Change in Public Knowledge, Attitude and Practice on Antibiotic use After a Territory-Wide Health Promotion Campaign in Hong Kong
Received: 08-Aug-2024 / Manuscript No. JIDT-24-144856 / Editor assigned: 12-Aug-2024 / PreQC No. JIDT-24-144856 (PQ) / Reviewed: 26-Aug-2024 / QC No. JIDT-24-144856 (QC) / Revised: 02-Sep-2024 / Manuscript No. JIDT-24-144856 (R) / Published Date: 09-Sep-2024 DOI: 10.4172/2332-0877.1000604
Abstract
Background: We evaluated the knowledge, attitude and practice on Antimicrobial Resistance (AMR) among the public, before and after a territory-wide campaign conducted in Hong Kong.
Methods: We conducted telephone surveys with target population of all Hong Kong residents aged ≥ 15 before and after the publicity campaign in November 2023. We adopted a standardized questionnaire and questions on knowledge, attitude and practices, e.g. whether some common conditions require antibiotics, awareness and common myths about AMR, infection control practices while taking antibiotics. Chi-square test was used to test for any significant difference between the results of 2022 and 2023 surveys.
Results: In the 2023 survey, 1083 residents were interviewed, with response rate of 50.1%. There was major improvement in knowledge that cold and flu need no antibiotics (from 49.7% to 83.3%, p<0.001) after the campaign. A large proportion (62.8% to 89.6%) did follow the infection control practice such as hand hygiene, disinfect and cover all wounds while taking antibiotics, with an improvement in wearing mask (72.3% in 2022 to 77.3% in 2023, p<0.001). Elderly respondents had lower health literacy on AMR, e.g. heard of antibiotic resistant, and resistant bacteria could be spread from person-to-person. Those who knew that antibiotics were not needed for flu were less likely to ask for antibiotics during consultation (2.7% vs. 11.4%, p<0.01).
Conclusion: Publicity campaign on AMR could improve public knowledge and behaviour on appropriate use of antibiotics. Targeted messages should be further promulgated to address knowledge deficit and the needs of the elderly to combat AMR.
Keywords: Antimicrobial resistance; Antimicrobial utilization; Antibiotics; Health promotion; Awareness campaign
Introduction
Health promotion campaign on appropriate use of antibiotics plays a vital role in AMR control. It has been noticed that a person’s knowledge, attitudes and beliefs about antimicrobials drives their use. This can be seen in their consultation behaviour by requesting antimicrobials from their general practitioners or by self-medication [1]. Studies have shown that mass media campaigns have increased public knowledge, changed their perception and behaviour in antibiotics use [2-6]. For example, after implementing a publicity campaign on the use of antibiotics and antibiotic resistance in Hong Kong in 2011, there was a significant increase in the proportion of respondents knowing that antibiotics could not cure influenza or viral infections. The study has shown that over one-quarter of the respondents could recall the campaign, mostly through announcement of public interest on television or radio. Besides, a systematic review has shown public health interventions using social media have positive outcomes in increasing AMR awareness [7].
At the Sixty-eighth World Health Assembly in May 2015, the World Health Organisation (WHO) endorsed a global action plan to tackle the growing problem of AMR. Among other initiatives, one of the objectives of the plan was to improve awareness and understanding of AMR through effective communication, education and training. The World AMR Awareness Week (WAAW) is a global campaign that is celebrated annually to improve awareness and understanding of AMR and encourage best practices among the public, One Health stakeholders and policymakers. In Hong Kong, we have launched the 2nd Strategy and Action Plan on AMR in November 2022 [8]. One of the key strategies is to increase public awareness and education on appropriate use of antibiotics. To echo the WAAW, we launched a publicity campaign in November 2023 to correct common myths and advocate for appropriate use of antibiotics. Health promotion activities included conducting press conference and media interviews, issuing press release, broadcasting television and radio advertisement, publicity through social media, public transport buses and mass transit railway, distribution of posters, pamphlets and promulgating videos at public hospitals and outpatient clinics. Key messages included common cold and flu need no antibiotics and infection control practices required while taking antibiotics. Health advice was printed in the medicine bags holding the antibiotics to remind patients taking appropriate actions to prevent transmission of resistant bacteria, e.g. wearing of mask, frequent hand hygiene, covering wound, minimizing contact with others while having respiratory symptoms. We conducted telephone survey among the general public before and after the campaign, and evaluated the effectiveness in changing public knowledge, attitude and practice on antibiotics use.
