Research Article Open Access
Cephalometric Analysis of the Velopharyngeal Muscular Triangle as a Possible Prognostic Factor for Velopharyngeal Closure in Submucous Cleft Palate
Masahiro Tezuka1, Yuichi Tamatsu2, Naoko Miura3, Toshiro Kibe1, Kazuhide Nishihara4 and Norifumi Nakamura1*1Department of Oral and Maxillofacial Surgery, Field of Maxillofacial Rehabilitation, Kagoshima University Graduate School of Medical and Dental Sciences, Japan
2Department of Gross Anatomy, Field of Neurology, Kagoshima University Graduate School of Medical and Dental Sciences, Japan
3Division of Rehabilitation, Division of Clinical Technology, Kagoshima University Medical and Dental Hospital, Japan
4Department of Oral and Maxillofacial Functional Rehabilitation, Graduate School of Medicine, University of the Ryukyus, Japan
- *Corresponding Author:
- Norifumi Nakamura
Department of Oral and Maxillofacial Surgery
Field of Maxillofacial Rehabilitation
Kagoshima University Graduate School of Medical and Dental Sciences
Sakuragaoka, Kagoshima, Japan
Tel: +81-99-275-6242
E-mail: nakamura@dent.kagoshima-u.ac.jp
Received date: March 11, 2016; Accepted date: June 27, 2016; Published date: June 30, 2016
Citation: Tezuka M, Tamatsu Y, Miura N, Kibe T, Nishihara K, et al. (2016) Cephalometric Analysis of the Velopharyngeal Muscular Triangle as a Possible Prognostic Factor for Velopharyngeal Closure in Submucous Cleft Palate. J Speech Pathol Ther 1:114. doi: 10.4172/2472-5005.1000114
Copyright: © 2016 Tezuka M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Speech Pathology & Therapy
Abstract
Objective: To elucidate the anatomical characteristics of submucous cleft palate (SMCP), we analyzed the velopharyngeal (VP) structures focusing on the relationship between the position of posterior pharyngeal wall (PPW) in the VP muscles and VP closure acquisition in SMCP patients.
Methods: Cranial landmarks for cephalomatric analysis were identified in a study of two cadavers, and the area of the velopharyngeal muscular triangle (VPM-triangle), which was bordered by the origin of the levator veli palatini muscle, the origin of the palatopharyngeal muscle, and the insertion of both muscles, was defined. We then cephalometrically measured the VP structures of 14 SMCP patients (SMCP group) and the position of the PPW within the VPM-triangle. As a comparison group, 20 healthy Japanese children (control group) and 20 patients who underwent palatal repair for cleft palate (postoperative CP group) were enrolled. In addition, we analyzed the correlation between VP closure and position of the PPW within the VPM-triangle in the SMCP group.
Results: The SMCP group exhibited shorter velar length, greater pharyngeal depth and greater height. In the control and postoperative CP groups, the part of the PPW within the VPM-triangle was located near to the motion vector of the levator veli palatine muscle, while it was located significantly more posteriorly in the SMCP group. The PPW of the poor VP closure subgroup of the SMCP group tended to locate more posteriorly than those of the favorable VP closure subgroup and the control group.
Conclusions: The VP forms of the SMCP group were characterized by a shorter velum, a deeper and higher pharynx, and a more posterior PPW than the motion vector of palatal muscles. A positional discrepancy of the velopharynx including the PPW position relating to the direction of the motion of the VP muscles may influence the difficulty of VP closure achievement in SMCP patients.
Keywords
Cleft palate; Submucous cleft palate; Velopharyngeal closure; Velopharyngeal muscular triangle; Cephalometric analysis; Palatoplasty; Cleft palate speech
Introduction
Submucous cleft palate (SMCP) is a congenital condition, in which significant defects of the secondary palate occur in the absence of an actual opening into the nasal cavity. It was first reported by Roux [1] in 1825 and was named SMCP by Kelly [2] in 1910. Calnan [3] described the pathogenesis, clinical behavior, differential diagnosis, and treatment of SMCP. The main symptoms of the condition include abnormal hypernasality and articulation disorders due to velopharyngeal incompetence (VPI) [4].
There have been many reports regarding the postoperative acquisition rate of velopharyngeal (VP) closure after palatal repair in patients with SMCP, but patients often display poor speech outcomes [5-8]. Many previous authors have discussed mechanisms responsible for the difficultly of achieving favorable VP closure in SMCP patients, and they include delayed surgical intervention, neurological deficiency, and anatomical abnormalities such as a short velum, a deep or high pharynx, or a large nasopharyngeal gap [9-12]. Kaplan [13] indicated the short palate and the deep nasopharynx in SMCP patients. Sommerlad et al. [12] classified SMCP into various types according to the severity of the associated anatomical abnormalities and found that patients with less severe anatomical abnormalities achieved less satisfactory speech results. Thus, although it is understood that anatomical conditions, e.g., in the craniopharyngeal region, can contribute to the difficulty of VP closure achievement in the presence of SMCP, there still remain questions regarding why the acquisition of favorable VP closure is difficult even in cases involving small cleft, and the specific anatomical features that influence the difficulty of VP closure.
