain experience exceeds a six-month period and subjective ratings and sometimes medical metrics of the pain prompt more intensive treatments using narcotic medications are implemented. This category of medicines, while useful medical treatments, are being widely abused. The United States government agency, the Center for Disease Control has issued a limitation on the prescribing of narcotic medications for pain management to address the abuse problem. This circumstance has prompted attention to alternative treatments for chronic pain. Clinical Psychologists working in medical settings and primary care facilities often receive referrals to assess pain patient’s coping with their chronic illness, their use (as prescribed or otherwise) of their medications and their readiness to consider other treatments for their chronic pain. A case report is presented to illustrate this pathway.
Case Report
A 47 year old Hispanic male was referred to Psychological services of a pre-surgical evaluation for the Spinal Cord Stimulator (SCS) trial procedure[1]. These evaluations entail the assessment of the patient’s coping with their pain, their understanding of their care and of the Spinal Cord Stimulator trial procedure. This individual was provided with a DVD by the spinal cord stimulator company, a brief meeting with a representative of the company as well as a discussion with his pain physician about the SCS. The patient had worked the last 23 years both fulltime and overtime as a cabinet installer. His company had contracts in private homes and in industry. The cabinets varied to a small degree but entailed some light assembly before the mounting on the wall. Approximately 60% of the mountings were overhead. The cabinets ranged in sizes and weights (50-200 pounds). The patient started at a Pain clinic eight years ago, this assessment/pain clinic care is his second pain clinic experience. He left the first pain clinic when after seven years of treatment they reduced and then discontinued his pain medications. The patient presented with excruciating, constant pain that started 13 years ago, He denied trauma, work accident or car accident onsets to the pain. He received a diagnosis of Degenerative Disc Disorder and was prescribed pain medications[2]. The patient maintained compliance on the medication regime he was prescribed. While compliant, the patient expressed dissatisfaction with pain relief from alternative treatments such as pain medicine injections and radio wave nerve corduroying. Also during this time, his job position responsibilities increased and the amount of assistance decreased thus placing him in a daily position of hanging heavy cabinets with little or no assistance. A short time later the patient was laid off from his position. The patient has been out of work for three years. The patient is married thirty one years and has two children aged 13 and 10 years. His wife works at the hospital as a nurse’s aid. The patient has extended family that lives nearby. He reports trying and being denied social security disability income. Since he has been at home the last three years, he reports feeling worse than the times when he worked. He has difficulty moving out of bed in the morning, sitting, standing and walking for distances more than one block. The patient reports sitting and viewing television most of his day when not going to doctors’ appointments. The patient’s pain medications were reduced by 60% over the last ten months. The patient reported current pain at 10/10 and dissatisfaction with his reduced pain medication regime[3]. The patient has medical conditions of diabetes mellitus type II, hyperlipidemia and hypertension that are controlled with medications. The patient reports severe sleep disturbance. The patient’s sleep history is positive for fragmented sleep during the years he works. Once he was at home with the layoff from work, he found himself sleeping in 1-2 h intervals with 2-3 h of wakefulness in between. He reported constant lethargy and fatigue. The patient’s BMI is 28. The patient has had three spinal stabilization surgeries. The patient denied nicotine and recreational drug use; he reported mild alcohol use.
Assessment and Follow-Up
A structured Pain Interview, several pain perception self-report measures, fatigue scale, opioid abuse scale, disability scale were used in the assessment. The patient was compliant with the assessment. Recommendations were made for the patient for pain management and cognitive behavioral therapy (CBT) for sleep disturbance. The patient was considered to be a good candidate for the SCS trial procedure. After the five day SCS trial procedure, the patient underwent the surgery to implant a SCS. He reported a reduction in his pain ratings to 6/10 following the procedure. He reported movement and some activity as a result of the pain relief - he walked to visit neighbours, played dominoes on the patio of his home with friends and family and on one occasion, drove to pick up his children from school. The patient is currently under consideration for a second SCS in another area of his spine where the degeneration is severe[4].
