Research Article Open Access
Characterization of Selected Metabolic and Immunologic Markers Following Exclusive Enteral Nutrition of Pediatric Crohn’s Disease Patients
Viral Brahmbhatt1*, Ivan Montoliu1, Nabil Bosco1, François-Pierre Martin1, Phillipe Guy1, Manuel Oliveira1, Stephanie Schatz2, Katharina Werkstetter2, Eduardo Schiffrin1, Berthold Koletzko2, Jalil Benyacoub1 and Sibylle Koletzko21Research and Development, NESTEC LTD, Lausanne, Switzerland
2Pediatric GI, Dr. von Hauner Children's Hospital, Ludwig-Maximilians-University of Munich, München, Germany
- Corresponding Author:
- Viral Brahmbhatt
Nestlé Research and Development Centre India Pvt. Ltd.
CP-12A, Sector-8, IMT Manesar
Gurgaon, Haryana, 122050, India
Tel: +911244195525
E-mail: Viral.Brahmbhatt@rd.nestle.com
Received Date: August 01, 2016; Accepted Date: August 27, 2016; Published Date: August 31, 2016
Citation: Brahmbhatt V, Montoliu I, Bosco N, Martin FP, Guy P, et al. (2016) Characterization of Selected Metabolic and Immunologic Markers Following Exclusive Enteral Nutrition of Pediatric Crohn’s Disease Patients. J Gastrointest Dig 6:466. doi:10.4172/2161-069X.1000466
Copyright: © 2016 Brahmbhatt V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Objectives: Exclusive enteral nutrition (EEN) is one of the first-line therapeutic options for pediatric patients with active Crohn’s disease (CD). However, only sparse data exist on plasma metabolic changes from patients on EEN therapy. Thus to gain mechanistic insights, we have characterized selected markers in pediatric CD patients treated with EEN for induction of disease remission. Methods: Plasma levels of 18 cytokines and chemokines and 163 metabolites in 10 pediatric CD patients receiving 8 weeks of EEN therapy were measured. Measurements were performed at three time points: a) at baseline (V0); b) during EEN intervention at week 4 (V4) and; c) at 4 weeks after completion of EEN therapy at week 12 (V12). Results: Comparisons between V0 and V4 levels identified changes in 20 different molecules, including increases in 7 metabolites of the diacyl phosphatidylcholine (PC) class and 6 metabolites of the alkylacyl PC class. However, most of these changes were not sustained after returning to a normal diet, i.e. only 7 out of the 20 molecules with significant changes between V0 and V4 still retained significance upon comparing V0 and V12. Conclusions: The changes in the plasma levels of various phospholipids at different time-points reflect the nutritional intervention and improved health status of pediatric CD patients.
Keywords
Inflammatory bowel disease; Nutrition; Lipidomics; Cytokines; Chemokines; Crohn’s diease
Abbreviations
CD: Crohn’s Disease; EEN: Exclusive Enteral Nutrition; PCDAI: Pediatric CD Activity Index; LPC: Lysophosphatidylcholines; PC: Phosphatidylcholine: PC-O: 1-Oalkyl- 2-acylglycerophosphocholines; SM: Sphingomyelins; SM-OH: Hydroxy-Sphingomyelin; IL: Interleukin; TH: T-Helper Cells; LOD: Limit of Detection; PCA: Principal Component Analysis; OPLS: Orthogonal Projection to Latent Structures; VIP: Variable Importance in Projection; RF: Random Forests; FDR: False Discovery Rate; CRP: C-Reactive Protein; His: Histidine; Trp: Tryptophan; MDC: Macrophage-Derived Chemokine; TARC: Thymus and Activation Regulated Chemokine; CCR4: CC Chemokine Receptor 4; LA: Linoleic Acid; DGLA: dihomo-γ-Linolenic Acid; EPA: Eicosapentaenoic Acid; DHA: Docosahexaenoic Acid; ALA: α-Linolenic Acid
Introduction
Crohn’s disease (CD) is one of the two main subtypes of inflammatory bowel diseases (IBD). The age of onset for CD has two peaks, one among which is in adolescence [1]. The pediatric CD population represents a particularly challenging group of IBD patients, as, in addition to an extended course of disease, growth failure and malnutrition are some of its major complications. Exclusive enteral nutrition (EEN) forms one of the mainstays of the different therapeutic approaches in this population has been recommended as the first choice of treatment with a high remission rate, particularly in newly diagnosed patients [2,3]. Apart from avoiding the metabolic consequences of systemic corticosteroids, the benefits of nutritional therapy include: a) improved mucosal healing; b) improved quality of life; c) improvement in nutritional status and; d) improvement in musculoskeletal growth parameters [4,5]. Despite an extensive body of literature supporting the use of nutritional therapy in pediatric CD, the underlying mechanisms for these benefits are not fully understood.
In this study, we undertook characterization of selected metabolites, including lipids and amino acids as well as selected chemokines and cytokines, before, during and after intervention with exclusive enteral nutrition (EEN) in pediatric CD patients. It was believed that the kinetic characterization of metabolic and inflammatory changes may provide insights into the beneficial mechanisms associated with EEN.