When we consider the VP closure mechanism, VP closure is controlled by synchronous and three-dimensional velopharyngeal tissue movements. The latter movements consist of upward and backward movements of the soft palate, inward movement of the lateral pharyngeal wall, and forward movement of the posterior pharyngeal wall (PPW). These motions, especially the backward and upward movements of the soft palate, are mainly controlled by the coordinating mechanism of the levator veli palatini and palatopharyngeal muscles [14,15]. Podvinec [16] explained the function of the soft palate by demonstrating the synthesized motion vectors of the levator veli palatini and palatopharyngeal muscles, and suggested that a discrepancy in craniopharyngeal growth might cause tonic contraction of the soft palate in an abnormal direction. The authors previously examined the craniopharyngeal morphology of cleft palate (CP) patients with persistent VPI and reported that anatomical discrepancies of the upper pharynx, such as a wide base and counterclockwise rotation of the pharyngeal triangle, which included the cranial base, cervical vertebrae, and posterior maxilla, were related to persistent VPI after palatal repair [17]. From the above findings, it can be hypothesized that a positional discrepancy of the synthesized motion of the levator veli palatini and palatopharyngeal muscles and PPW due to congenital craniopharyngeal growth abnormalities might make it difficult to achieve VP closure in SMCP patients.
The purpose of this study was to elucidate the reasons why it is difficult to achieve VP closure in SMCP patients. We analyzed the VP structures of SMCP patients focusing on the positional relationship between PPW and the velopharyngeal muscles. Then, we examined the relationship between these factors and VP closure acquisition in order to discuss possible prognostic factors associated with VP closure in SMCP patients.
Methods
Subjects
Fourteen patients with submucous cleft palate (SMCP), who were diagnosed and treated at the Department of Oral and Maxillofacial Surgery, Kagoshima University Medical and Dental Hospital (Kagoshima University Hospital), were enrolled and subjected to cephalometric analyses of their VP structures (SMCP group). The patients included 6 males and 8 females, and their age at the time of the cephalometric assessment ranged from 3 years and 2 months to 11 years and 8 months (mean: 6 years and 7 months) (Table 1). A diagnosis of SMCP was made when a patient exhibited Calnan’s triad: bifid uvula, translucency of the midline of the soft palate, and a Vshaped defect of the posterior edge of the hard palate [3]. Before the operation, a nasopharyngeal fiberscopic examination was performed in all patients to ensure midline defect of the nasal surface of the soft palate representing the incomplete union of palatal muscles. All of the patients were Japanese and belonged to a consecutive series of patients that visited our outpatient department between 2006 and 2013. Patients whose clinical symptoms were suggestive of 22q11.2 deletion syndrome were excluded. In addition, other syndromic patients and those with mental retardation were also excluded. A mental development test based on a questionnaire examining exercise, social skills, and language was performed, and the patients that presented with significant delays (more than one year) were considered to be mentally retarded.
| SMCP | Control | Postop CP | |
|---|---|---|---|
| No of Subjects | 14 | 20 | 20 |
| Sex distibution | |||
| Male | 6 | 10 | 9 |
| Female | 8 | 10 | 11 |
| Age (mean) at Cephalometricassesment | 3 yrs 2 mnths-11 yrs 8 mnths | 4 yrs 6 mnths-6 yrs 2mnths | 4 yrs 0 mnths-6yrs 9mnths |
Table 1: Study populations for the cephalometric analysis.
Palatal repair was performed with the modified V-Y palatoplasty procedure, which allowed conservation of the periosteum in the anterior part of the maxilla [18]. The palatal muscles were sufficiently retropositioned as they were turned sideways, producing a levator sling. To extend the nasal mucosa of the soft palate, the nasal mucosa of the soft palate was extended using a large Z-plasty and a free mucosal graft obtained from the buccal area.
As a comparison group, 20 healthy age- and sex-matched Japanese children, who had previously undergone cephalometric radiograph examinations at the Department of Pediatric Dentistry, Kagoshima University Hospital, were also enrolled in this study (control group). They included 10 males and 10 females, and their ages ranged from 4 years and 6 months to 6 years and 2 months (mean: 5 years and 7 months). Furthermore, as references, 20 patients with cleft palate (CP) solely, who had already achieved favorable VP closure after undergoing palatal repair at our department using the same palatal repair procedure, were enrolled (postoperative CP group). The patients included 9 males and 11 females, and their ages at the time of the cephalometric assessment ranged from 4 years to 6 years and 9 months (mean: 4 years and 7 months). The patients in the postoperative CP group seemed to be younger than those in the SMCP group, but there were no significant differences in the sex ratio or age among the three groups (p=0.09(SMCP vs. Controll), 0.13(Control vs. CP), and 0.08(SMCP vs. CP), respectively).
This study was approved by the clinical research ethical review board of Kagoshima University Graduate School of Medical and Dental Sciences (#93).