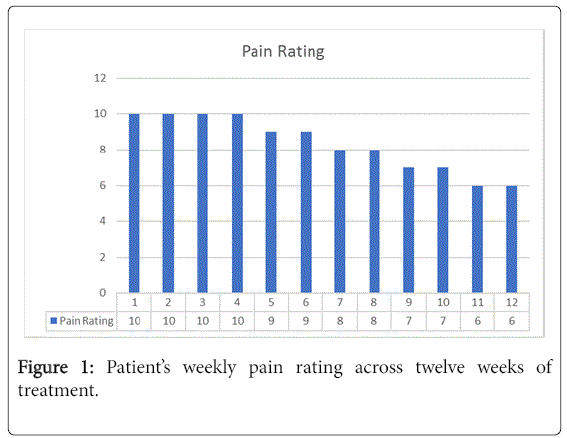
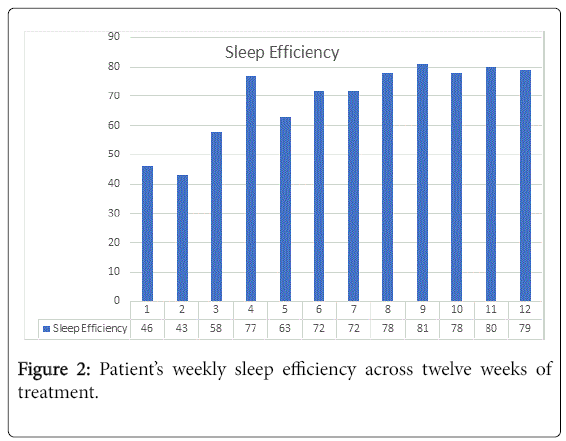
The patient responded to the pain management and CBT for his sleep weekly for twelve weeks. The cognitive behavioral therapy approaches to sleep and pain problems entails the use of an educative stance to providing information and behavioral assignments. The patient was asked to track his sleep and pain levels daily during this treatment period. Weekly CBT sessions focused on the behavioral problems of managing his pain and sleep. For example, he was taught the relaxation skill of mindfulness by instruction and trial during the sessions and assigned practice between sessions. Also, therapy discussion points of the use of sleep hygiene and distraction technique of small physical/emotional/cognitive tasks for distraction from pain were presented. Home practice and continued logging of sleep and pain ratings were employed. He willingly tracked his pain ratings and tried the relaxation exercises. He modified his bedtime and sleep schedule in general with no daytime sleeping. He complied with the behavioral assignments from both the pain management therapy and the CBT. For example, he took to playing checkers once a day with a friend during the afternoons. This small event became something he looked forward to and expanded to his continuing to play checkers with his oldest child when she came home from school. Figure 1 represents his daily pain ratings at pre-treatment (weeks 1-2), during treatment (weeks 3-8) and post intervention (weeks 9-12). In Figure 2, sleep efficiency was computed from his sleep logging and is presented in terms of the pre-treatment (weeks 1-2), during treatment (weeks 3-8) and post treatment intervals (weeks 9-12).
Clinical Issues
The Centers for Disease Control and Prevention issued new guidelines in 2017 that opioids should not be the first line or only treatment for patients who present with chronic non-cancer pain. A reduction in primary care physician’s prescriptions for opioid medications cascading the demand and eventual reduction in prescriptions of opioids in pain clinics. This circumstance presented health care practitioners with an increasing number of patients with addiction to opioid medications. The compulsive uncontrollable craving for the medication to combat the pain left many patients to dire circumstances (e.g. increased emergency room visits, seeking recreational drugs, increased alcohol and over the counter medications, doctor shopping). Additionally, a grave number of patients were untreated with the mandated reductions in opioid medications cited as the reason.
Pain patient suffer from poor sleep quality. The depressed mood secondary to the chronic pain and reduced social/emotional/physical activity is related to the poor sleep quality. A common, secondary reason for poor sleep quality in pain patient is sleep position. Patients report waking from sleep and difficulty falling asleep due to flare-ups and soreness from the immobility once in various sleep positions. The third common reason for poor sleep quality in pain patients is the erratic sleep schedules due to sedation properties of pain medications and the chronic pain, many feel the need to nap during the day and erode their sleep need.
Conclusion
The volume of pain patients needing non-opioid/behavioral treatment is increasing. The number of new cases will present challenges to the Addictions counsellor/facility for treatment management. With the new mandates for reductions in pain medication regimes, it is plausible that pain patients may need assistance from professionals trained in the care of addictions. Interprofessional communications in terms of referrals for care, as illustrated in this case of pain medicine referral to psychology services, provides an example of a common goal-patient health.
References
- Brown GK (1990) A causal analysis of chronic pain and depression. ‎J Abnorm Psychol 99: 127-37.
- The CDC provides crucial new guidance on opioids and pain. National institute on drug abuse advancing addition science.
- Sayar K, Arikan M, Yontem T (2002) Sleep quality in chronic pain patients. Can J Psychiatry 47: 844-848.
- Sexton-Radek K, Graci G (2008) Combating your sleep. New York: Pergamon Press.
Citation: Radek KS (2017) Chronic Pain Pre-Surgical Assessments and Follow-Up Case Study. J Addict Res Ther 8: 341. DOI: 10.4172/2155-6105.1000341
Copyright: © 2017 Radek KS. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3623
- [From(publication date): 0-2017 - Dec 22, 2024]
- Breakdown by view type
- HTML page views: 2978
- PDF downloads: 645