Materials and Methods
Survey design and sampling method
We conducted two rounds of telephone surveys with target population of all Hong Kong residents aged 15 or above who could speak Cantonese, Putonghua or English before and after the publicity campaign in 2023. Persons who stayed in institution and foreign domestic helper were excluded. Telephone numbers were randomly selected from the combined landline and mobile phone sampling frame obtained from the Office of the Communications Authority of Hong Kong. For the successfully contacted residential unit, the person aged 15 or above who was available and his or her birthday came soonest would be interviewed. For mobile phone number, the primary user of that particular number would be invited. When there was no response to the call, further attempts were made at different times of the day and on different days of the week, in order to minimize non-response bias. The response rate was defined as the number of completed cases, divided by the sum of the completed cases, refusal cases and drop-out cases. Weighting of the data was first done to compute the design weights by calculating the probability of being sampled in the combined landline frame and mobile phone frame, followed by adjusting the samples to the updated population’s age-gender distribution provided by the Census and Statistics Department [9,10].
Questionnaire design
A standardized bilingual (Chinese and English) questionnaire was designed, taking reference from similar surveys from WHO and other areas. To ensure comparability, most questions in the survey conducted in 2022 were kept with slight modifications to make the questions clearer in 2023. All questions were reviewed by public health physicians responsible for controlling AMR in human and food sector with a total of 18 questions included in the final survey tool. Questions included knowledge, attitude and practices such as whether or not some common conditions required antibiotics, awareness and common misconceptions of AMR and infection control practice while taking antibiotics. Relevant questions on food were also included as part of “One Health” approach to control AMR. A pilot study recruiting 15 interviewees from landline and 15 interviewees from mobile phone was conducted in October 2023. The questionnaire was then fine-tuned before conducting the field work from November 2023 to January 2024.
Statistical analysis
Frequency and percentage were used to present descriptive statistics. We conducted subgroup analysis in different age groups to assess for any difference in knowledge, attitude and practice. To compare the questions before (2022 survey) and after (2023 survey) the publicity campaign, chi-square test was used to test for any significant different in answering the questions by the respondents. The data were analysed using the statistical software package SPSS version 27 and p-value less than 0.05 would be considered as statistically significance.
Results
Comparison of the findings between 2022 and 2023 survey
In the 2023 survey, a total of 1,083 eligible Hong Kong residents aged 15 or above were successfully interviewed. The respondents included 426 landline users (39.3%) and 657 mobile phone users (60.7%), with combined response rate of 50.1%. Table 1 shows the basic demographics of the respondents and there was no significant difference in age and sex distributions between the two surveys. Tables 2-5 compare the results of the 2022 and 2023 surveys. On awareness, there was 66.7% and 22.6% of respondents in 2023 having heard of antibiotic resistance and antimicrobial resistance respectively, less than the corresponding figures (76.0% and 40.3%, p<0.001) in 2022. Regarding knowledge on which common conditions were needed for antibiotics, there was major improvement in knowledge that cold and flu needed no antibiotics, from 49.7% to 83.3%, p<0.001, while fewer respondents answered correctly for urinary tract infection and skin and wound infection. A slight drop from 44.1% in 2022 to 39.2% in 2023 was noted for respondents who could answered correctly that resistant bacteria could be spread from person-to-person. On attitude, among the respondents in 2023, vast majority (94.7%) of the respondents would accept the doctor’s advice to observe for a few more days or to wait for the diagnostic test result before deciding whether to prescribe antibiotics or not, despite it was slightly less than that (96.4%, p<0.006) in 2022. On the other hand, only a small portion (about 5%) of respondents preferred consulting doctors who would prescribe antibiotics more readily in both years. It was glad to see that only a minority (2.6% in 2022 and 3.6% in 2023) of respondents had asked for antibiotics during the last medical consultation for cold or flu. When asked whether the respondents always practiced the health advice during the last taking of antibiotics, a range of 62.8% to 89.6% of respondents did follow the infection control practice (e.g. practice hand hygiene, disinfect and cover all wounds) to prevent further spread of resistant bacteria in 2023. There was an improvement in wearing mask (72.3% to 77.3%, p<0.001) while the percentage of other personal hygiene practices were similar to that of 2022 (Tables 1-5).
