Cerebral Abscess Caused by Streptococcus agalactiae: An Unusual Presentation
Received: 10-Dec-2018 / Accepted Date: 20-Feb-2019 / Published Date: 28-Feb-2019 DOI: 10.4172/2167-7964.1000306
Abstract
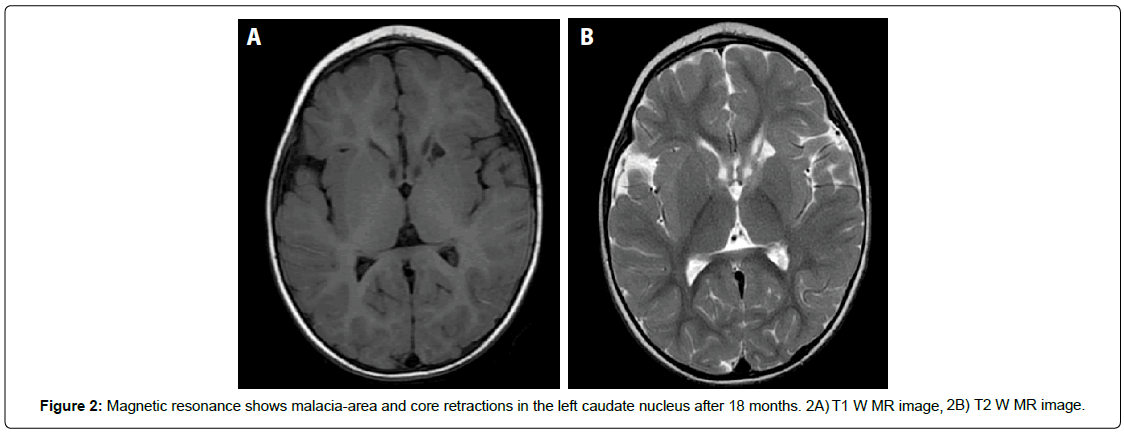
During the first three months of life, Group B streptococcus or Agalactiae (GBS) can cause meningitis and be associated with cerebrovascular accidents resulting from sepsis and infection of the central nervous system. This article presents the unusual case of a female infant who was afflicted with GBS, meningitis, sepsis complicated by septic shock, ischemic lesions secondary to inflammatory vacuities and a cerebral abscess accompanied by epileptic seizures with a hypsarrythmia electroencephalographic pattern. A long-term NICU stay with antibiotic management, inotropic support and antiepileptic treatment succeeded in resolving the acute stage of the illness. Out-patient follow-up revealed increased muscle-tone but delayed neurological development. While this improved significantly with integral rehabilitative therapy, a slight delay still remained. Neuroimaging follow-up at 18 months found malacia-area and core retractions in the left caudate nucleus.
Keywords: Brain abscess; Cerebral abscess; Group B streptococcus; Streptococcus agalactiae; Meningitis; Infant
Introduction
Group B streptococcus (GBS) belongs to a group of gram-positive bacteria that can colonize the digestive and urinary tracts of children and adults, without causing pathology. In infants, however, it can lead to morbidity and mortality in the first three months of life. During this period, and especially latter part of it, GBS can cause meningitis and can be associated with cerebrovascular accidents resulting from sepsis and infection of the central nervous system. When GBS is found during the first week of life, it is classified as early-onset, whereas infection between the 7th and 89th days of life is considered late-onset.
Case Report
A 48-day-old infant, born at 40 weeks through vaginal delivery, and was admitted to the emergency department for irritability and a 102.2°F fever (39.0°C). A focal seizure ensued, which then became generalized. A lumbar puncture found evidence of hyperproteinorrachia, pleocytosis with a predominance of neutrophil polymorph nuclear cells, and isolated group B streptococcus. The patient`s condition worsened into hypo dynamic septic shock refractory to crystalloid, and in response to this, she was given inotropic support, antibiotic treatment (ampicillin), and phenobarbital.