Material and Methods
Patient recruitment and the clinical trial protocol have been outlined in detail previously [5]. Briefly, pediatric patients (6-18 years of age) with active CD as diagnosed according to the ESPGHAN criteria were recruited consecutively after obtaining an appropriate informed consent. Exclusion criteria included extensive small bowel resection (>100 cm), ileostomy, extra-intestinal manifestations of CD and other systemic diseases. If the disease course worsened to warrant need of steroids or biologicals the patient was excluded from further follow-up in the study. The severity of the disease was assessed according to the pediatric CD activity index (PCDAI) [6]. A score of <10 is defined as being in remission, 10-27.5 as mild, 27.6-37.5 as moderate, and more than 37.5 as severe. EEN was started as treatment for all the patients included in the study. The formulation used was a casein-based polymeric formula (Modulen IBD®, Nestlé Frankfurt, Germany). The lipid composition of the formula is shown in Table 1A and 1B. The powdered formulation was reconstituted and given either orally or by nasogastric feeding as exclusive nutrition for 8 weeks. Only water and chewing gum were allowed in addition to the oral or enteral formula diet. The volume provided was determined by the attending physician according to the estimated energy requirements based on actual weight and target weight after 8 weeks in patients with underweight. All patients completed the EEN intervention for 8 weeks. Following EEN, gradual transition to regular diet done over a period of 2-4 weeks and by week 12 all patients were on regular diet. Plasma was analyzed from blood collected at three time points: initial visit (V0), at 4 weeks (V4) and finally at 12 weeks of the initial visit (V12).
| Total fat | 23 g /100 g product |
| Milk fat | 12.8 g/100 g product |
| Medium chain triglycerides | 6.0 g/100 g product |
| Corn oil | 3.2 g/100 g product |
| Soy lecithin | 1.0 g/100 g product |
Table 1A: Lipid composition of Modulen IBD® (provided by manufacturer).
| Fatty acid Composition of Modulen IBD | per 100 g product | per 100 g fat | per 100 g fatty acids | |
|---|---|---|---|---|
| Total Saturated | 14.61 | 63.6 | 67.8 | |
| Total Monounsaturated | 3.75 | 16.3 | 17.4 | |
| Total Polyunsaturated | 2.38 | 10.3 | 11 | |
| out of which | n-6 | 2.24 | 9.72 | 10.4 |
| n-3 | 0.14 | 0.61 | 0.7 | |
| linoleic | 2.23 | 9.71 | 10.4 | |
| alpha-linolenic | 0.13 | 0.56 | 0.6 | |
| Ratios | ||||
| linoleic/alpha-linolenic | 17.38 | |||
| Polyunsaturated/saturated | 0.16 | |||
| Fatty acids/Fat | 0.94 | |||
| n-6/n-3 | 15.9 | |||
| Butyric acid (C4:0) | 0.386 | 1.68 | 1.79 | |
| Caproic acid (C6:0) | 0.274 | 1.19 | 1.27 | |
| Caprylic acid (C8:0) | 3.336 | 14.51 | 15.47 | |
| Capric acid (C10:0) | 2.534 | 11.02 | 11.75 | |
| Lauric acid (C12:0) | 0.523 | 2.28 | 2.43 | |
| Myristic acid (C14:0) | 1.292 | 5.62 | 5.99 | |
| C15:0 acid | 0.133 | 0.58 | 0.62 | |
| Palmitic acid (C16:0) | 4.44 | 19.31 | 20.6 | |
| Margaric acid (C17:0) | 0.085 | 0.37 | 0.39 | |
| Stearic acid (C18:0) | 1.554 | 6.76 | 7.21 | |
| Arachidic acid (C20:0) | 0.033 | 0.14 | 0.15 | |
| Behenic acid (C22:0) | 0.013 | 0.06 | 0.06 | |
| Lignoceric acid (C24:0) | 0.012 | 0.05 | 0.06 | |
| Myristoleic acid (C14:1 n-5) | 0.085 | 0.37 | 0.39 | |
| Palmitoleic acid (C16:1) | 0.149 | 0.65 | 0.69 | |
| C17:1 acid | 0.036 | 0.16 | 0.17 | |
| Oleic acid (C18:1 n-9) | 3.478 | 15.13 | 16.14 | |
| Gondoic acid (C20:1 n-9) | 0.002 | 0.01 | 0.01 | |
| Linoleic acid (C18:2 n-6) | 2.233 | 9.71 | 10.36 | |
| Arachidonic acid (C20:4 n-6) | 0.002 | 0.01 | 0.01 | |
| Alpha linolenic acid (C18:3 n-3) | 0.129 | 0.56 | 0.6 | |
| C20:3 acid (n-3) | 0.012 | 0.05 | 0.06 | |
Table 1B: Fatty=composition of Modulen IBD® (provided by manufacturer).
Metabonomics analysis
A targeted mass spectrometric metabonomic approach using the Biocrates Life Sciences AbsoluteIDQTM kit was applied to plasma samples as previously published [7]. Sample preparation, extraction and loading was done according to the manufacturer’s instructions. A final volume of 10 μl of plasma was loaded onto the provided 96-well plate, containing isotopically labeled internal standards. Analyses were done on a Dionex Ultimate 3000 liquid chromatography system (Dionex AG, Olten, Switzerland) coupled to a 3200 QTRAP mass spectrometer (AB Sciex, Foster City, CA, USA) fitted with a TurboV ion source operating the electrospray ionization (ESI) mode. Sample extracts were analyzed in both positive and negative ESI modes via direct infusion using a gradient flow rate of 0-2.4 min: 30 μl/min, 2.4-2.8 min: 200 μl/min, 2.9-3 min: 30 μl/min. Mass spectrometer was operated with the desolvation temperature of 200°C, ESI voltage at -4500 V (ESI -) and 5500 V (ESI +). Tandem mass spectrometry in the selected reaction monitoring mode was performed with nitrogen collision gas pressure of 5 mTorr and optimised declustering potential values for the 163 metabolites screened in the assay. Raw data files (Analyst software, version 1.5.1; AB Sciex, Foster City, CA, USA) were imported into the provided analysis software MetIQ to calculate metabolite concentrations. Individual lipid species are annotated as follows: [lipid class] [total number of carbon atoms]:[total number of double bonds]. For example, PC 34:4 reflects a phosphatidylcholine species comprising 34 carbon atoms and 4 double bonds. Lipid classes were labelled as follows: LPC, Lysophosphatidylcholines; PC, Phosphatidylcholines; PC-O, 1-O-alkyl-2-acylglycerophosphocholines; SM, Sphingomyelins; and SM-OH, Hydroxy-Sphingomyelin.