Comparison of cephalometric measurements of VP structures
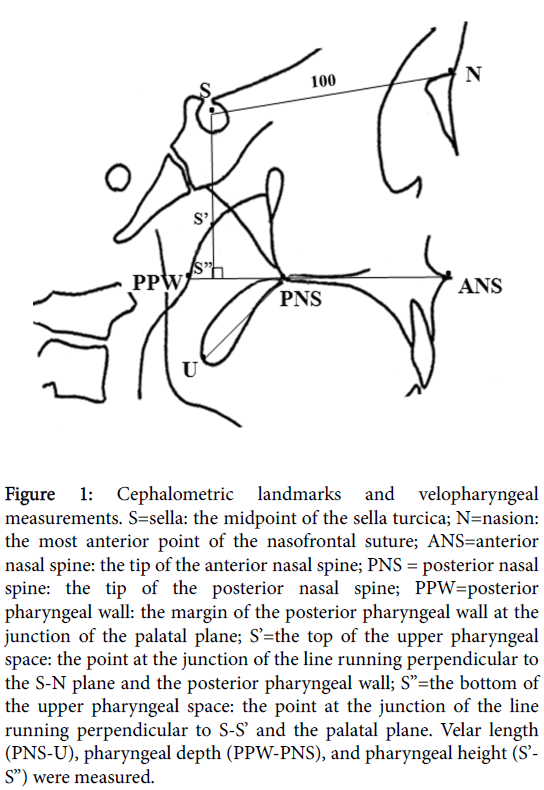
Lateral cephalometric radiographs that were obtained in a resting position were used for the analyses of craniopharyngeal morphology. The lateral cephalometric radiographs of the subjects in the SMCP group were taken before the palatoplasty was performed. The dimensions of the craniopharynx were measured by a single examiner (M.T.) to eliminate interoperator error and any operator-based bias. The skeletal landmarks and measurements were derived from tracings of the lateral cephalograms by drawing the S-N plane to create the Xaxis, and projecting a line that ran perpendicular to this plane through point S to create the Y-axis. The reference baseline and cephalometric landmarks are illustrated in Figure 1.
Figure 1: Cephalometric landmarks and velopharyngeal measurements. S=sella: the midpoint of the sella turcica; N=nasion: the most anterior point of the nasofrontal suture; ANS=anterior nasal spine: the tip of the anterior nasal spine; PNS = posterior nasal spine: the tip of the posterior nasal spine; PPW=posterior pharyngeal wall: the margin of the posterior pharyngeal wall at the junction of the palatal plane; S’=the top of the upper pharyngeal space: the point at the junction of the line running perpendicular to the S-N plane and the posterior pharyngeal wall; S”=the bottom of the upper pharyngeal space: the point at the junction of the line running perpendicular to S-S’ and the palatal plane. Velar length (PNS-U), pharyngeal depth (PPW-PNS), and pharyngeal height (S’- S”) were measured.
The measurements included velar length (PNS-U), pharyngeal depth (PNS-PPW), and pharyngeal height (S’-S”), and the ratio of velar length to pharyngeal depth (PNS-U/PNS-PPW × 100) was also calculated. As the age and sex distribution (and hence, craniofacial size) of the subjects in the CP and control groups was uneven, all craniopharyngeal dimensions were standardized relative to the length of the anterior cranial base (S-N), which was given a value of 100 (S-N revised).
Identification of anatomical landmarks relating to the motion vectors of the palatopharyngeal muscles
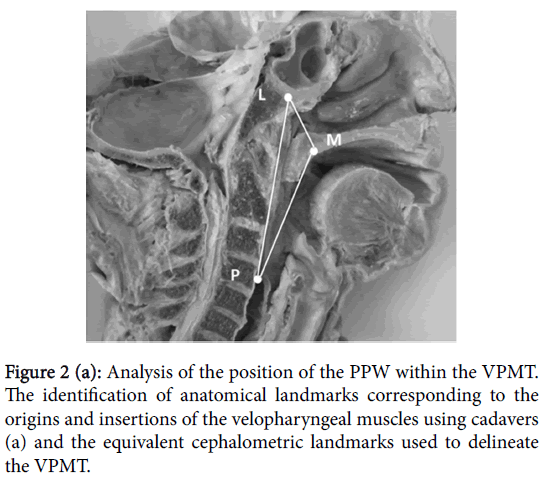
Prior to the analysis of the cephalometric analysis of VP structure, we identified landmarks that corresponded to the origin (L) and insertion (M) of the levator veli palatini muscle and the origin (P) and insertion (M) of the palatopharyngeal muscle using two cadavers (Figure 2a).