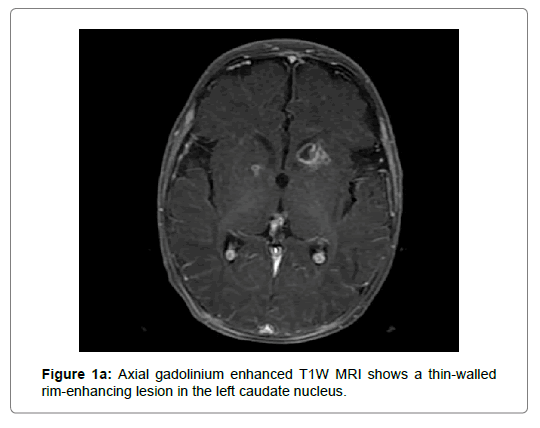
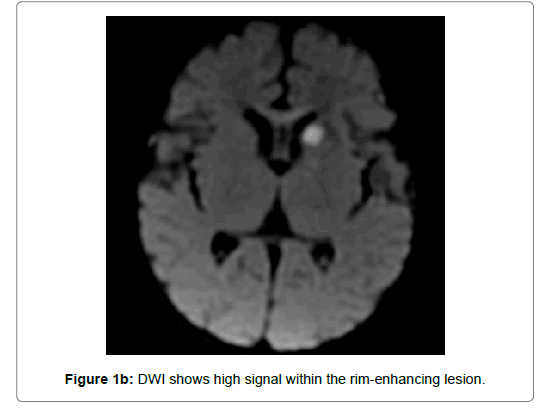
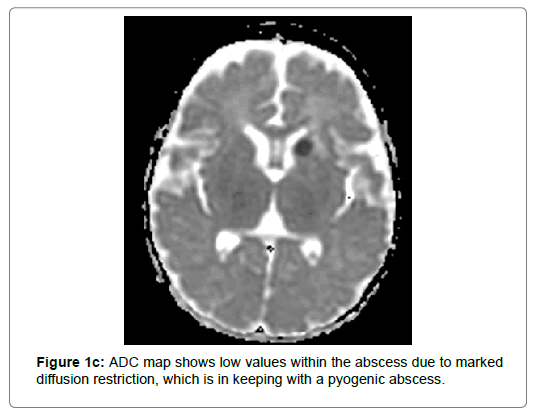
A cerebral MRI done on day 4 of the illness revealed a ring-enhancing lesion in the left caudate nucleus. This lesion displayed central low T1 and primary high T2 signals, as well as marked restricted diffusion, all of which were indicative of a pyogenic abscess (Figures 1a-1c). Images also revealed ischemic lesions in the left thalamus, ipsilateral cerebral peduncle, and right occipital peritrigonal area. An initial electroencephalogram performed after receiving 20 days of inotropic support revealed paroxysmal activity with irregular, sharp spikes and waves, as well as multifocal polypuntas that fragmented the background pattern (hypsarrythmia). In response to this, antiepileptic management with vigabatrin was started.
On the 35th day, both clinical observation and imagining showed that the patient had overcome the acute stage of the illness. At this time, antibiotic treatment ended and the patient was put on vigabatrin. Out-patient follow-up subsequently noted increased muscle tone, but delayed neurodevelopment, and integral rehabilitative therapy was initiated. After 18 months of rehabilitative therapy and vigabatrin treatment, neurodevelopment improved significantly, although a slight delay in neurodevelopment still persisted. An electroencephalogram taken at this time was normal, and vigabatrin was discontinued. Finally, a concurrent MRI showed only malacia-area and core retractions in the left caudate nucleus (Figure 2).
Discussion
The acquisition of GBS tends to be connected with the following factors. Early-onset GBS is transmitted vertically from mother to newborn. Late-onset GBS (LGBS), on the other hand, is acquired vertically or horizontally, and is more common in cases of prematurity and female sex [1-3]. Two predisposing risk factors may be immunodeficiency and prolonged stay in the neonatal care unit [4]. In less than 50% of cases, GBS in infants is due nosocomial from health workers or maternal infection passed on through contaminated breast milk [1-3]. The cause of our patient´s late-onset GBS was not clear.