Cytokine and chemokine analysis
Cytokine and chemokine analysis were performed using the human T-helper cells (TH) type 1 (TH1) and type 2 (TH2) 10-plex and the human chemokine 9-plex ultrasensitive kits from mesoscale discovery as per the manufacturer’s instructions (Meso scale Discovery, Maryland, USA). The concentrations for interleukin (IL)-1β and IL-13 were below the limit of detection and hence were not used for data analysis. IL-8 was represented in both kits and considering the high amount of inter-assay variability that has been observed for these kits [8], the concentration values of IL-8 from the TH1/TH2 10-plex ultrasensitive kit were used. The limit of detection (LOD) for individual cytokines and chemokines is provided in supplementary Table 1A.
Statistical analysis
Quantitative data were pre-processed prior to the analysis. To remove non determined values, the LOD of such a variable was used instead. To further reduce the list of relevant species, data was analyzed first using the package SIMCA-P+ (version 12.0, Umetrics AB, Umeå, Sweden) and in-house developed MATLAB (The MathWorks Inc., Natick, MA, USA) routines. In order to detect the presence of similarities between metabolic profiles, Principal Component Analysis (PCA) and the Orthogonal Projection to Latent Structures (OPLS) were used [9].
Internal validation (cross-validation, 7 segments, random sampling) was used to assess the validity of the model. The classification accuracy of the OPLS-DA model was established from the predicted samples at each cross-validation cycle. Results of this model allowed a sub selection of variables ranked according to their Variable Importance in Projection (VIP) values [10].
Significant changes in cytokines, chemokines and selected metabolomic data between different time points were analyzed by Random Forests (RF). The ‘randomForest’ package [11] in the R environment (R Core Team, 2012) was used for this purpose, with 500 trees and 4 variables at each split as model parameters. In-house written routines in R were used for pre-processing and hypothesis testing.
To keep a balanced set for the analysis, samples corresponding to individuals not present at all three time-points were removed. The uncorrected and the false discovery rate (fdr) corrected p-values for data passing the initial pre-processing filters is provided in supplementary Table 2.
| Variable | Value |
|---|---|
| Male patients [n/N] | 7/10 |
| Age, median (range) [yrs] | 13.7 (10.6; 17.7) |
| Bone age, median (range) [yrs] | 13.5 (8.5-18.0) |
| Body mass index median (range) [z-score compared to reference] | -1.25 (-2.02; 0.18) |
| Disease localisation [n] | |
| - ileocolonic/colonic | 9/1 |
| - upper GI involved | 6 |
| - perianal fistula | 0 |
| PCDAI remission / mild / moderate / severe activity [n] | 0 / 3 / 5 / 2 |
| CRP, median (range) | 2.5 (0.3-5.0) |
| >0.5mg/dl [n/N] | 9/10 |
Table 2: Baseline characteristics of patients.
Non-parametric Spearman rho values for correlations and their two-tailed p values were calculated using GraphPad Prism 5 software (San Diego, California, USA). The correlations were calculated for data from each visit between either PCDAI or C-reactive protein (CRP) and the metabolites that show a significant change between any of the two visits.
Ethical considerations
The clinical trial protocol was approved by the Federal Office for Radiation Protection (Salzgitter, Germany, approval Z5-22462/2-2004-051) and the Ethical Committee of the Medical Faculty of the University of Munich (project 202/04). Informed consent was obtained from both parents/caregivers and the patients.
Results
This study is a retrospective analysis of pediatric CD patients which were recruited in a prospective study described earlier to investigate the effect of EEN on bone health, particularly on bone density and geometry [5]. The baseline characteristics of the patients characterized in this study are presented in Table 2.
Seven out of the 10 patients were newly diagnosed. All 10 patients received standard of care treatment, which includes 6-8 weeks of EEN.
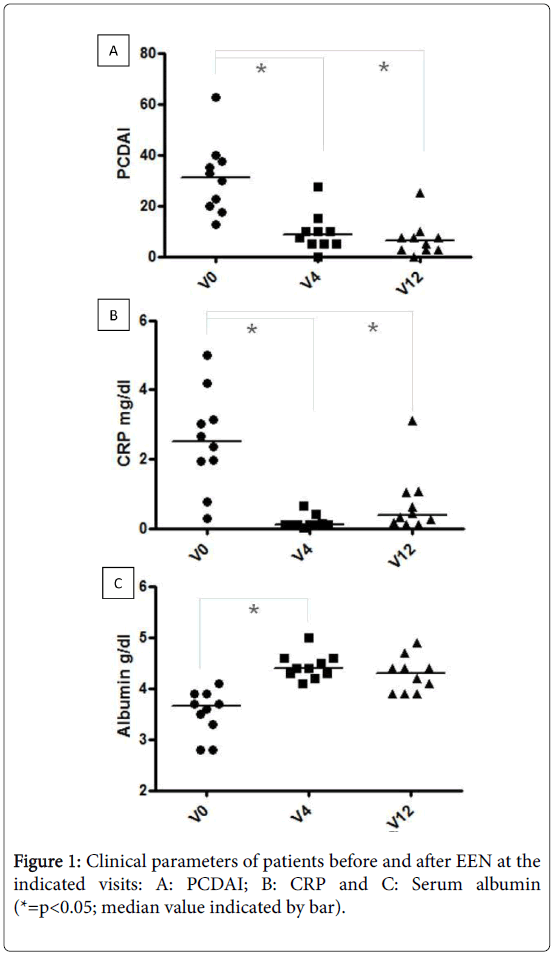
The progression of the disease on clinical parameters, following treatment, is depicted in Figure 1. The median PCDAI was significantly reduced from 31.3 to 8.8 and 6.3 at week 4 and week 12, respectively. This corresponds to a 50% and 80% remission rate at week 4 and week 12 respectively (Figure 1A).
In addition to the reduction in disease activity, median CRP levels were also significantly reduced from 2.5 mg/dl to 0.1 mg/dl and 0.38 mg/dl at week 4 and week 12, respectively (Figure 1B). The simultaneous improvement in nutritional status is highlighted by improved levels of serum albumin from median baseline levels of 3.6 g/dl to 4.4 g/dl at week 4 (Figure 1C).