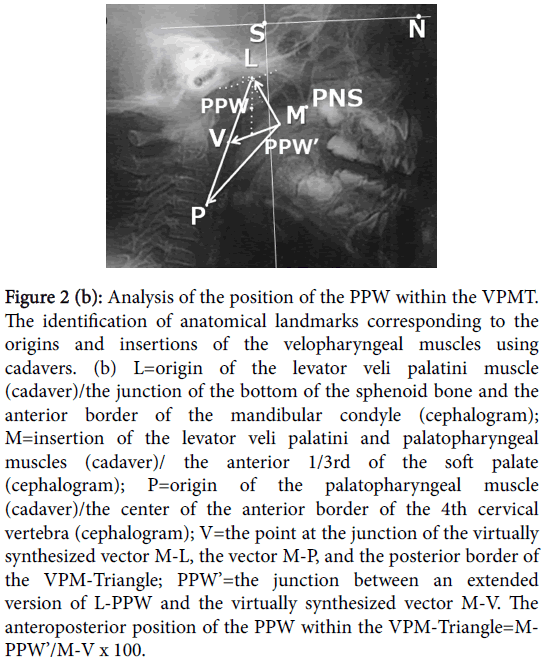
Figure 2b: Analysis of the position of the PPW within the VPMT. The identification of anatomical landmarks corresponding to the origins and insertions of the velopharyngeal muscles using cadavers. (b) L=origin of the levator veli palatini muscle (cadaver)/the junction of the bottom of the sphenoid bone and the anterior border of the mandibular condyle (cephalogram); M=insertion of the levator veli palatini and palatopharyngeal muscles (cadaver)/ the anterior 1/3rd of the soft palate (cephalogram); P=origin of the palatopharyngeal muscle (cadaver)/the center of the anterior border of the 4th cervical vertebra (cephalogram); V=the point at the junction of the virtually synthesized vector M-L, the vector M-P, and the posterior border of the VPM-Triangle; PPW’=the junction between an extended version of L-PPW and the virtually synthesized vector M-V. The anteroposterior position of the PPW within the VPM-Triangle=MPPW’/ M-V x 100.
The corresponding lateral cephalogram landmarks for the VPMtriangle were defined as follows (Figure 2b):
L: The junction of the bottom of the sphenoid bone and the anterior border of the mandibular condyle
P: The center of the anterior border of the 4th cervical vertebra
M: The anterior 1/3rd of the soft palate
V: The junction of the virtually synthesized motion vector M-L, the motion vector M-P, and the posterior border of the VPM-triangle (LP).
To analyze the anteroposterior position of the PPW within the VPM-triangle (the PPW to VPM-triangle ratio), the anteroposterior position of the point PPW’, which was the located at the junction of an extended version of L-PPW and the virtually synthesized vector M-V, was calculated using the following formula:
Anteroposterior position of PPW=M-PPW’/M-V × 100
The PPW to VPM-triangle ratio was compared among the SMCP, CP, and control groups.
The skulls of two soft embalmed cadavers were dissected at the midline. Through the sagittal plane of each hemi-face section, the origins and insertions of the levator veli palatine and palatopharyngeal muscles were identified. We then chose cephalometric landmarks that corresponded to these origins and insertions. The triangle produced by the projection of points L, M, and P on the sagittal plane of the hemi-face section was named the velopharyngeal muscular triangle (VPMtriangle).
Analysis of the relationship between the PPW to VPMtriangle ratio and VP closure achievement in the SMCP group
Postoperatively, the SMCP patients were followed-up every 3 months by two speech-language-hearing therapists (SLHT) belonging to the cleft lip and palate (CLP) team. Reliable speech assessments including of hypernasality, nasal emission, and VP closure status were performed by one SLHT (N.M.) to avoid an inter examiner error. In the speech assessment, hypernasality and nasal emission were categorized into four groups: normal, slight, moderate, and severe.
When we compared between the SMCP and postoperative CP group, the velar length was smaller, the pharyngeal depth and height Furthermore, according to the results of these assessments, VP closure status was then judged as VP competence (VPC), borderline VPC, borderline VPI, or VPI. During the speech assessments, cephalograms obtained during the phonation of the /i/ syllable, and Nasometer test data were used as references. When poor VP closure was observed postoperatively, a nasopharyngeal fiberscopic examination was performed to determine the presence/absence of an orifice between the soft palate and pharyngeal wall.
To detect possible prognostic factors for the acquisition of VP closure in SMCP patients, the PPW to VPM-triangle ratio on postoperative lateral cephalograms obtained in a resting position were compared between patients who achieved favorable VP closure, including VPC and borderline VPC, and those exhibiting poor VP closure, including borderline VPI and VPI.
Statistical analysis
The mean and standard deviation (SD) values of velar length, pharyngeal depth, pharyngeal height, velar length to pharyngeal depth ratio, and PPT to VPM-triangle ratio for all study subjects and compared among the SMCP, CP (postoperative stage), and control groups. The Mann-Whitney U-test was used to investigate differences among the 3 groups. The Kruskal-Wallis test (StatView, Hulinks, Tokyo, Japan) was employed to search for differences in velar length, pharyngeal depth, pharyngeal height, the velar length to pharyngeal depth ratio, or the PPW to VPM-triangle ratio among the SMCP, CP, and control groups.
Furthermore, the differences in the PPT to VPM-triangle ratio among the subjects that achieved favorable VP closure, those displaying poor VP closure, and the controls were compared using the same statistical methods. Significance was defined as P<0.05.
