Chronic Cough Caused By an Intra-Abdominal Bronchogenic Cyst: A Case Report and Literature Review
Received: 21-Apr-2018 / Accepted Date: 08-May-2018 / Published Date: 11-May-2018 DOI: 10.4172/2161-0711.1000611
Abstract
Introduction: Bronchogenic cyst is an extremely rare congenital abnormality that is incidentally found by imaging during health check-up. They can hardly occur in the abdomen with unspecific symptoms or change in laboratory values. Case presentation: Here in, we are going to report a case of a 33 years old male patient who was admitted in our department for an intra-abdominal mass. Pathological result of the resected mass was bronchogenic cyst. Conclusion: In most of the cases, bronchogenic cysts are misdiagnosed. The use of endoscopic ultrasound guided fine needle aspiration, computed tomography guided needle biopsy or intraoperative frozen section biopsy is helpful in confirming their diagnosis and to choose the most appropriate treatment.
Keywords: Intra-abdominal bronchogenic cyst; Imaging; Congenital disease; Endoscopic ultrasound guided fine needle aspiration; Intraoperative frozen section biopsy
Introduction
Bronchogenic cyst (BCS) is a rare type of congenital abnormality that occurs in the primitive foregut during early embryogenesis. They are thought to develop before the formation of the diaphragm due to an abnormal budding of the tracheobronchial tree and getting displaced in the abdomen [1]. As they don’t have any connection with the respiratory tract, they are considered to be congenital cysts. BCS are mostly found in the thorax and mediastinum, their occurrence in the abdominal cavity is extremely rare [1,2].
Here we are going to report our experience with a patient who had bronchogenic cyst and was admitted in our department for surgery. In this paper, we also discuss the features of BCS, the Radiology, Embryology, Histology and treatment options, which could be helpful for early diagnosis and treatment of BCS.
Case report
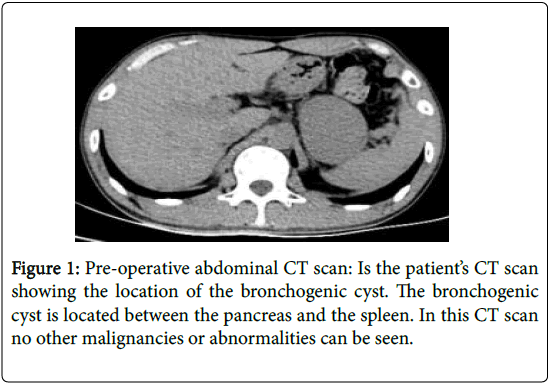
A 33 years old male patient was admitted in our department because of an intra-abdominal mass which was found by CT scan (Figure 1) during his health check-up for a dry and intermittent chronic cough which he had for past 23 years. The mass (size 8 cm × 6 cm) was located between the tail of the pancreas and spleen.
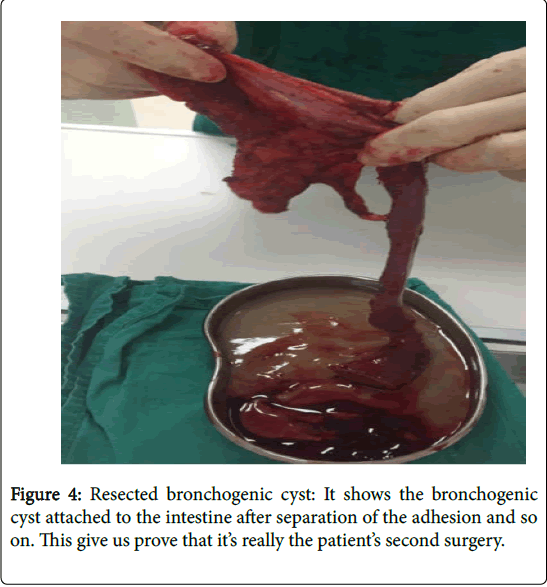
23 years ago, after a traumatic abdominal injury the patient went to local hospital for treatment. Abdominal CT scan revealed an intraabdominal mass located between the tail of the pancreas and spleen. He was diagnosed as pancreatic pseudo cyst and underwent pancreatocystojejunostomy surgery. After the injury, the patient had chronic intermittent cough for which he was given medications but did not get better. Abdomen Inspection showed a surgical scar of about 10 cm along the midline of the abdomen. A 5 cm × 4 cm soft, non-mobile and painless mass was palpable in the upper left quadrant of the abdomen. The laboratory results were within the normal range and no abnormalities were found in mediastinum CR and CT scan.