The plasma of these patients was characterized for the levels of 163 metabolites, 8 cytokines and 8 chemokines at the three different time points.
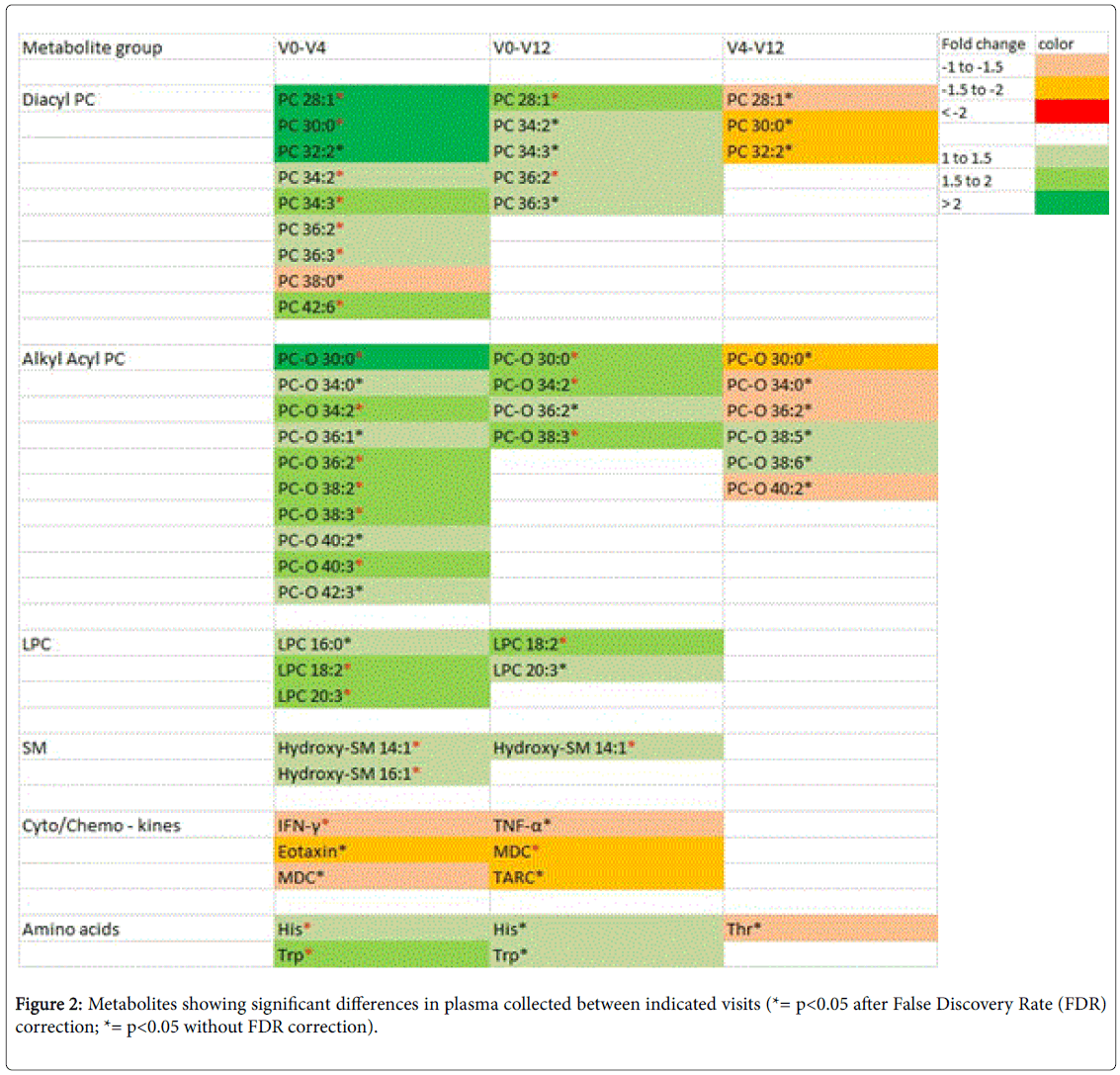
The median values of these compounds are presented in supplementary Table 1. Significant changes over time in a variety of metabolites as well as limited changes in cytokine and chemokine levels are observed (Figure 2).
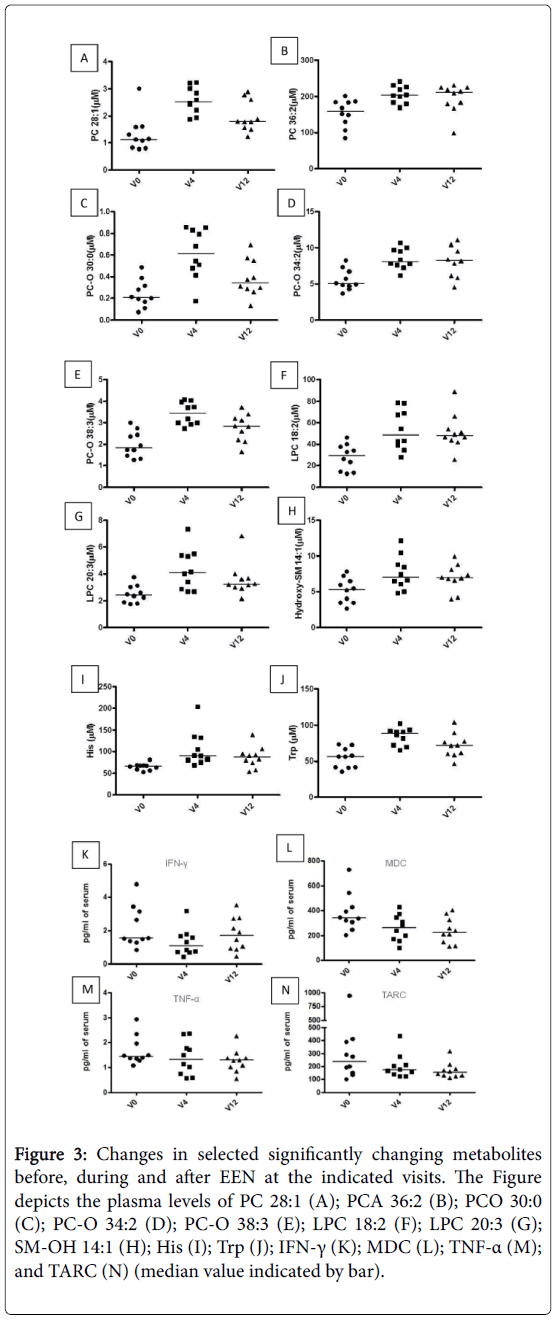
Among the diacyl PC metabolites changing between baseline and week 4 and those that remained significant after an fdr correction, the biggest change was observed in the plasma concentration of PC 28:1. As further detailed in Figure 3A, the median baseline values for PC 28:1 was 1.1 μM and these values increased to 2.5 μM at week 4. By week 12 the concentration of PC 28:1 was 1.8 μM.