| Year (column%) | p-value | ||
|---|---|---|---|
| 2022 | 2023 | ||
| Survey timeline and sample size | |||
| Period of interview | 7 September, 2022 to 06 October, 2022 | 27 November, 2023 to 08 January, 2024 | - |
| Sample size | 1,076 | 1,083 | - |
| Contact method (weighted) and response rate | |||
| Landline users | 34.70% | 26.10% | <0.01 |
| Mobile users | 65.30% | 73.90% | |
| Combined response rate | 32.70% | 50.10% | - |
| Sex distribution (weighted) | |||
| Female | 52.80% | 52.90% | 0.99 |
| Male | 47.20% | 47.10% | |
| Age group (weighted) | |||
| 15-24 | 8.90% | 9.30% | 0.98 |
| 25-34 | 14.10% | 13.60% | |
| 35-44 | 16.30% | 16.00% | |
| 45-54 | 17.20% | 17.00% | |
| 55-64 | 19.70% | 19.10% | |
| 65 or above | 23.70% | 25.10% | |
Table 1: Comparison of the findings between 2022 and 2023 survey-basic demographics of respondents.
| Year (column%) | p-value | ||
|---|---|---|---|
| 2022 | 2023 | ||
| Whether respondents had heard of the selected items related to antimicrobial resistance | |||
| Antibiotic resistance* | |||
| Yes | 76.00% | 66.70% | <0.01 |
| No | 23.50% | 32.50% | |
| Can't remember | 0.50% | 0.80% | |
| Antimicrobial resistance* | |||
| Yes | 40.30% | 22.60% | <0.01 |
| No | 57.90% | 76.00% | |
| Can't remember | 1.80% | 1.40% | |
| Whether respondents notice the instructions on antibiotics medicine bags† | |||
| Yes | 20.60% | 19.70% | 0.778 |
| No | 59.10% | 60.70% | |
| Can't remember | 20.40% | 19.50% | |
Note: *Weighted sample sizes for 2022 and 2023 surveys were 1,076 and 1,083, respectively. †Weighted sample sizes for 2022 and 2023 surveys were 869 and 852, respectively. Only responses from respondents aged 15 and over whose last taken antibiotics were prescribed by doctors were included for analysis.
Table 2: Comparison of the findings between 2022 and 2023 survey-awareness.
| Year (column%) | p-value | ||
|---|---|---|---|
| 2022 | 2023 | ||
| Whether respondents thought the selected health conditions need to use antibiotics*† | |||
| Bladder infection or Urinary Tract Infection (UTI) | |||
| Yes (correct) | 59.40% | 56.90% | 0.024 |
| No | 15.00% | 19.40% | |
| Don't know | 25.60% | 23.70% | |
| Cold and flu | |||
| Yes | 35.60% | 8.30% | <0.01 |
| No (correct) | 49.70% | 83.80% | |
| Don't know | 14.70% | 7.90% | |
| Skin or wound infection | |||
| Yes (correct) | 75.70% | 50.00% | <0.01 |
| No | 11.00% | 35.00% | |
| Don't know | 13.30% | 15.00% | |
| Body aches | |||
| Yes | 5.90% | 2.60% | <0.01 |
| No (correct) | 78.00% | 89.20% | |
| Don't know | 16.10% | 8.20% | |
| Headaches | |||
| Yes | 7.20% | 2.60% | <0.01 |
| No (correct) | 79.50% | 91.00% | |
| Don't know | 13.30% | 6.40% | |
| Whether respondents thought the selected statements about antibiotic resistance as true or false* | |||
| If bacteria are resistant to antibiotics, it can be very difficult or impossible to treat the infections they cause | |||
| True (correct) | 71.40% | 67.60% | 0.123 |
| False | 16.70% | 17.90% | |
| Don't know | 11.90% | 14.50% | |
| Bacteria which are resistant to antibiotics can be spread from person to person | |||
| True (correct) | 44.10% | 39.20% | 0.039 |
| False | 37.60% | 39.10% | |
| Don't know | 18.20% | 21.60% | |
Note: *Weighted sample sizes for 2022 and 2023 surveys were 1,076 and 1,083, respectively; †Caution should be taken when comparing the results, as the wording of the question differs between 2022 and 2023. In 2022, the question was "Do you think these conditions can be treated by antibiotics?" while in 2023, it was "Do you think these conditions need to use antibiotics?".