Independent of its mode of acquisition, late-onset GBS is often accompanied by meningitis, and when seen together, the two are called group B streptococcal meningitis (GBSM) [1-3]. Although the initial symptoms of meningitis are subtle and non-specific, its mature symptoms usually appear acutely and progress rapidly. Common symptoms which were experienced by our patient include: onset of epileptic crisis, irritability, complications after hospital admission (in up to 62% of cases), brain abscess, and delay in neurodevelopment (in up to 61% of cases) [1,2,5]. Other common symptoms, which were not experienced by our patient, are: venous sinus thrombosis and bulging of the fontanelle, which latter typically appears later and is associated with a worse outcome [5].
The commonness of ischemic strokes in infants afflicted by late-onset GBSM is suggested by the following results. A study of fourteen infants with late-onset GBSM found that two had ischemic arterial strokes from venous sinus thrombosis, ten had ischemic arterial strokes in varying locations, and six experienced moderate to severe neurodevelopmental delay [6]. For this population of patients, two patterns of focal ischemia have been identified. One affects the cortical surface in patches and is associated with the development of severe neurological disabilities and death. The other affects the basal ganglia, thalamic, and periventricular white matter [7]. Our patient´s ischemic lesions correspond more to the second pattern, as they occurred in the left thalamus, the ipsilateral cerebral peduncle, and the right occipital peritrigonal area.
We found one case in the literature, in which the patient had nine injuries along the temporal, parietal and occipital lobes with significant mass effect and obstructive hydrocephalus, which required surgical drainage, corticosteroid therapy, and antibiotics [4].
Meningitis is diagnosed from a complete clinical history and physical examination confirmed by evaluation of the cerebrospinal fluid. Two important signs to look are neurological focalization and inadequate response to antibiotic therapy, which could suggest hydrocephalus, abscesses, or empyemas. When suspected, it is generally recommended to exclude intracranial hypertension before performing a lumbar puncture [8].
Neuroimaging helps find associated complications suspected from the clinical signs. Early findings from brain computed tomography can be mild ventriculomegaly and increased subarachnoid spaces [8]. MRI findings can detect brain abscesses and can vary with time. The early cerebritis stage shows a poorly defined subcortical hyperintense zone that can be observed on T2-weighted imaging [9,10]. Lesions appearing hyperintense on diffusion-weighted imaging with apparent-diffusion- coefficient (ADC) values of 2 are more likely to be non-abscess cystic lesions [9]. Contrast-enhanced T1-weighted studies demonstrate poorly delineated enhancing areas within the isointense to mildly hypointense edematous regions [9].
During the late cerebritis stage, the central necrotic area is hyperintense to brain tissue in the proton-density and T2-weighted sequences. The thick, somewhat irregularly marginated rim appears isointense to mildly hyperintense on spin-echo T1-weighted images and isointense to relatively hypointense on proton-density and T2- weighted scans. Rim enhances after contrast administration, peripheral edema and satellite lesions can be observed [9].
During both the early and late capsule stages, the collagenous abscess capsule is visible prior to contrast as a comparatively thin-walled, isointense to slightly hyperintense ring that becomes hypointense on T2-weighted MRIs [10], with marked diffusion restriction on diffusion-weighted images (high DWI signal and low values in the ADC maps within the abscess). If a cerebral abscess ruptures into the ventricular system, purulent material within the ventricle appears similar to that within the central abscess cavity, with diffusion restriction on DWI [9].