Although the concentration of PC 28:1 was still significantly higher as compared to baseline, there was a trend towards its reduction when compared to week 4. Apart from PC 28:1 which is normally present at low concentrations in human plasma, another diacyl PC that increased in concentration at both week 4 and week 12 is PC 36:2 (Figure 2 and Figure 3B).
The median baseline concentration for PC 36:2 was 160 μM, which increased by more than 25% at week 4 and remained significantly higher at the end of week 12, when its median concentration was 211.5 μM.
Ten ether linked PC metabolites were identified to be changing at week 4 as compared to baseline. However, out of these only 6 metabolites retained their significance after a false discovery rate correction (Figure 2).
Further among these 6 metabolites, 3 metabolites were still significantly different from baseline at week 12. These metabolites were PC-O 30:0, PC-O 34:2 and PC-O 38:3. The concentrations of these metabolites at the three different time points are depicted in Figure 3C-3E. The maximal median concentrations for PC-O 30:0 and PC-O 38:3 were observed at week 4 at 0.6 μM and 3.99 μM, respectively, whereas the maximal median concentration for PC-O 34:2 was observed at week 12 at 8.26 μM.
In line with the changes in the PC metabolites, wherein most of the changes are seen in unsaturated species, the unsaturated LPC metabolites, LPC 18:2 and LPC 20:3, are significantly increased at week 4 over baseline (Figure 2, Figure 3F and Figure 3G), while only the linoleic acid containing LPC still retains significance after fdr correction at week 12 compared to baseline (Figure 2 and Figure 3F). Hydroxy-SM 14:1 and Hydroxy-SM 16:1, are significantly increased by more than 50% and 25%, respectively over baseline at week 4 and Hydroxy-SM 14:1 (supplementary Table 1) maintains this increase over baseline even at week 12.
Apart from the phosphocholine containing metabolites, only the concentrations of His and Trp significantly increased from median baseline values of 66.9 and 55.9 μM to 90.1 and 88.4 μM at week 4, respectively (Figure 3). None of the other metabolites, including acyl carnitines, showed any significant changes in their concentration.
Figure 3: Changes in selected significantly changing metabolites before, during and after EEN at the indicated visits. The Figure depicts the plasma levels of PC 28:1 (A); PCA 36:2 (B); PCO 30:0 (C); PC-O 34:2 (D); PC-O 38:3 (E); LPC 18:2 (F); LPC 20:3 (G); SM-OH 14:1 (H); His (I); Trp (J); IFN-γ (K); MDC (L); TNF-α (M); and TARC (N) (median value indicated by bar).
Among the different cytokines and chemokines that were measured in this group of patients, the comparison of baseline to week 4 reveals that interferon (IFN)-γ is significantly reduced while Eotaxin and macrophage-derived chemokine (MDC) show trends towards a reduction.
Similarly upon comparing values at baseline with those at week 12 reveals a significant reduction in MDC, but only trends towards reduction for tumor necrosis factor (TNF)-α and thymus and activation regulated chemokine (TARC). The median values for IFN-γ reduced by more than 40% at week 4 and those for MDC were reduced by more than 35% at week 12.
In an additional bid to identify key metabolites and cytokines that are linked with the different stages of nutritionally-mediated disease recovery, we performed Spearman correlational analysis on the significantly changing variables with clinically relevant parameters such as PCDAI and CRP. The metabolites that are significantly correlated with either PCDAI or CRP are tabulated in Table 3 and Table 4, respectively.
| PCDAI | ||||||||
| V0 | V4 | V12 | ||||||
| metabolite | r | p | metabolite | r | p | metabolite | r | p |
| PC 38:0 | 0.7576 | 0.0149 | IFN-g | -0.6648 | 0.036 | |||
| PC-O 30:0 | -0.6485 | 0.049 | PC-O 38:2 | -0.6399 | 0.0463 | |||
| PC-O C38:3 | -0.6727 | 0.039 | ||||||
| LPC 20:3 | -0.6848 | 0.0347 | ||||||
Table 3: Metabolites showing significant correlation with PCDAI at indicated visits.
| V0 | V4 | V12 | ||||||
|---|---|---|---|---|---|---|---|---|
| metabolite | r | p | metabolite | r | p | metabolite | r | p |
| Eotaxin | -0.8061 | 0.0072 | Trp | -0.7645 | 0.0126 | Trp | -0.6626 | 0.0438 |
| PC 32:2 | -0.6727 | 0.039 | PC 28:1 | -0.6444 | 0.049 | |||
| PC 34:2 | -0.8061 | 0.0072 | PC 34:2 | -0.6565 | 0.0438 | |||
| PC 34:3 | -0.6848 | 0.0347 | PC 34:3 | -0.6687 | 0.039 | |||
| PC 36:2 | -0.6727 | 0.039 | PC√?¬† 36:3 | -0.6809 | 0.0347 | |||
| PC-O 34:2 | -0.697 | 0.0306 | PC-O 36:2 | -0.7477 | 0.0174 | |||
| PC-O 36:1 | -0.6848 | 0.0347 | PC-O 38:3 | -0.693 | 0.0306 | |||
| PC-O 36:2 | -0.7939 | 0.0088 | ||||||
| LPC 16:0 | -0.7697 | 0.0126 | ||||||
| LPC 18:2 | -0.8788 | 0.0016 | ||||||
Table 4: Metabolites showing significant correlation with CRP at indicated visits.