Table 3: Comparison of the findings between 2022 and 2023 survey-knowledge.
| Year (column%) | p-value | ||
|---|---|---|---|
| 2022 | 2023 | ||
| Whether respondents would accept the doctor’s advice to observe for a few more days or to wait for the diagnostic test result before deciding whether to prescribe antibiotics or not* | |||
| Yes/Accept | 96.40% | 94.70% | <0.01 |
| No/Not accept | 2.30% | 1.90% | |
| Don't know | 1.40% | 3.40% | |
| Whether respondents wanted doctors to share decision making with them on antibiotics prescription* | |||
| Yes | 66.30% | 49.50% | <0.01 |
| No | 18.90% | 30.10% | |
| Neutral | 14.90% | 20.40% | |
| Whether respondents preferred consulting doctors who would prescribe antibiotics more readily* | |||
| Yes | 5.70% | 4.80% | 0.068 |
| No | 83.30% | 81.00% | |
| Don't know/Depends on the situation | 11.00% | 14.20% | |
Note: *Weighted sample sizes for 2022 and 2023 surveys were 1,076 and 1,083, respectively.
Table 4: Comparison of the findings between 2022 and 2023 survey-attitude.
| Year (column%) | p-value | ||
|---|---|---|---|
| 2022 | 2023 | ||
| Whether respondents had asked for antibiotics during the last medical consultation for cold or flu* | |||
| Yes | 2.40% | 4.10% | 0.761 |
| No | 97.60% | 95.70% | |
| Can't remember | 0% | 0.30% | |
| Frequency of practising the health advice during the last medication period | |||
| Practise frequent hand hygiene† | |||
| Always | 60.50% | 62.80% | 0.732 |
| Seldom | 24.70% | 23.30% | |
| Never | 12.70% | 12.30% | |
| Can't remember | 2.00% | 1.60% | |
| Eat or drink only thoroughly cooked or boiled items† | |||
| Always | 92.70% | 89.60% | 0.111 |
| Seldom | 5.40% | 7.00% | |
| Never | 1.70% | 3.00% | |
| Can't remember | 0.20% | 0.40% | |
| Disinfect and cover all wounds‡ | |||
| Always | 62.20% | 64.40% | 0.219 |
| Seldom | 30.40% | 27.20% | |
| Never | 5.30% | 6.90% | |
| Can't remember | 2.10% | 1.50% | |
| Wear surgical mask if the respondent has respiratory symptoms§ | |||
| Always | 72.30% | 77.30% | <0.01 |
| Seldom | 15.20% | 16.90% | |
| Never | 10.70% | 4.80% | |
| Can't remember | 1.80% | 1.10% | |
| Young children with symptoms of infections should minimise contact with other children‖ | |||
| Always | 80.30% | 79.40% | 0.722 |
| Seldom | 11.70% | 12.80% | |
| Never | 6.60% | 7.00% | |
| Can't remember | 1.50% | 0.80% | |
Note: *Weighted sample sizes for 2022 and 2023 surveys were 232 and 506, respectively. Only responses from respondents aged 15 and over who had consulted a doctor for cold or flu in the past 12 months were included for analysis; †Weighted sample sizes for 2022 and 2023 surveys were 869 and 852, respectively; ‡Weighted sample sizes for 2022 and 2023 surveys were 869 and 788, respectively; §Weighted sample sizes for 2022 and 2023 surveys were 869 and 840, respectively; ‖Weighted sample sizes for 2022 and 2023 surveys were 519 and 517, respectively. Only responses from respondents aged 15 and over whose last taken antibiotics were prescribed by doctors and reported having young children at home were included for analysis.
Table 5: Comparison of the findings between 2022 and 2023 survey-practice.
