Choroidal Metastasis as a First Sign of Recurrence in a Patient with Breast Cancer: A Case Report
Received: 09-Sep-2016 / Accepted Date: 23-Sep-2016 / Published Date: 30-Sep-2016 DOI: 10.4172/2572-4118.1000112
Abstract
Choroidal metastasis is the most frequent ocular tumor. Due to its high vascularity, the choroid is particularly susceptible to hematogenous dissemination of cancer cells. The most common primary tumors in choroidal metastasis are located in the lung for men and the breast for women. We report a patient followed for breast cancer treated in June 2005. She was asymptomatic until February 2016, when she presented a progressive decrease in left eye’s visual acuity and headache. Funduscopic examination showed a left exudative retinal detachment. The brain Magnetic resonance imaging revealed a left choroid metastasis. The total body computer tomography scan showed a many lung, liver, peritoneal and bone metastases. The symptoms were improved after whole-brain radiotherapy and first line systemic chemotherapy based on Bevacizumab and weekly Paclitaxel.
Keywords: Breast cancer; Choroidal metastasis; Tumor; Primary breast malignancy; Chemotherapy
35905Introduction
Choroidal metastasis is the most frequent ocular tumor. Due to its high vascularity, the choroid is particularly susceptible to hematogenous dissemination of cancer cells [1]. The most common primary tumors in choroidal metastasis are located in the lung for men and the breast for women [2]. Choroidal metastases usually appear late and are generally a sign of advanced metastatic disease and poor prognosis [3]. The most common symptom of choroidal metastasis is the progressive decrease in visual acuity [2]. We report a case of choroid metastasis which was the first sign of systemic dissemination of the disease.
Case Report
We present the case of a 61-year-old Caucasian woman diagnosed with non-metastatic infiltrating ductal carcinoma in the right breast in June 2005. The Clinicopathologic characteristics of the tumor were: T2N2M0, Hormonal Receptor (RH) positive, human epidermal growth factor 2 receptor (HER2) negative. She was treated with radical right mastectomy with homolateral axillary lymphadenectomy completed by adjuvant systemic chemotherapy based on a sequential anthracyclinetaxan regimen followed by locoregional RT encompassing the chest wall and sus clavicular regional lymph nodes. She had two years of adjuvant hormonotherapy based on Tamoxifen 20 mg per day, followed by three years of Aromasine 25 mg per day, completed in April 2013.
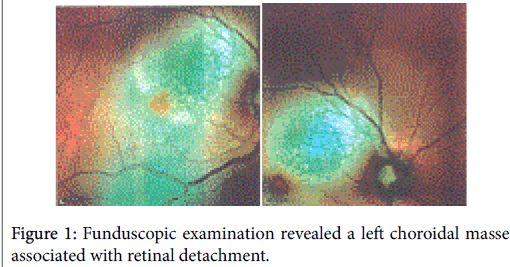
She was asymtomatic until February 2015, when she presented a progressive decrease in left eye’s visual acuity and headache. The Ophthalmological examination showed a visual acuity at 8/10 in the right eye and 4/10 in the left eye. The biomicroscopy of the anterior segment was normal. Funduscopic examination showed a choroidal masse associated with exudative retinal detachment (Figure 1).
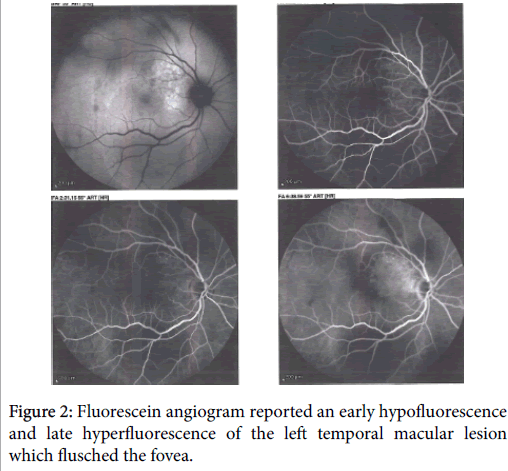
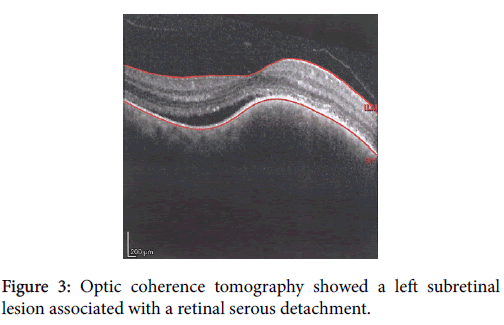
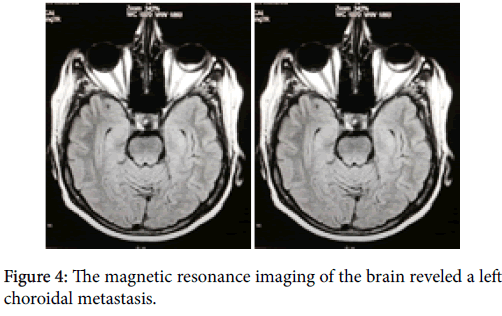
Fluorescein angiogram reported an early hypofluorescence and late hyperfluorescence of the left temporal macular lesion which flusch the fovea (Figure 2). Optic coherence tomography showed a left subretinal lesion associated with a retinal serous detachment (Figure 3). The magnetic resonance imaging of the brain revealed a left choroid metastasis (Figure 4).