Overall, it is apparent that there is no overlap between the metabolites that correlate with PCDAI and CRP. Numerically, there are more metabolites that correlate at the initial stage as compared to the post-interventional stages.
For PCDAI, no overlapping metabolites were identified among the different time-points. For CRP, while no overlapping metabolites were identified among all three time-points, PC 34:2, PC 34:3 and PC-O 36:2 negatively correlated at time-points V0 and V12. Additionally, Trp levels were negatively correlating with CRP at time-points V4 and V12.
Discussion
The objective of the study was to characterize targeted parameters in 10 prospectively recruited pediatric CD patients treated with EEN to achieve remission of the disease. Established mass spectrometry- and immunoassay- based methodologies were utilized to achieve this. The pediatric CD cohort used in this study is clinically well characterized [5]. It is hoped that this approach will provide insights into the metabolic consequences and unlock underlying mechanisms of the benefits of enteral nutritional therapy.
The efficacy of EEN in the pediatric CD population is well established [2,4,12]. In this study the standard of care, which consists of EEN as the sole source of nutrition for up to 8 weeks, was provided. At the initial visit, high PCDAI and CRP values provide evidence of active disease. The efficacy of the therapeutic intervention is confirmed by a significant reduction in both the PCDAI and CRP values within 4 weeks of intervention and this benefit is maintained at the later timepoint. In the current study we observed that 80% of the patients were in clinical remission at week 12. This corroborates previous findings observed with this type of intervention [2,13,14].
Having confirmed the efficacy of EEN in this cohort, we analyzed the plasma for selected cytokines, chemokines and metabolites, as mentioned earlier. It is reasonable to expect unique cytokine and chemokine profiles in CD patients depending on the clinical stage, intestinal involvement and the type of therapy [15-17]. However, to our best knowledge the characterization of plasma cytokine and chemokine profiles after EEN has not been previously undertaken. Among the 18 molecules assessed, we found a decrease in 2 proinflammatory cytokine concentrations, namely, IFN-γ and TNF-α, with decreasing severity of the disease. This is in line with earlier studies wherein pediatric patients under EEN therapy with the same diet showed a significant reduction in mucosal IFN-γ mRNA expression [14]. Broadly, building from previously established relationships between cytokine levels with mucosal expression and disease activity, this may reflect a systemic or mucosal reduction in TH1 cell number or activity [14,18]. Additionally, with regards to the chemokines we found that EEN reduced levels of MDC and TARC. These TH2 attracting and activating chemokines are expressed mainly by innate cell and target CC chemokine receptor 4 (CCR4) which in turn is expressed largely by TH2 cells [19,20]. It should be noted that increased levels of MDC have previously been reported in adult CD patients, levels of which did not decrease during treatment with systemic steroids [21]. It is known that TNF-α stimulation of innate cells enhances MDC production [22]. Therefore, it is likely that a parallel reduction of TNF-α might explain the reduced chemokine levels observed in EEN-treated patients.
Among the metabolites measured, nutritionally-mediated disease recovery is reflected in several PC species. Previous studies have characterized either the plasma fatty acid (FA) profile or the profile of FA linked with PC species in the plasma of active and quiescent CD patients and their matched healthy controls [23-25]. However, the kinetic study of changes in plasma PC species mediated during disease recovery in pediatric CD patients has not been done. In the present study, at the initial time-point, multiple diacyl PC species and alkyl ether PC species negatively correlate with PCDAI and CRP. Levy et al. have previously observed a reduction in plasma levels of polyunsaturated fatty acids (PUFA) during active pediatric CD [23]. Thus it is interesting that in our cohort, among the several PC species that show a negative correlation with PCDAI and CRP, the unsaturated PC species predominate. Additionally, Trebble et al. have observed a reduction in plasma PC-linked linoleic acid (LA) in active disease as compared to age matched healthy controls. In support of reduced LA levels, we find that LPC 18:2, which is expected to have LA as the linked fatty acid, is negatively correlated with CRP [25]. Further, PC 32:2, PC 34:2 and PC 36:2, which may also contain LA are also negatively correlated with CRP. Despite the lack of an age-matched control cohort in our study, we believe that metabolites that negatively correlate with the increasing values of PCDAI and CRP reflect reduced levels compared to a healthy state indicating that inflammation increases lipid breakdown [26-28]. In support of this, reduction in fat mass and lipoprotein-associated phospholipids has been observed during active CD [23,24,29]. In addition to inflammation, reduced dietary intake [4,30], may further contribute to this situation. Hence, taken together, there is a high likelihood that levels of PC are lower during active CD. It is also interesting to note that during EEN, all of the previously observed relationships with CRP are lost, but some of those reappear when the patient reverts to a normal diet.
