Case Report Open Access
Cerebral Aneurysm in Lyme Neuroborreliosis with Regression After Medical Treatment
Jonathan Tiu1*, Richard M Hanson2 and Robert Staudinger21Department of Neurology, School of Medicine, New York University, USA
2Department of Neurology and Veterans Affairs NYHHS, School of Medicine, New York University, USA
- *Corresponding Author:
- Jonathan Tiu
Department of Neurology
School of Medicine, New York University, USA
Tel: 16319353534
E-mail: jonathan.tiu@nyumc.org
Received date: May 27, 2017; Accepted date: June 13, 2017; Published date: June 16, 2017
Citation: Tiu J, Hanson RM, Staudinger R (2017) Cerebral Aneurysm in Lyme Neuroborreliosis with Regression After Medical Treatment. J Neuroinfect Dis 8: 252. doi:10.4172/2314-7326.1000252
Copyright: © 2017 Tiu J, et al. This is an open-access article distributed under the terms of the creative commons attribution license, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Visit for more related articles at Journal of Neuroinfectious Diseases
Abstract
Lyme disease in the United States is caused predominantly by the spirochete Borrelia burgdorferi and affects multiple organ systems. Lyme Borreliosis infrequently involves the peripheral and central nervous system, and the term Neuroborreliosis is used for the latter case. The most common manifestations of Neuroborreliosis include cranial neuropathy and lymphocytic meningitis. It can also cause cerebral vasculitis leading to both wall thickening and endothelial obliteration. Other manifestations include stroke, with over 50 documented cases, and rarely nonaneurysmal subarachnoid hemorrhage and intraparenchymal hemorrhage.
Intracranial aneurysm detected in the setting of Lyme Borreliosis infection has been previously documented in four cases [3,4]. However, the existence of a causal relationship between Lyme infection and intracranial aneurysm has been debated. We discuss these cases, and present our own case of a man with Lyme Neuroborreliosis with an intracranial aneurysm which regressed upon completion of treatment with ceftriaxone.
Keywords
Lyme neuroborreliosis; Cerebral aneurysm; Mycotic aneurysm; Infectious Vasculitis
Case Report
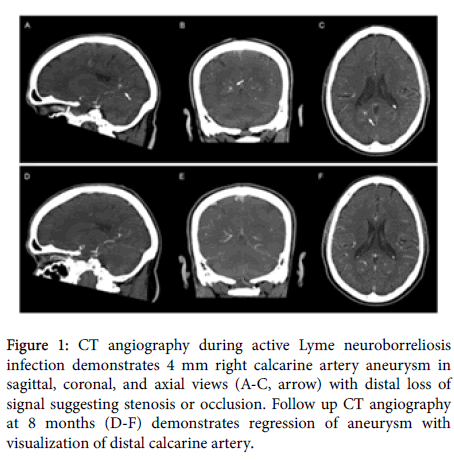
A 62-year-old right handed man presented with three days of double vision, gait instability, fever, and headache. The neurological examination showed a Horner syndrome and dysmetria on the right side, dysarthria, as well as gait ataxia. An urgent lumbar puncture was performed, revealing xanthochromic fluid with 313 WBCs (70% lymphocytes) and 770 RBCs, a protein content of 64.2 mg/dl and glucose of 57 mg/dl (serum glucose 147 mg/dl). The patient was started empirically on acyclovir, ampicillin, vancomycin, and ceftriaxone [1]. MRI showed acute infarcts in the right dorsal midbrain and a small cortically based area of enhancement in the right parietooccipital area. Adjacent to the latter lesion, MR angiography showed an aneurysm of the right calcarine artery. CT angiography two days later showed the aneurysm to be 4 mm (Figure 1). It also demonstrated distal calcarine artery narrowing and focal stenosis of the right superior cerebellar artery. CSF gram stain and cultures were negative. PCR for HSV-1, EBV, VZV, serology for West Nile virus, lymphocytic choriomeningitis virus and listeria, as well as VDRL were negative. A transesophageal echocardiogram was negative for vegetations, and bacterial blood cultures were negative. Inflammatory markers and PCR for HIV-1 were negative [2-4]. CSF ELISA and Western blot returned positive for Lyme, with 6 out of 10 Lyme specific IgG bands on Western Blot, but negative IgM. Lyme antibodies from serum are not available for calculation of the antibody index. Further history revealed that the patient had traveled to Western Pennsylvania several months before admission, but did not report a tick bite or rash. He had no history of previous Lyme disease. The patient was treated for presumed neuroborreliosis with ceftriaxone for four weeks, with an excellent clinical response and resolution of CSF pleocytosis. His neurological symptoms also resolved within several months of onset. Repeat CT angiography seven months after admission showed regression of the aneurysm and resolution of focal arterial stenoses.