The total body computer tomography scan showed a many lung, liver, peritoneal and bone metastases. The left eye’s vision was progressively improved after whole-brain radiotherapy according to the schedule: 30 Gy in 10 fractions, and first line systemic chemotherapy based on Paclitaxel at 90 mg/m2 weekly for three doses with one week rest (28-day cycle) in combination with bevacizumab 10 mg/kg every 14 days. The first radiological evaluation, done after three cycles, showed a partial response according to Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. The patient is still alive, she is asymptomatic and continues its palliative chemotherapy.
Discussion
Common metastatic sites of breast cancer are the bone, lung, liver and brain. Choroidal metastatic disease is rare from a primary breast malignancy and it's the most frequent ocular tumor [1]. The incidence of ocular metastasis from breast cancer ranges from 3 to 30% [4,5]. The choroid is often the most affected (89%) followed by the iris (9%) and ciliary body (2%) [1]. Bilateral Choroidal metastases were observed in 20% [1]. Clinical signs depend on the localization and the extent of the choroidal metastasis, The most common symptoms are the progressive decrease in visual acuity and the blurred vision but other symptoms may be present, such as eye pain, retinal detachment, phtophobia, diplopia, exophtalmos, and apoptosis [6,7]. Choroidal metastases usually appear late and are generally a sign of advanced metastatic disease and poor prognosis [3]. In a report by Sánchez et al. they described the case of a 47-year-old woman, treated for breast cancer seven years ago, with progressive vision loss due to retinal detachment secondary to choroidal metastasis in the right eye. These symptoms were the first sign of her breast malignancy’s recurrence [8]. The diagnosis of a choroidal metastasis is based on ophthalmoscopy and imaging techniques: B-mode ultrasonography, fluorescein angiography, Optic coherence tomography [1]. Biopsy choroidal lesion is essential, when the choroidal metastasis is isolated, and in the absence of a primary neoplasm [9]. Treatment of choroidal metastasis depends on the patient’s general condition and presence of metastases to other organs. Therapeutic arsenal include external beam radiotherapy (EBRT), systemic treatment (chemotherapy and hormone therapy), enucluation, transpupillary thermotherapy, local resection, photocoagulation, and cryotherapy [6]. In the case reported above, the symptoms were improved after whole-brain radiotherapy and first line systemic chemotherapy based on Bevacizumab and weekly Paclitaxel.
Conclusion
Visual trouble in a patient with history of breast cancer may hide a choroidal metastasis. It’s the first sign of breast malignancy’s recurrence in many cases reported in the literature. Therapeutic decision must be discussed in a multidisciplinary meeting between oncologist, radiotherapist, ophthalmologist and radiologist.
Conflict of Interest
The authors declare that they have no conflict of interests.
Author’s contribution
Youssef Seddik performed literature review, composed this case report and manuscript writing. All authors read and approved the final manuscript.
References
- Shields CL, Shields JA, Gunduz K, Cater J, Mercado GV, et al. (2000) Conjunctival melanoma: risk factors for recurrence, exenteration, metastasis, and death in 150 consecutive patients. Arch. Ophthalmol 118: 1497-1507.
- Ferry AP, Font R (1974) Carcinoma metastatic to the eye and orbit I. A clinicopathologic study of 227 cases. Arch Ophthalmol 92: 276-86.
- Volpe NJ, Albert DM (1994) Metastasis to the uvea. In: Albert DM, Jakobiec FA, editors. Principles and practice of ophthalmology. Philadelphia: WB Saunders p: 3260-70.
- Merril CF, kaufman DI, Dimitrov NV (1991) Breast cancer metastatic to the eye is a common entity. Cancer 68: 623-627.
- Fenton S, Kemp EG, Harnett AN (2004) Screening for ophthalmic involvement in asymptomatic patients with metastatic breast carcinoma. Eye 18: 38-40.
- Dobrowsky W (1988) Treatment of choroid metastases. Br J Radiol 61: 140-142.
- Aragão RE, Barreira IM, Gomes LM, Bastos AS, Beserra Fde F (2013) Choroidal metastasis as the first sign of bronchioloalveolar lung cancer: case report. Arq Bras Oftalmol 76: 250-252.
- Sánchez R, Betancourt L, Sánchez A (2008) Choroidal metastasis as first manifestation of systemic recurrence of breast cancer. Breast J 14:498-500.
- Eide N, Syrdalen P, Walaas L (1999) Fine needle aspiration biopsy in selecting treatment for inconclusive intraocular disease. Acta Ophthalmol. Scand 77: 448-452.
Citation: Seddik Y, Brahmi SA, Al-Jarroudi O, Chacha R, Barabino AD, et al. (2016) Choroidal Metastasis as a First Sign of Recurrence in a Patient with Breast Cancer: A Case Report. Breast Can Curr Res 1: 112. DOI: 10.4172/2572-4118.1000112
Copyright: ©2016 Seddik Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 16722
- [From(publication date): 9-2016 - Jul 03, 2025]
- Breakdown by view type
- HTML page views: 15556
- PDF downloads: 1166