Subgroup analysis in 2023 survey
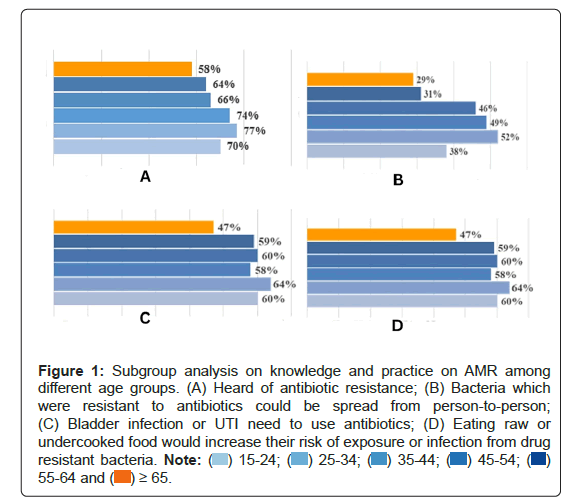
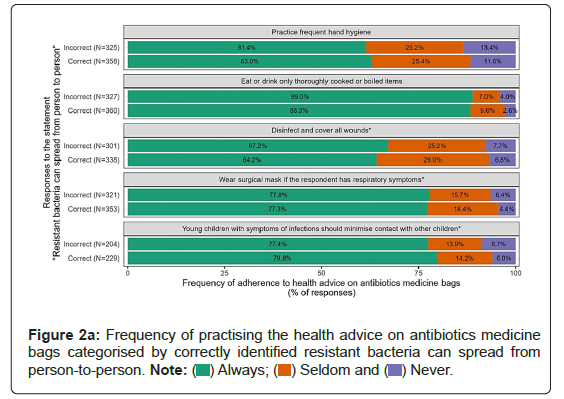
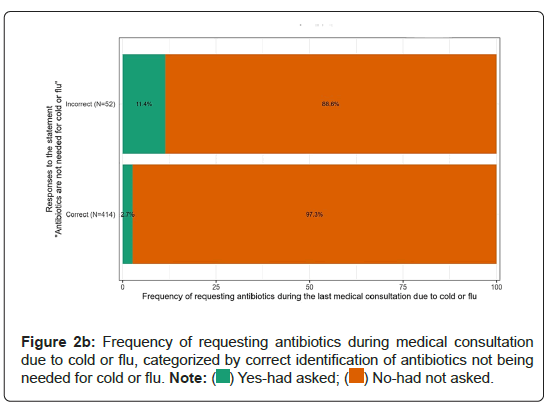
In the subgroup analysis, we found the elderly respondents had lower health literacy on AMR (Figure 1). Compared with younger age groups, fewer respondents aged 65 or above had heard of antibiotic resistant. They were found less aware that resistant bacteria could be spread from person-to-person and bladder infection or urinary tract infection required antibiotics. Besides, fewer elderly respondents knew that eating raw or undercooked food would increase their risk of exposure or infection from resistant bacteria. Additional analysis was conducted to examine the relationship between knowledge about antibiotic resistance and practising the health advice on antibiotics medicine bags. It was shown that there was no statistically significant difference in the frequency of practising the health advice between those answered correctly and those wrongly on the statement about person-to-person transmission of resistant bacteria (Figure 2a). On the other hand, respondents who correctly identified that antibiotics were not needed for cold and flu were less likely to ask for antibiotics during the last medical consultation than those who answered wrongly (2.7% vs. 11.4%, p<0.01) (Figure 2b).
Figure 1: Subgroup analysis on knowledge and practice on AMR among different age groups. (A) Heard of antibiotic resistance; (B) Bacteria which were resistant to antibiotics could be spread from person-to-person; (C) Bladder infection or UTI need to use antibiotics; (D) Eating raw or undercooked food would increase their risk of exposure or infection from drug resistant bacteria. 