Figure 1: CT angiography during active Lyme neuroborreliosis infection demonstrates 4 mm right calcarine artery aneurysm in sagittal, coronal, and axial views (A-C, arrow) with distal loss of signal suggesting stenosis or occlusion. Follow up CT angiography at 8 months (D-F) demonstrates regression of aneurysm with visualization of distal calcarine artery.
Discussion
We report a patient with Lyme borreliosis who developed a lymphocytic meningitis and vasculitis resulting in midbrain infarction and aneurysm formation. The diagnosis of neuroborreliosis in this patient is supported by proposed criteria [5]. The causal relation between B. burgdorferi and cerebral aneurysm formation is only based on circumstantial evidence, and is controversial. Oksi et al. [3] initially published a case series of three patients with Lyme borreliosis and intracranial aneurysm, leading the authors to suggest Lyme mediated vasculitis as a mechanism of intracranial aneurysm formation.
In response, Polet et al. [4] published a report of a man with headache and anterior stroke due to neuroborreliosis whose angiography demonstrated a basilar aneurysm and cerebral vascular narrowing. They suggested that the aneurysm was coincidental, and that a causal link between borreliosis and aneurysm could not be established. Our case supports the conclusion that neuroborreliosis can be associated with cerebral aneurysm formation. Our patient had a dramatic response to antibiotic treatment with resolution of clinical, laboratory, and imaging findings. This is the first case report of regression of a cerebral aneurysm in association with Neuroborreliosis with antibiotic treatment and without neurovascular intervention. We suggest that this response supports a causal relationship. Cerebral vasculitis and aneurysm formation may be a rare complication of Lyme disease, but important for general neurologists to recognize.
Author Contributions
Jonathan Tiu, study concept and design, analysis of data, drafting of manuscript. Richard M Hanson, study concept and design, interpretation of data, revision of manuscript. Robert Staudinger, study concept and design, interpretation of data, revision of manuscript.
References
- Carod Artal FJ (2016) Clinical management of infectious cerebral vasculitides. Expert Rev Neurother 16: 205-221.
- Topakian R, Stieglbauer K, Nussbaumer K, Aichner FT (2008) Cerebral vasculitis and stroke in Lyme neuroborreliosis. Two case reports and review of current knowledge. Cerebrovasc Dis 26: 455-461.
- Oksi J, Kalimo H, Marttila RJ, Marjamaki M, Sonninen P, et al. (1998) Intracranial aneurysms in three patients with disseminated Lyme borreliosis: Cause or chance association? J Neurol Neurosurg Psychiatr 64: 636-642.
- Polet JD, Weinstein HC (1999) Lyme borreliosis and intracranial aneurysm (1999) J Neurol Neurosurg Psychiatr 66: 806-807.
- Blanc F, Jaulhac B, Fleury M, de Seze J, de Martino SJ, et al. (2007) Relevance of the antibody index to diagnose Lyme neuroborreliosis among seropositive patients. Neurology 69: 953-958.
Relevant Topics
- Bacteria Induced Neuropathies
- Blood-brain barrier
- Brain Infection
- Cerebral Spinal Fluid
- Encephalitis
- Fungal Infection
- Infectious Disease in Children
- Neuro-HIV and Bacterial Infection
- Neuro-Infections Induced Autoimmune Disorders
- Neurocystercercosis
- Neurocysticercosis
- Neuroepidemiology
- Neuroinfectious Agents
- Neuroinflammation
- Neurosyphilis
- Neurotropic viruses
- Neurovirology
- Rare Infectious Disease
- Toxoplasmosis
- Viral Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 5332
- [From(publication date):
June-2017 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 4393
- PDF downloads : 939