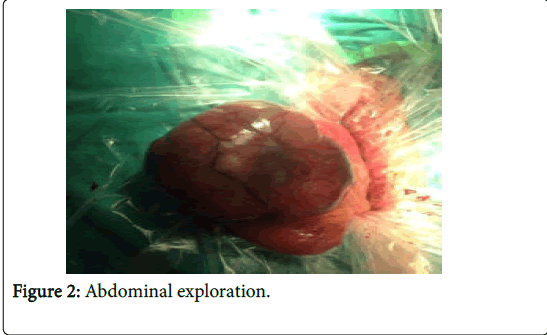
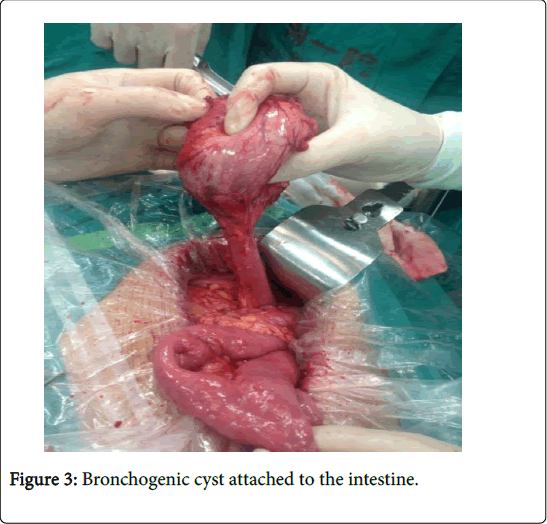
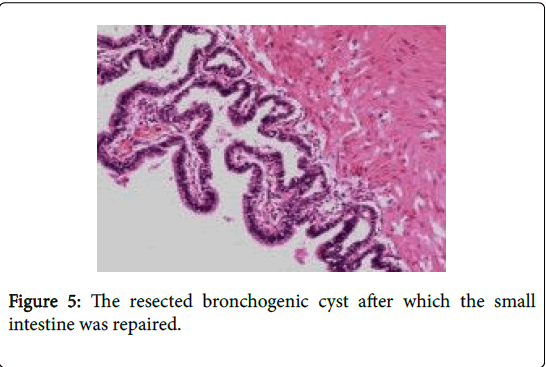
During exploratory laparotomy, we found that the pancreas and spleen was normal, there was no distant metastasis, an 8 cm × 6 cm pink colored, soft mass which was anastomosed to the jejunum (Figures 2 and 3) was found. The mass and the anastomosed jejunum was resected; the remaining small intestine was repaired. The gross appearance of the resected specimen was a benign cyst. When the mass was opened, it revealed to be a large cystic cavity filled with grayish mucoid fluid (Figure 4). It was then sent for pathological study and the result was a bronchogenic cyst (Figure 5).
After the surgery, the patient did not had cough and the postoperative course was uneventful. The patient was discharged at 7th day postoperatively and came for checkup after three months; he remained asymptomatic for six months.
Discussion
BCS usually arises from the ventral foregut during the third to seventh week of the fetal development. During this period of development, the thoracic and abdominal cavities are connected by pericardio-peritoneal canal. But when the Pleuroperitoneal membrane fuses to form the trachea, bronchus and diaphragm, the canal is separated.
If there is an abnormal fusion of the membrane, a portion of the tracheobronchial tree may pinched off and migrate to different locations (from mouth to anus) to form bronchogenic cysts [3]. Histologically, BCS contain normal bronchial tissue such as PSCCE, mucus gland, smooth muscle fiber, fibrous tissue, elastic tissue and cartilage but very few cysts consist of all these components at the same time [4].
Most of the BCS are incidentally found during health checkups and imaging is the most common method for their findings. CT scan, MRI, or Ultrasound can be used to check for the presence of an abdominal cystic lesion or mass, but often it’s difficult to identify their nature because of their thick walls (Figure 1) and irregular shape. As there are no specific symptoms or typical changes in laboratory results, CT scan is helpful in making a diagnosis. In cases where the cysts have thin wall, CT scan can even determine the cystic contents and enable us to think for further differential diagnosis [5]. BCS contain protein rich fluid which makes them to have a high range of CT value (30 to 100 HU). On CT images, typical BCS are observed as a mass with a smooth surface, clear margin and with homogenous density in internal region [4]. On MRI scan in T1 weighted images, BCS present as a cystic mass with slightly hyper- or iso-intense to skeletal muscle. On the T2 weighted images, they are either hyper- or iso-intense to cerebrospinal fluid [6].
Endoscopic ultrasound (EUS) is another tool that can be helpful in identifying the gastrointestinal intramural or extramural BCS. EUS guided fine needle aspiration (EUS-FNA), CT guided needle biopsy and intra-operative frozen section diagnosis can help us to confirm the nature of the cyst by the presence of pseudo stratified ciliated columnar epithelium (PSCCE) and the absence of neoplastic cells. Some people do not advise to perform biopsy because it is difficult to target the thin wall of a BCS exactly and it also have high risk of complications like dissemination of tumor and hemorrhage [4].