Results
Comparison of cephalometric measurements of VP structures
Table 2 shows the results of the cephalometric measurements of VP structures in the SMCP, control, and postoperative CP groups. When we compared between the SMCP and control groups, pharyngeal depth was greater and the velar length to pharyngeal depth ratio was smaller in the SMCP than in the control group (p<0.01 and <0.05, respectively).
| Measurements | SMCP (n=14) | Control (n=20) | Postop. CP (n=20) |
|---|---|---|---|
| PNS-U(Valer length) | 39.53 ± 7.09 | 42.01 ± 4.44 | 46.27 ± 6.95 |
| PNS-PPW(Pharyngeal Depth) | 39.39 ± 9.99 | 31.94 ± 6.12 | 27.84 ± 7.65 |
| S’-S”(Pharyngeal height) | 5.09 ± 4.79 | 4.80 ± 4.69 | 2.24 ± 4.09 |
| Velar length to pharyngeal depth ratio | 109.90 ± 49.78 | 138.68 ± 31.63 | 177.70 ± 59.77 |
| *: p<0.05**: p<0.01 | |||
Table 2: Comparison of cephalometric measurements of the velopharyngeal structures.
In contrast, the postoperative CP group demonstrated a significantly longer velum, a shallower and smaller (less high) pharynx, and a greater velar length to pharyngeal depth ratio than the SMCP and control groups.
Comparison of the anteroposterior position of the PPW within the VPM-triangle among the three groups
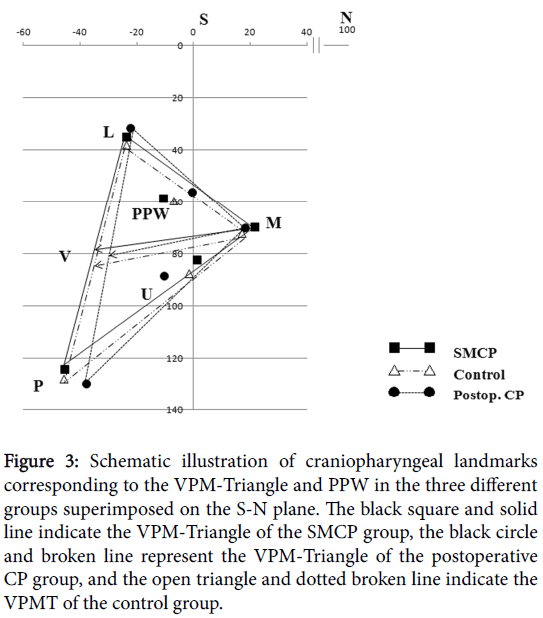
Figure 3 schematizes the mean craniopharyngeal structure measurements obtained in the three groups superimposed on the S-N plane (X-axis) and the line perpendicular to it (Y-axis).
Figure 3: Schematic illustration of craniopharyngeal landmarks corresponding to the VPM-Triangle and PPW in the three different groups superimposed on the S-N plane. The black square and solid line indicate the VPM-Triangle of the SMCP group, the black circle and broken line represent the VPM-Triangle of the postoperative CP group, and the open triangle and dotted broken line indicate the VPMT of the control group.
The form of the VPM-triangle and the position of the PPW within the VPM-triangle varied among the three groups. The VPM-triangle of the SMCP group was anteroposteriorly wider than that of the control group. The VPM-triangle of the postoperative CP group was anteroposteriorly narrower, vertically longer, and rotated counterclockwise compared with those seen in the other two groups.
Regarding the position of the PPW, the height of the PPW was almost the same in all three groups. The anteroposterior position of the PPW differed among the three groups (Figure 3). The PPW was situated near to the line running perpendicular to S-N in the postoperative CP group, and the PPW was much closer to the motion vector line L-M in the control and postoperative CP groups than in the SMCP group.
Statistical analyses of the mean (and SD) PPW to VPM-triangle ratio revealed that the ratio of the SMCP group (47.87 ± 21.95) was significantly greater than that of the postoperative CP group (33.35 ± 12.26, p<0.05) and tended to be greater than that of the control group (39.94 ±1 6.82) (Table 3). The above findings suggest that the PPW was positioned close to the motion vector of the levator veli palatini muscle in the healthy subjects and CP patients who had already acquired favorable VP closure, while it was situated more posteriorly within the VPM-triangle and further away from the synthesized motion vector of the levator veli palatini and palatopharyngeal muscles in the SMCP patients.
| SMCP (n=14) | Control (n=20) | Postop.CP (n=20) | |
| PPW to VPM-triangle ratio | 47.87 ± 21.95 | 39.94 ± 16.82 | 33.35 ± 12.26 |
Table 3: Comparison of the PPW to VPM-triangle ratio between the SMCP, control, and postoperative CP groups.