Following the initial intervention with EEN, there is an increase in the levels of 19, out of the 76, diacyl and alkyl ether containing PC species that were measured. As mentioned earlier, the inflammatory catabolic state during active disease is ameliorated by EEN, thus restoring the lipid anabolic state. The formula used in this study is known to contain approximately 6% of the total fatty acids as myristic acid (Table 1). This is reflected in the increased levels of PC 28:1, PC 30:0 and PC 32:2 at 4 weeks after initiation of EEN. Further, the formula provides the required daily intake of essential fatty acids (Table 1). The adequate intake of LA is evidenced in the increased levels of PC 36:2, PC 34:2, PC 32:2, PC 36:3, PC 38:3, PC 40:3, LPC 18:2 and LPC 20:3 which are likely to contain LA and dihomo-γ- linolenic acid (DGLA). At 12 weeks, the patients have transitioned to a normal diet. It appears that the PC levels start to reduce with resuming a normal diet. Less than 50% of the PC species, with increased levels at the 4 week time point, have higher levels compared to the initial time point. Among these, PC 28:1 and PC-0-30:0, which are likely to contain medium chain fatty acids (MCFA), are maintained at higher levels despite a trend towards reduction between week 4 and 12. This reduction of PC species containing MCFA is expected during the transition away from enteral nutrition, which contains medium chain triglycerides. The trend in increased levels of PC-O 38:5 and PC-O 38:6 between weeks 4 and 12 seems to reflect endogenous synthesis of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) from the increased supply of α-linolenic acid (ALA). The lag-phase of increase could be explained by the slow rate of ALA-conversion. However, both the lack of maintenance of PC 42:6 levels at week 12 and the reappearance of the negative correlations of PC 34:2, PC 34:3 and PC-O 36:2 with mildly increasing CRP levels, perhaps, warrant caution.
In summary, the nutritional switch from a mixed diet to EEN and the associated improvement in nutritional status and reduction of disease activity in pediatric CD patients is reflected in plasma metabolic and immunological parameters. While a cautious interpretation to the data presented herein is warranted, the study suggests that follow-up of patients with regular intervals of monitoring may be beneficial in early identification of nutritional needs and metabolic changes.
Financial Support
S.K. was supported by a research grant from Nestec SA. The work of B.K was partly supported by European Research Council Advanced Grant ERC-2012-AdG-no.322605 META-GROWTH. V.B., I.M, N.B., F-P.M., P.G, M.O., E.S. and J.B. are employed by Nestec SA.
References
- Palfai TP, Monti PM, Ostafin B, Hutchison K (2000) Effects of nicotine deprivation on alcohol-related information processing and drinking behavior. J Abnorm Psychol 109: 96-105.
- Harrison EL, Hinson RE, McKee SA (2009) Experimenting and daily smokers: episodic patterns of alcohol and cigarette use. Addict Behav 34: 484-486.
- Howell A, Leyro T, Hogan J, Buckner J, Zvolensky M (2010) Anxiety sensitivity, distress tolerance, and discomfort intolerance in relation to coping and conformity motives for alcohol use and alcohol use problems among young adult drinkers. Addictive Behaviors 35:1144-1147.
- Krukowski RA, Solomon LJ, Naud S (2005) Triggers of heavier and lighter cigarette smoking in college students. J Behav Med 28: 335-345.
- Reed MB, Wang R, Shillington AM, Clapp JD, Lange JE (2007) The relationship between alcohol use and cigarette smoking in a sample of undergraduate college students. Addictive Behaviors 32: 449-464.
- Hughes JR, Kalman D (2006) Do smokers with alcohol problems has more difficulty quitting? Drug Alcohol Depend 82: 91-102.
- Hurt RD, Offord KP, Croghan IT, Gomez-Dahl L, Kottke TE, et al. (1996) Mortality following inpatient addictions treatment: Role of tobacco use in a community-based cohort. JAMA: Journal of the American Medical Association 275: 1097-1103.
- Lisha NE, Carmody TP2, Humfleet GL2, Delucchi KL2 (2014) Reciprocal effects of alcohol and nicotine in smoking cessation treatment studies. Addict Behav 39: 637-643.
- Taylor B, Rehm J (2006) When risk factors combine: The interaction between alcohol and smoking for aerodigestive cancer, coronary heart disease, and traffic and fire injury. Addictive Behaviors 31: 1522-1535.
- Jarvis CM, Hayman LL, Braun LT, Schwertz DW, Ferrans CE, et al. (2007) Cardiovascular risk factors and metabolic syndrome in alcohol- and nicotine-dependent men and women. J CardiovascNurs 22: 429-435.
- Joseph AM, Willenbring ML, Nugent SM, Nelson DB (2004) A randomized trial of concurrent versus delayed smoking intervention for patients in alcohol dependence treatment. Journal of Studies on Alcohol, 65: 681-691.
- Kodl M, Fu SS, Joseph AM (2006) Tobacco cessation treatment for alcohol-dependent smokers: when is the best time? Alcohol Res Health 29: 203-207.
- Fu S, Kodl M, Willenbring M, Nelson D, Nugent S, et al. (2008) Ethnic differences in alcohol treatment outcomes and the effect of concurrent smoking cessation treatment. Drug and Alcohol Dependence 92: 61-68.
- Holt LJ, Litt MD, Cooney NL (2012) Prospective analysis of early lapse to drinking and smoking among individuals in concurrent alcohol and tobacco treatment. Psychology of Addictive Behaviors 26:561-572.
- Centers for Disease Control and Prevention (CDC) (2009) Cigarette smoking among adults and trends in smoking cessation - United States, 2008. MMWR Morb Mortal Wkly Rep 58: 1227-1232.
- Irving LM, Seidner AL, Burling TA, Thomas RG, Brenner GF (1994) Drug and alcohol abuse inpatients' attitudes about smoking cessation. J Subst Abuse 6: 267-278.
- Macnee CL, Talsma A (1995) Development and testing of the barriers to cessation scale. Nurs Res 44: 214-219.
- Orleans CT, Rimer BK, Cristinzio S, Keintz MK, Fleisher L (1991) A national survey of older smokers: treatment needs of a growing population. Health Psychol 10: 343-351.
- Kristeller JL (1994) Treatment of hard-core, high-risk smokers using FDA approved pharmaceutical agents: An oral health team perspective. Health Values 18: 25-32.
- Asher MK, Martin RA, Rohsenow DJ, MacKinnon S, Traficante R, et al. (2003) Perceived barriers to quitting smoking among alcohol dependent patients in treatment. Journal of Substance Abuse Treatment 24: 169-174.
- Martin RA, Rohsenow DJ, MacKinnon SV, Abrams DB, Monti PM (2006) Correlates of motivation to quit smoking among alcohol dependent patients in residential treatment. Drug Alcohol Depend 83: 73-78.