The management of bronchogenic cysts is still controversial because most of the cases are diagnosed post-operatively. Watchful and waiting is suggested if the benign nature of the cyst is confirmed by the presence PSCCE in EUS-FNA biopsy. Sato et al. [7]. Reported a case of gastric bronchogenic cyst which was diagnosed by EUS-FNA biopsy. Cytological evaluation of the aspirate was benign PSCCE with a mucinous background, so surgery was not chosen as treatment. Similarly, a case of a 26 years old Swedish male patient who came to seek medical help because of epigastric pain was reported by Rubio et al. [8]. The patient received a gastroscopy and biopsy of the corpus showed an intramural cyst lined with PSCCE, the patient was prescribed omeprazole and the symptoms disappeared. If EUS-FNA confirm the diagnosis of BCS, surgery is not mandatory for these patients.
In cases where the nature of the cyst cannot be identified preoperatively or if the cyst is communicating or adhering to the alimentary canal, it should be resected as it can easily cause infection, ulceration, perforation, bleeding, fistula formation, obstruction, and they have even been linked to malignancy changes [9]. Similarly Ubukata et al. [10]. Reported a case of an 81 years old woman who was asymptomatic but came to hospital for a physical check-up and found to have a cystic mass attached to the lesser curvature of the stomach. The initial diagnosis was congenital cyst without malignant component but the patient opted for surgery and the post-operative diagnosis was bronchogenic cyst.
Our patient had a unique history of coughing for 23 years which resolved after surgery. Since literature review showed that there is no link between the tracheobronchial tree and bronchogenic cyst [1], the relationship of coughing and intra-abdominal bronchogenic cyst was questioned. For answers, we searched for all cases with intraabdominal bronchogenic cysts with similar histology, but none of the patient had the same symptom. We speculated that, the injury made the mass to be more mobile or with time the mass has grown which caused the diaphragm to press against the cyst, which was stimulating it and causing the patient to cough.
Conclusion
Bronchogenic cyst is a rare congenital entity which is lined by PSCCE and derived from ventral foregut during the period of embryogenesis. The clinical manifestation is unspecific and so it can be easily misdiagnosed. EUS-FNA/CT-guided needle biopsy or intraoperative frozen section biopsy can be helpful in confirming their diagnosis and allow us to choose the correct therapeutic approach.
Informed Consent
Ethical approval was obtained from the ethics committee of first affiliated hospital of Wenzhou medical university. Informed consent was obtained from the patient for publication of this case report and any accompanying images.
Funding
Doctor startup fund and Yuying project of the second affiliated hospital of Wenzhou Medical University (216200) and research fund for Lin He’s Academician workstation of new medicine and clinical translation (17331105).
References
- Kurokawa T, Yamamoto M, Ueda T, Enomoto T, Inoue K, et al. (2013) Gastric bronchogenic cyst histologically diagnosed after laparoscopic excision: Report of a case. Int Surg 98: 455-460.
- Ishizuka O, Misawa K, Nakazawa M, Nishizawa O (2004) A retroperitoneal bronchogenic cyst: Laparoscopic treatment. Urol Int 72: 269-270.
- Menke H, Schmeer T, Horcic M, Meier R, Maurer CA (2009) Bronchogenic cyst: A rare cause of a retroperitoneal mass. Eur J Surg 163: 311-314.
- Ryan AG, Zamvar V, Roberts SA (2002) Iatrogenic candidal infection of a mediastinal foregut cyst following endoscopic ultrasound-guided fine-needle aspiration. Endoscopy 34: 838-839.
- Kajiya Y (1977) Retroperitoneal foregut cyst. Abdom Imaging 22: 111-113.
- Choi KK, Sung JY, Kim JS, Kim MJ, Park H, et al. (2012) Intra-abdominal bronchogenic cyst: Report of five cases. Korean J Hepatobiliary Pancreat Surg 16: 75-79.
- Sato M, Irisawa A, Bhutani MS, Schnadig V, Takagi T, et al. (2008) Gastric bronchogenic cyst diagnosed by endosonographically guided fine needle aspiration biopsy. J Clin Ultrasound 36: 237-239.
- Rubio CA, Orrego A, Willén R (2005) Bronchogenic gastric cyst. A case report. In Vivo 19: 383-385.
- Kim KH, Kim JI, Ahn CH, Kim JS, Ku YM, et al. (2004) The first case of intraperitoneal bronchogenic cyst in Korea mimicking a gallbladder tumor. J Korean Med Sci 19: 470-473.
- Ubukata H, Satani T, Motohashi G, Konishi S, Goto Y, et al. (2011) Intra-abdominal bronchogenic cyst with gastric attachment: Report of a case. Surg Today 41: 1095-1100.
Citation: Chandoo A, Wu RS, Peng ZY, Xin L, Wang-Kai X, et al. (2018) Chronic Cough Caused By an Intra-Abdominal Bronchogenic Cyst: A Case Report and Literature Review. J Community Med Health Educ 8: 611. DOI: 10.4172/2161-0711.1000611
Copyright: © 2018 Chandoo A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5141
- [From(publication date): 0-2018 - Dec 20, 2024]
- Breakdown by view type
- HTML page views: 4419
- PDF downloads: 722