Analysis of the relationship between the PPW to VPMtriangle ratio and postoperative VP closure in the SMCP group
Speech assessments were conducted in 13 patients in the SMCP group. Because in one patient VP closure function was not stable in speech evaluation, we excluded from this evaluation. The hypernasality assessments produced the following results: normal: 4 patients, slight: 4 patients, moderate: 4 patients, and severe: 1 patient. Nasal emission was classified as follows: normal: 3 patients, slight: 5 patients, moderate: 4 patients, and severe: 1 patient. Regarding the subjects’ postoperative VP closure status, favorable VP closure was observed in 8 subjects (4 VPC and 4 borderline VPC), and poor VP closure was seen in 5 subjects (4 borderline VPI and 1 VPI). he mean and SD PPW to VPM-triangle ratios of the favorable VP closure group, poor VP closure group, and healthy children were 44.77 ± 20.93, 56.81 ± 24.10, and 39.94 ± 16.82, respectively (Table 4).
| SMCP (n=13) | Control (n=20) | ||
|---|---|---|---|
| Favourable VP clousure (n=8) | Poor VP clousure (n=5) | ||
| PPW to VPM triangle ratio | 44.77 ± 20.93 | 56.81 ± 24.10 | 39.94 ± 16.82 |
Table 4: Comparison of the PPW to VPMT ratio between the patients that exhibited favorable and poor VP closure in the SMCP and control groups.
The PPW to VPM-triangle ratio of the poor VP closure group tended to be greater than those of the favorable VP closure group and healthy children; however, the differences were not significant.
Discussion
As mentioned above, the acquisition of favorable VP closure is difficult in SMCP patients, even in those with small cleft. Actually, it is clear that the favorable VP closure acquisition rate for SMCP patients (61.5%) in this series was markedly lower than those for patients with other cleft types, when we compare these findings with the postoperative acquisition rates of VP closure after palatoplasty at our department between 2006 and 2012 [18]. This investigation was an attempt to characterize the velopharyngeal structures that may influence VP closure acquisition in SMCP patients, focusing on the coordinating mechanism of the levator veli palatini and palatopharyngeal muscles and the location of the posterior pharyngeal wall. If possible, we also hoped to identify craniopharyngeal morphological markers that could be used as possible indicators of speech outcomes following palatal repair for SMCP.
Several conclusions are thought to be warranted from our data. The first major conclusion is that the craniopharyngeal structures of SMCP patients are characterized by a short velum and a deep and high pharynx, when compared with those of age-matched healthy children and CP patients. On the other hand, although all of the CP patients were examined at the postoperative stage, the craniopharyngeal forms were quite different from those of the other subjects. For example, they demonstrated significantly longer velum and significantly shallower and smaller (in height) pharynx than the SMCP patients and healthy subjects. The above differences in the craniopharyngeal forms of the 3 groups suggest that SMCP and CP may not represent a severity continuum of anatomical soft palate abnormalities.
There have been several reports regarding the velopharyngeal morphology of SMCP patients, but there are several different opinions regarding the craniopharyngeal structures of SMCP patients. Weatherly-White [19] reported that not all SMCP patients exhibited speech disorders; therefore, VPI might be caused by not only a short palate but also the degree of development of the velar muscles. Fujita et al. [9] examined the cephalograms of 20 SMCP patients with VPI and stated that SMCP patients with VPI had significantly shorter velar. Kaplan [13] also indicated that the hard and soft palates were shorter and the nasopharynx was deeper in SMCP patients. On the other hand, Harita et al. [10] reported that a deep pharynx did not affect the risk of VPI in SMCP patients based on videofluoroscopic measurements of the velar length to pharyngeal depth ratio in 13 patients. Our present results support Fujita and Kaplan’s view that a shorter velum and a deeper pharynx are morphological characteristics of SMCP and suggest that these characteristics might affect the postoperative acquisition of VP closure.
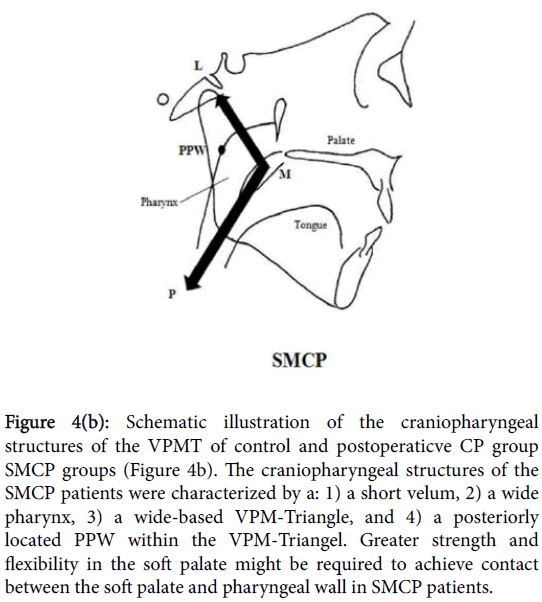
Our second major conclusion is that the VPM-triangle, which is produced by the virtually synthesized motion vectors of the levator veli palatini and palatopharyngeal muscles, was characterized by a widebased triangle and a posteriorly located PPW in the SMCP group. Prior to this study, we hypothesized that the cause of contradiction; less severe anatomical abnormalities (a smaller cleft) resulted in less satisfactory speech results in SMCP patients, might be caused by both anatomical (morphological) factors and the functional disruption of the velopharyngeal muscles. Therefore, we focused on the VPMtriangle produced by the synthesized motion vectors of the levator veli palatini and palatopharyngeal muscles because of several reasons. The first, it is well known that velar activity and VP closure together with the synthesized motion vector of the levator veli palatini and palatopharyngeal muscles [16]. Braithwaite [20] reported that the VP closure mechanism involves coordinated movement of the levator veli palatini, palatopharyngeal, and superior constrictor pharyngeal muscles, and especially the action of the former two muscles, which have the same insertion in the soft palate. The second, congenital craniofacial malformations, including cleft lip and palate, with growth disturbances and disharmony in the maxillofacial region could be a factor in VPI [21]. The authors [17] compared the pharyngeal structures of CP patients with/without VPI and found a short velum and counterclockwise rotation and wide base of the pharyngeal triangle in those with persistent VPI. These results suggested that the rotation of the pharyngeal structure could affect the difficulty of achieving sufficient VP closure in patients with CP.