For treatment, use of broad-spectrum antibiotics should be established empirically. Antibiotics typically used are third or fourth generation cephalosporins (ceftriaxone or cefepime), vancomycin, and metronidazole. Subsequent treatment should be selected according to the pathogen and antibiotic sensitivity. The isolated pathogen usually responds to penicillin or ampicillin. The duration of therapy is four to six weeks for abscesses treated surgically and six to eight weeks for patients who only receive medication. When the abscess measures less than 2.5 cm in diameter or when there are multiple small abscesses, treatment with medication without surgical intervention is recommended. Patients with brain abscesses less than 2.5 cm treated only with antibiotics should see improvement [10].
Systematic review and meta-analysis show that, long-term 32% of patients with a history of group B streptococcal meningitis had alterations in neurodevelopment at the time of their 18-month followup. In 18% of these patients, these alterations are moderate to severe. The long-term evolution of patients with cerebral abscesses is unknown [11]. Our patient experienced a slight delay in neurodevelopment, which improved with rehabilitative therapy. Factors that have been related to death or severe deterioration are seizures, severe alteration of the state of consciousness, respiratory distress, bulging fontanelle, leukopenia, acidosis, hyperproteinorraquia higher than 300 mg/dl, hypoglucorraquia less than 20 mg/dl, and a need for ventilatory support [12].
Conclusion
When GBS occurs in the first three months of life, there is a high probability of it being accompanied by neurological complications, such as cerebrovascular events related to inflammatory arteriopathy and brain abscesses. If neurological focalization is observed, these should be suspected and checked for with a magnetic resonance study of the brain performed in a timely manner.
References
- Zeng SJ, Tang XS, Zhao WL, Qiu HX, Wang H, et al. (2016) Clinical analysis of cases of neonatal Streptococcus agalactiae sepsis. Genet Mol Res 15: 2.
- Bartlett AW, Smith B, George CR, McMullan B, Kesson A, et al. (2017) Epidemiology of late and very late onset group B Streptococcal disease. Pediatr Infect Dis J 36: 20-24.
- Morgan K, Baca N (2010) Late-onset group B Streptococcal meningitis in infants. Pediatr Neurol 53: 175-176.
- Pasternak JD, Fulford M, Gunnarsson T, Provias J, Singh SK (2009) An unexpected intracranial pressure crisis: Infant brain abscess of unusual aetiology. Child Nerv Syst 25: 377-381.
- Lawrence CK, Boggess KA, Wolkowiez M (2015) Bacterial meningitis in infants: Clinics in Perinatology. Clin Perinatol 42: 29-45.
- Tibussek D, Sinclair A, Yau I, Teatero S, Fittipaldi N, et al. (2015) Late-onset group B streptococcal meningitis has cerebrovascular complications. J Pediatr 166: 1187-1192.
- Hernández MI, Sandoval CC, Tapia JL, Mesa T, Escobar R (2011) Stroke patterns in neonatal group B streptococcal meningitis. Pediatr Neurol 44: 282-288.
- Parmar H, Ibrahim M (2012) Pediatric intracranial infections. Neuroimaging Clin 22: 707-725.
- Bonfield CM, Sharma J, Dobson S (2015) Pediatric intracranial abscesses. J Infect 71: S42-S46.
- Kohli-Lynch M, Russell NJ, Seale AC, Dangor Z, Tann CJ (2017) Neurodevelopmental impairment in children after group B streptococcal disease worldwide: Systematic review and meta-analyses. Clinical infectious diseases.65: S190-199.
- Libster R, Edwards KM, Levent F, Edwards MS, Rench MA (2012) Long-term outcomes of group B streptococcal meningitis. Pediatrics 130: e8-e15.
Citation: Fuentes A, Charry M, Donato A (2019) Cerebral Abscess Caused by Streptococcus agalactiae: An Unusual Presentation. OMICS J Radiol 8:306 DOI: 10.4172/2167-7964.1000306
Copyright: © 2019 Fuentes A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 4828
- [From(publication date): 0-2019 - Nov 21, 2025]
- Breakdown by view type
- HTML page views: 3905
- PDF downloads: 923