- Marlatt GA, Gordon JR (1985) Relapse prevention. New York: Guilford Press.
- Velicer WF, DiClemente CC, Prochaska JO, Brandenburg N (1985) Decisional balance measure for assessing and predicting smoking status. J PersSoc Psychol 48: 1279-1289.
- DiClemente CC, Prochaska JO (1982) Self-change and therapy change of smoking behavior: a comparison of processes of change in cessation and maintenance. Addict Behav 7: 133-142.
- Curry SJ, Grothaus L, McBride C (1997) Reasons for quitting: intrinsic and extrinsic motivation for smoking cessation in a population-based sample of smokers. Addict Behav 22: 727-739.
- Baha M, Le Faou AL (2010) Smokers' reasons for quitting in an anti-smoking social context. Public Health 124: 225-231.
- Curry SJ, McBride C, Grothaus LC, Louie D, Wagner EH (1995) A randomized trial of self-help materials, personalized feedback, and telephone counseling with nonvolunteer smokers. J Consult Clin Psychol 63: 1005-1014.
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M (1993) Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction 88: 791-804.
- First MB, Williams JB, Spitzer RL, Gibbon M (2002) Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Clinical Trials Version (SCID-CT). New York: Biometrics Research, New York State Psychiatric Institute.
- Brown RA, Lejuez CW, Kahler CW, Strong DR (2002) Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol 111: 180-185.
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO (1991) The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict 86: 1119-1127.
- Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF (1994) Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addict Behav 19: 33-39.
- Fagerstrom KO, Heatherton TF, Kozlowski LT (1990) Nicotine addiction and its assessment. Ear Nose Throat J 69: 763-765.
- Filbey FM, Claus E, Audette AR, Niculescu M, Banich MT, et al. (2007) Exposure to the taste of alcohol elicits activation of the mesocorticolimbicneurocircuitry. Neuropsychopharmacology 33: 1391-1401.
- Fleming MF, Barry KL, MacDonald R (1991) The alcohol use disorders identification test (AUDIT) in a college sample. Int J Addict 26: 1173-1185.
- Cherpitel CJ (1995) Analysis of cut points for screening instruments for alcohol problems in the emergency room. J Stud Alcohol 56: 695-700.
- Macnee CL, Talsma A (1995) Predictors of progress in smoking cessation. Public Health Nurs 12: 242-248.
- Curry S, Wagner EH, Grothaus LC (1990) Intrinsic and extrinsic motivation for smoking cessation. J Consult Clin Psychol 58: 310-316.
- McBride CM, Pollak KI, Bepler G, Lyna P, Lipkus IM, et al. (2001) Reasons for quitting smoking among low-income African American smokers. Health Psychol 20: 334-340.
- Bonn-Miller MO, Zvolensky MJ (2009) An evaluation of the nature of marijuana use and its motives among young adult active users. Am J Addict 18: 409-416.
- Buckner JD, Zvolensky MJ, Schmidt NB (2012) Cannabis-related impairment and social anxiety: the roles of gender and cannabis use motives. Addict Behav 37: 1294-1297.
- Agrawal A, Budney AJ, Lynskey MT (2012) The co-occurring use and misuse of cannabis and tobacco: a review. Addiction 107: 1221-1233.
- Degenhardt L, Hall W, Lynskey M (2001) The relationship between cannabis use and other substance use in the general population. Drug Alcohol Depend 64: 319-327.
- Cohen J, Cohen P (1983) Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum.
- Cohen J, Cohen P, West SG, Aiken LS (2003) Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Mahwah, NJ US: Lawrence Erlbaum Associates Publishers.
- Lipkus IM, Feaganes JR, Green JD, Sedikides C (2001) The Relationship Between Attitudinal Ambivalence and Desire to Quit Smoking Among College Smokers. Journal of Applied Social Psychology, 31: 113-133.
- Wilson SJ, Creswell KG, Sayette MA, Fiez JA (2013) Ambivalence about smoking and cue-elicited neural activity in quitting-motivated smokers faced with an opportunity to smoke. Addict Behav 38: 1541-1549.
- Festinger LA (1957) A theory of cognitive dissonance. Evanston, IL: Row, Peterson.
- Markowitz LJ (2000) Smoker's perceived self-exemption from health risks. Psi Chi Journal of Undergraduate Research 5: 119-124.
- Jamieson P, Romer D (2001)What do young people think they know about the risks of smoking? In P. Slovic (Ed.), Smoking: Risk, perception, and policy (pp. 51-63). Thousand Oaks, CA US: Sage Publications, Inc.
- Schane RE, Glantz SA, Ling PM (2009) Social smoking implications for public health, clinical practice, and intervention research. American Journal of Preventive Medicine 37: 124-131.
- DaniJA, De Biasi M (2001) Cellular mechanisms of nicotine addiction. PharmacolBiochemBehav 70: 439-446.
- Nestler EJ (2005) Is there a common molecular pathway for addiction? Nat Neurosci 8: 1445-1449.
- Ehrman RN, Robbins SJ, Bromwell MA, Lankford ME, Monterosso JR, et al. (2002) Comparing attentional bias to smoking cues in current smokers, former smokers, and non-smokers using a dot-probe task. Drug Alcohol Depend 67: 185-191.
- Kerst WF, Waters AJ (2014)Attentional retraining administered in the field reduces smokers’ attentional bias and craving.
- Wiers RW, Rinck M, Kordts R, Houben K, Strack F (2010) Retraining automatic action-tendencies to approach alcohol in hazardous drinkers. Addiction 105: 279-287.
- Raupach T, West R, Brown J (2013) The most "successful" method for failing to quit smoking is unassisted cessation. Nicotine Tob Res 15: 748-749.
- Korte KJ, Capron DW, Zvolensky M, Schmidt NB (2013) The Fagerström test for nicotine dependence: do revisions in the item scoring enhance the psychometric properties? Addict Behav 38: 1757-1763.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 11288
- [From(publication date):
August-2016 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 10425
- PDF downloads : 863