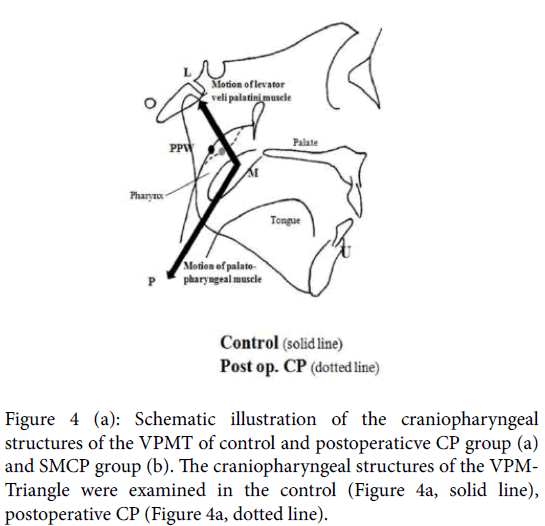
Figure 4 provides a schematic illustration of the differences in the position of the PPW within the VPM-triangle between the control or postoperative CP group and the SMCP group. In the control and postoperative CP groups, the PPW took a more anterior position in the VPM-triangle and was located close to the motion vector of the levator veli palatini muscle. When the levator veli palatini muscle constricts, the nasal surface of the soft palate can easily come into contact with the pharyngeal wall in healthy subjects (shown by the solid line in Figure 4a). Furthermore, in the postoperative CP group, in which significantly smaller pharyngeal height values were recorded, VP closure could also be achieved easily by the action of the levator veli palatini muscle (shown by the dotted line in Figure 4a). However, in the SMCP group, the PPW was located more posteriorly, as the pharynx was high and deep (Figure 4b), therefore, greater soft palate strength and flexibility might be required to enable contact between the soft palate and pharyngeal wall in SMCP patients.
Figure 4b: Schematic illustration of the craniopharyngeal structures of the VPMT of control and postoperaticve CP group SMCP groups (Figure 4b). The craniopharyngeal structures of the SMCP patients were characterized by a: 1) a short velum, 2) a wide pharynx, 3) a wide-based VPM-Triangle, and 4) a posteriorly located PPW within the VPM-Triangel. Greater strength and flexibility in the soft palate might be required to achieve contact between the soft palate and pharyngeal wall in SMCP patients.
Our final conclusion is that the anteroposterior position of the PPW within the VPM-triangle might be a prognostic factor for favorable VP closure in SMCP patients. In the present study, the PPW was locate more posteriorly within the VPM-triangle and further way from the motion vector of the levator veli palatini muscle in the SMCP group, especially in the poor VP closure subgroup. The results suggest that a positional discrepancy of the PPW relative to the direction of motion of the velopharyngeal muscles due to the disharmony of the velopharyngeal development might be one cause of the difficulty of achieving VP closure in SMCP patients. However, the significant difference was not detected in the position of PPW due to the small sample size of the present study. Therefore, further studies are necessary to develop clinically useful prognostic factors for SMCP.
This study had several limitations that should be taken into consideration when interpreting our results. The first is that the anatomical VPM-triangle landmarks, which were used in pediatric case, were established using adult cadavers. Obviously, the craniopharyngeal morphologies of adults and children might differ. However, it is very difficult to obtain child cadavers, and the mechanism responsible for closing the VP space is considered to be the same in both adults and children. Therefore, the three anatomical landmarks, L, M, and P, identified during the examinations of the adult cadavers were considered to be sufficiently reliable markers for this study. In addition, it would have been preferable to compare the preoperative VP structures of the SMCP and CP groups in order to elucidate the morphological characteristics. However, it was not possible to collect preoperative cephalograms for patients with CP who had not undergone palatal repair until the age of 6 years in Japan. Furthermore, since previous studies indicated the differences in pharyngeal form between infants and young children due to variations in the size of the adenoids and maxillary growth [14], we used agematched the subjects that took part in the cephalometric analyses. Despite these limitations, the present study described the mechanism responsible for a poor speech prognosis in SMCP patients and provided a possible morphological marker for predicting postoperative VP closure in SMCP patients.
