Cervical spine stenosis and myelopathy secondary to posterior longitudinal ligament ossification
Received: 08-May-2021 / Accepted Date: 13-May-2021 / Published Date: 20-May-2021 DOI: 10.4172/2167-7964.1000328
Abstract
Posterior longitudinal ligament ossification is one of etiology of cervical myelopathy. We report in this article image a case of 80-years-old man with bilateral neuralgia with C6 root palsies. CT scan is the gold standard imagery for the diagnosis. The treatment depends on many parameters dealing with the level of compression as well as the severity of the symptoms
Keywords: cervical spine- posterior longitudinal ligamentossification
Text
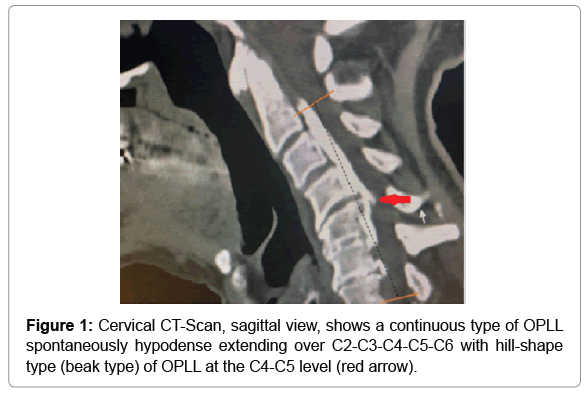
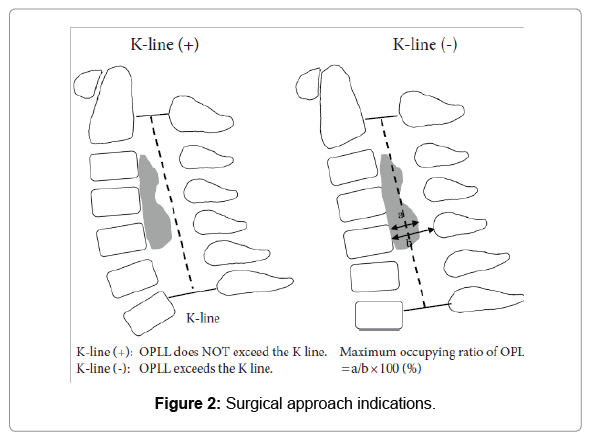
Ossification of the posterior longitudinal ligament (OPLL) is an important cause of cervical myelopathy that results from bony ossification of the cervical or thoracic posterior longitudinal ligament (PLL). It has been estimated that nearly 25% of patients with cervical myelopathy will have features of OPLL [1]. We report a case of 80-years-old man admitted in the neurological surgery department for cervico-brachial neuralgia with bilateral C6 root palsies. There were no other neurological findings associated. His past medical history was unremarkable. Cervical CT-Scan, sagittal view, shows a continuous type of OPLL extending over C2-C3-C4-C5-C6. The lesion is spontaneously hypodense with a broken sign, visible as a crack in ossification of the posterior longitudinal ligament plaque and also a hill-shape type (beak type) of OPLL at the C4-C5 level (Red arrow) Figure 1. The continuous type represents 25.97% of OPLL. The decision to treat these lesions is challenging. Various radiological parameters are used to evaluate cervical OPLL and to determine the surgical strategy Figure 2 [2]. For example, Fujiyoshi et al.[3] suggested that in the K-line (-) group, posterior decompression surgery would be unable to achieve a satisfactory posterior shift of the spinal cord and thus satisfactory neurologic improvement. Our patient is in this group. Moreover, looking at the patient advanced age, the decision for treatment or conservative management is very tricky. But the good news is that many other possibilities such as the anterior resection for OPLL with or without wide corpectomy and fusion or anterior and posterior combined surgery may be considered.
References
- Smith ZA, Buchanan CC, Raphael D, Khoo LT (2011) Ossification of the posterior longitudinal ligament:npathogenesis, management, and current surgical approaches: a review. Neurosurgical focus 30(3):E10.
- Shimokawa N, Sato H, Matsumoto H, Takami T (2019) Review of radiological parameters, imagingncharacteristics, and their effect on optimal treatment approaches and surgical outcomes for cervical ossification of thenposterior longitudinal ligament. Neurospine 16(3):506.
- Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, etnal. (2008) A new concept for making decisionsnregarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spinen(Phila Pa 1976) 33(26):E990-993.
Citation: Hugues DYC, Thierry YTR, Miloud G (2021) Cervical Spine- Posterior Longitudinal Ligament- Ossification. OMICS J Radiol 10: 328. DOI: 10.4172/2167-7964.1000328
Copyright: © 2021 Hugues DYC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3357
- [From(publication date): 0-2021 - Dec 21, 2025]
- Breakdown by view type
- HTML page views: 2459
- PDF downloads: 898