Discussion
Health promotion on AMR is one of the foundations for optimizing use of antimicrobials, which in turn influence the pattern of AMR. We have evaluated the knowledge, attitude and practice related to AMR among the public, after a territory-wide campaign conducted in Hong Kong. Influenza is a strong driver for antimicrobial use [11]. We have shown significant improvement of over 30% (from 49.7% to 83.8%) in knowledge among the respondents that common cold and influenza did not require antibiotics, which was one of the key messages in our publicity campaign. The percentage (83.8%) is much higher when compared to the average of 30% (ranging from 17% to 47% in different countries) in a multi-country survey conducted by WHO [12]. In a systematic review, it has been shown that mass media campaign for health promotion in AMR is effective [13]. The use of disease-specific health promotion message is also a recommended strategy. We have included these two elements in our last publicity campaign. Our results support that better knowledge in AMR (correctly identified that antibiotics are not needed for cold and flu) is associated with more appropriate behaviour (not to ask for antibiotics during the medical consultation). Nevertheless, the survey finds room for improvement in some of the areas in public education on AMR. For example, less than half of the respondents knows that resistant bacteria can spread from person-to-person, about two-third of the respondents have heard of antibiotic resistance and only about one-fifth of the respondents are aware of the health advice printed in the medicine bags.
In the 2023 survey, we find if the doctors’ initial assessment indicated antibiotics are not needed, over 96% of the public would accept doctors’ advice. Besides, only a small portion (about 5%) of respondents prefers consulting doctors who would prescribe antibiotics more readily in both years. This information is useful to reassure the doctors not to feel pressure to prescribe any unnecessary antibiotics. In fact, after we conducted the 2022 survey, we have shared these results to our doctors to solicit their support in appropriate use of antibiotics [14]. As mentioned in a systematic review, engaging doctors in the patient education is also named as one of the key successful factors in the publicity campaign [13].
In the subgroup analysis, we find that elderly has lower health literacy in AMR. Similar observations are found in other studies. For example, in a cross-sectional survey involving respondents aged 60 years and above, more than half (53.5%) of the respondents incorrectly believe that antibiotics can treat viral infections [15]. Lack of knowledge and awareness is identified as a large contributor to the misuse of antibiotics and is predominantly determined by both education level and accessibility to public information [16]. Older adults are more likely to overestimate their AMR knowledge, with the belief that having previously taken specific antibiotics for familiar symptoms meaning that they could take them again with or without a prescription [17,18]. Reasons for antibiotic misuse amongst older adults include having more medication than needed, feeling better, experiencing side effects, forgetting to take them, or feeling no difference in symptoms, with over 65% of older adults keeping their leftover antibiotics for themselves [19]. More tailor-made, easy-to-understand health promotion messages on AMR should be designed and targeted for this special group of population.
Conclusion
This evaluation shows publicity campaign on AMR has increased public knowledge on appropriate use of antibiotics, which influence people’s behaviour in antibiotic utilization and in turn affects the resistance pattern of bacteria. Targeted messages should be designed and promulgated to address knowledge deficit and specific population subgroups such as elderly to combat AMR.
Limitations
There are strengths and limitations of this study. The surveys are conducted territory-wide with representative samples from Hong Kong and good response rates. These surveys can provide longitudinal data to track the knowledge, attitude and practice among the general public in the future. Yet, there are several limitations. First, these are selfreport surveys and data cannot be verified. Second, the response rate in 2023 is higher than that of 2022, which may possibly affect results if non-respondents are less educated on knowledge of AMR. Third, some questions need to be interpreted with caution since there is slight adjustment of the questions compared with those in 2022.
Ethics Approval
Ethics approval is considered not necessary as the survey only collected anonymized and non-identifiable data.
Competing Interests
None declared.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
We would like to thank you the team in The Chinese University of Hong Kong (CUHK) in conducting the field work and data collation.
References
- McNulty CA, Nichols T, French DP, Joshi P, Butler CC (2013) Expectations for consultations and antibiotics for respiratory tract infection in primary care: The RTI clinical iceberg. Br J Gen Pract 63:e429-e436.
[Crossref] [Google Scholar] [PubMed]
- Mazinska B, Struzycka I, Hryniewicz W (2017) Surveys of public knowledge and attitudes with regard to antibiotics in Poland: Did the European antibiotic awareness day campaigns change attitudes? PLoS ONE 12:e0172146.
[Crossref] [Google Scholar] [PubMed]
- Khoshgoftar M, Zamani-Alavijeh F, Kasaian N, Shahzamani K, Rostami S, et al. (2021) The effect of public health educational campaign regarding antibiotic use and microbial resistance on knowledge, attitude and practice in the Iran. J Educ Health Promot 10:3.