Conclusions
The velopharyngeal forms of the SMCP group were characterized by a shorter velum, a deeper and higher pharynx, and a more posterior PPW than the motion vector of palatal muscles. A positional discrepancy of the velopharynx including the PPW position relating to the direction of the motion of the velopharyngeal muscles may influence the difficulty of VP closure achievement in SMCP patients.
References
- Roux JP (1825) Memoir sur la staphylorrapie, ou suture de voile du voile du palais. JS Chaude, Paris.
- Kelly AB (1910) Congenital insufficiency of the palate. J Laryngo Rhino Oto 25: 281-300.
- CALNAN J (1954) Submucous cleft palate.Br J PlastSurg 6: 264-282.
- McWilliams BJ (1991) Submucous clefts of the palate: how likely are they to be symptomatic?Cleft Palate Craniofac J 28: 247-249.
- Oji T, Sakamoto Y, Ogata H, Tamada I, Kishi K (2013) A 25-year review of cases with submucous cleft palate.Int J PediatrOtorhinolaryngol 77: 1183-1185.
- Gosain AK, Hettinger PC (2009) Submucous cleft Palate, Part III Primary Cleft Lip and Palate Repair: Comprehensive Cleft Care. The McGraw-Hill Companies Inc, New York.
- Gilleard O, Sell D, Ghanem AM, Tavsanoglu Y, Birch M, et al. (2014) Submucous cleft palate: a systematic review of surgical management based on perceptual and instrumental analysis.Cleft Palate Craniofac J 51: 686-695.
- Sullivan SR, Vasudavan S, Marrianan E, Mullijen JB (2011) Submucous cleft palate and velopharyngeal insufficiency: Comparison of speech outcomes using three operative techniques by one surgeon. Cleft Palate-Craniofacial J 48: 561-570.
- Fujita Y, Abe Y, Miura E, Moriya Y, Ohmura T, et al. (1980) Follow-up study on 28 cases of submucous cleft palate (in Japanese). Jpn J Oral Surgery 26: 1250-1256.
- Harita Y, Isshiki N (1990) Comparison of submucous cleft palate and congenital velopharyngeal incompetence (in Japanese with English abstract). PracticaOto-Rhino-Laryngologica 83: 639-658.
- Chen PK, Wu J, Hung KF, Chen YR, Noordhoff MS (1996) Surgical correction of submucous cleft palate with Furlowpalatoplasty.PlastReconstrSurg 97: 1136-1146.
- Sommerlad BC, Fenn C, Harland K, Sell D, Birch MJ, et al. (2004) Submucous cleft palate: a grading system and review of 40 consecutive submucous cleft palate repairs.Cleft Palate Craniofac J 41: 114-123.
- Kaplan EN (1975) The occult submucous cleft palate.Cleft Palate J 12: 356-368.
- Peterson-Falsone SJ, Hardin-Hones MA, Karnell MP (2010) Noncleftvelopharyngeal problems, Session III Diagonosing and Managing Communication Disorders: Cleft Palate Speech Fourth Edition. Mosby Inc and Elsevier Inc, St Louis.
- Kuehn DP, Perry JL (2009) Anatomy and physiology of the velopharynx. Part V Cleft palate speech and management of velopharyngeal dysfunction: Comprehensive Cleft Care. The McGraw-Hill Companies Inc, New York.
- PODVINEC S (1952) The physiology and pathology of the soft palate.J LaryngolOtol 66: 452-461.
- Nakamura N, Ogata Y, Kunimitsu K, Suzuki A, Sasaguri M, et al. (2003) Velopharyngeal morphology of patients with persistent velopharyngeal incompetence following repushback surgery for cleft palate.Cleft Palate Craniofac J 40: 612-617.
- Oyama K, Nishihara K, Matunaga K, Miura N, Kibe T, et al (2016) Perceptual-speech, nasometoric and cephalometric results after modified V-Y palatoplasties with or without mucosal graft. Cleft Palate-Craniofac J 53: E-published ahead of print.
- Weatherley-White RC, Sakura CY Jr, Brenner LD, Stewart JM, Ott JE (1972) Submucous cleft palate. Its incidence, natural history, and indications for treatment.PlastReconstrSurg 49: 297-304.
- Braithwaite F (1963) Cleft palate repair: Modern Trends in Plastic Surgery. Butterworths, London.
- Wada T, Satoh K, Tachimura T, Tatsuta U (1997) Comparison of nasopharyngeal growth between patients with clefts and noncleft controls.Cleft Palate Craniofac J 34: 405-409.
Relevant Topics
- Stuttering therapy
- Active listening
- Aphasia
- Articulation disorders:
- Autism Speech Therapy
- Bilingual Speech pathology
- Clinical Linguistics
- Communicate Speech pathology
- Interventional Speech Therapy
- Late talkers
- Medical Speech pathology
- Spectrum Pathology
- Speech and Language Disorders
- Speech and Language pathology
- Speech Impediment / speech disorder
- Speech pathology
- Speech Therapy
- Speech Therapy Exercise
- Speech Therapy for Adults
- Speech Therapy for Children
- Speech Therapy Materials
Recommended Journals
Article Tools
Article Usage
- Total views: 12576
- [From(publication date):
October-2016 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 11794
- PDF downloads : 782