[Crossref] [Google Scholar] [PubMed]
- Filippini M, Ortiz LG, Masiero G (2013) Assessing the impact of national antibiotic campaigns in Europe. Eur J Health Econ 14:587-599.
[Crossref] [Google Scholar] [PubMed]
- Chaintarli K, Ingle SM, Bhattacharya A, Ashiru-Oredope D, Oliver I, et al. (2016) Impact of a United Kingdom-wide campaign to tackle antimicrobial resistance on self-reported knowledge and behaviour change. BMC Public Health 16:393.
- Ho ML, Cowling BJ, Seto WH, Wong LC, Wong TY (2014) Determinants of an effective antibiotic campaign: Lessons from Hong Kong. J Glob Antimicrob Resist 2:334-337.
[Crossref] [Google Scholar] [PubMed]
- Parveen S, Garzon-Orjuela N, Amin D, McHugh P, Vellinga A (2022) Public health interventions to improve antimicrobial resistance awareness and behavioural change associated with antimicrobial use: A systematic review exploring the use of social media. Antibiotics (Basel) 11:669.
[Crossref] [Google Scholar] [PubMed]
- Centre for Health Protection (2024) Hong Kong Strategy and Action Plan on Antimicrobial Resistance 2023-2027.
- Bankier MD (1986) Estimators based on several stratified samples with applications to multiple frame surveys. J Am Stat Assoc 81:1074-1079.
- Wong KT, Zheng V, Wan P (2022) Using a dual-frame design to improve phone surveys on political attitudes: developing a weighting strategy for limited external information in Hong Kong. Qty Quan 56:2387-2414.
- Barchitta M, Maugeri A, Vinci R, Agodi A (2022) The inverse relationship between influenza vaccination and antimicrobial resistance: An ecological analysis of Italian data. Vaccines (Basel) 10:554.
- World Health Organization (2015) Antibiotic resistance: Multi-country public awareness survey.
- Gilham EL, Pearce-Smith N, Carter V, Ashiru-Oredope D (2024) Assessment of global antimicrobial resistance campaigns conducted to improve public awareness and antimicrobial use behaviours: A rapid systematic review. BMC Public Health 24:396.
[Crossref] [Google Scholar] [PubMed]
- Centre for Health Protection (2023) Letter-to-doctor: Stay vigilant against antibiotic resistance.
- Kong LS, Islahudin F, Muthupalaniappen L, Chong WW (2019) Knowledge and expectations on antibiotic use among older adults in Malaysia: A cross-sectional survey. Geriatrics (Basel) 4:61.
[Crossref] [Google Scholar] [PubMed]
- Hawkins O, Scott AM, Montgomery A, Nicholas B, Mullan J, et al. (2022) Comparing public attitudes, knowledge, beliefs and behaviours towards antibiotics and antimicrobial resistance in Australia, United Kingdom and Sweden (2010-2021): A systematic review, meta-analysis and comparative policy analysis. PLoS ONE 17:110-123.
[Crossref] [Google Scholar] [PubMed]
- Grigoryan L, Germanos G, Zoorob R, Juneja S, Raphael J, et al. (2019) Use of antibiotics without a prescription in the U.S. population. Ann Intern Med 171:257-263.
[Crossref] [Google Scholar] [PubMed]
- Smith CA, Chang E, Gallego G, Khan A, Armour M, et al. (2019) An education intervention to improve decision making and health literacy among older Australians: A randomised controlled trial. BMC Geriatr 19:129-140.
[Crossref] [Google Scholar] [PubMed]
- Malani P, Solway E, Kirch M, Singer DC, Kullgren JT (2021) Use and perceptions of antibiotics among US adults aged 50-80 years. Infect Control Hosp Epidemiol 42:628-629.
[Crossref] [Google Scholar] [PubMed]
Citation: Ma E, Hsu E, Chow T, Ko LS, Lau KY, et al. (2024) Change in Public Knowledge, Attitude and Practice on Antibiotic use After a Territory-Wide Health Promotion Campaign in Hong Kong. J Infect Dis Ther 12:604. DOI: 10.4172/2332-0877.1000604
Copyright: © 2024 Ma E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1626
- [From(publication date): 0-2024 - Nov 14, 2025]
- Breakdown by view type
- HTML page views: 1257
- PDF downloads: 369