Case Report Open Access
Cemento-Ossifying Fibroma- A Case Report
Ugrappa Sridevi*, Ajay Jain, Neeraja Turagam and Mudrakola Durga PrasadAIMST Dental Institute, AIMST University, Semeling, Bedong, Kedah, Malaysia
- *Corresponding Author:
- Ugrappa Sridevi
Faculty of Dentistry, AIMST Dental Institute; AIMST University
Semeling, Bedong, Kedah, Malaysia
Tel: +60109454204
Email: srideviugrappa@gmail.com
Received date: June 08, 2016; Accepted date: June 25, 2016; Published date: July 04, 2016
Citation: Sridevi U, Jain A, Turagam N, Prasad MD (2016) Cemento-Ossifying Fibroma: A Case Report. Adv Cancer Prev 1:111. doi:10.4172/2472-0429.1000111
Copyright: © 2016 Sridevi U et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Advances in Cancer Prevention
Abstract
Background: Cemento-Ossifying Fibroma (COF) is considered by most as relatively rare, benign, non-odontogenic neoplasm of the jaw bones and other craniofacial bones characterized by replacement of normal bone by fibrous tissue and varying amounts of newly formed bone or cementum-like material, or both. It commonly affects, adults between the third and fourth decade of life and often shows variations in clinical, radiographic, and histopathologic features, hence require different treatment options.
Purpose: This paper attempts to diagnose a case of cemento-ossifying fibroma of the jaw not only based on clinical characteristics but also radiographic and histopathologic features as an adjunct.
Case: The patient was diagnosed with cemento-ossifying fibroma, presenting its clinical presentation, diagnostic imaging and histopathology features, as well as its surgical treatment.
Conclusion: The diagnosis of cemento-ossifying fibroma of the jaw can be established based on clinical, radiographic and histo-pathological features. It is a benign growth, considered to originate from the periodontal ligament and presents as a slow-growing lesion, but may cause deformity if left untreated. However, these tumors may exhibit variations in their neoplastic behaviours. It is often encapsulated and predominantly located in the mandible, and the definitive diagnosis of these lesions requires integration of its clinical, radiological and histological features. We present a case of cemento-ossifying fibroma in relation to the lower left one-third of the face, and its management.
Keywords
Cemento-ossifying fibroma; Benign odontogenic tumour; Fibro-osseous lesions
Introduction
Fibro-osseous lesions are a heterogeneous group of benign lesions of unknown aetiology affecting the jaws and other craniofacial bones, which are characterized by the replacement of normal bone by fibrous tissue, which contains a newly formed, mineralized product [1]. Over the last several decades, fibro-osseous lesions have evolved which includes two major entities: fibrous dysplasia and ossifying fibroma, as well as the other less common lesions such as florid osseous dysplasia, periapical dysplasia and focal sclerosing-osteomyelitis [2]. Cementoossifying fibroma is considered by most as relatively rare, benign, nonodontogenic neoplasm of the jaw bone. With female predilection over men (5:1), it is most frequently seen in third and fourth decades of life. The most common location is in premolar-molar region of the mandible, with 62% to 89% of patients, 77% occurring in the premolar and 75 to 89% in molar region and in maxilla, 11%-26% of cases [3]. Clinically, these tumours manifest as a slow-growing intra-bony asymptomatic mass, over a period of time lesion may become large enough to cause facial asymmetry. Radiologically, cemento-ossifying fibroma shows a number of patterns depending on the degree of maturation of the lesion. Histologically, these tumours are composed of well vascularized fibrocellular tissue with the capacity to form immature bone trabeculae and cementoid formations, though these findings are not specific of the lesion and can also be seen in fibrous dysplasia. A definitive diagnosis therefore requires correlation of the clinical, radiological and histological findings [4].
Case Report
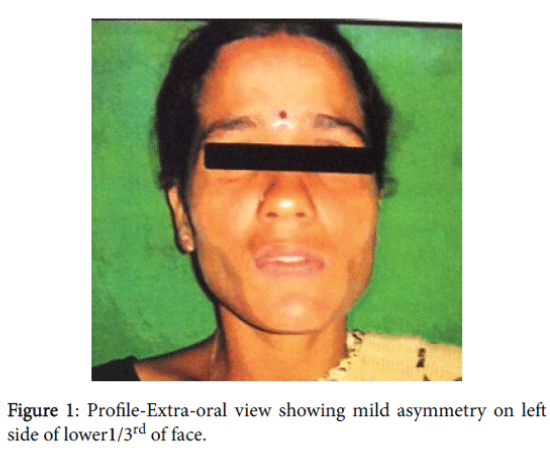
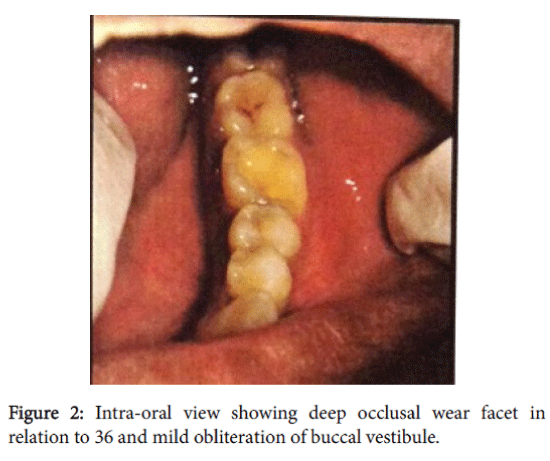
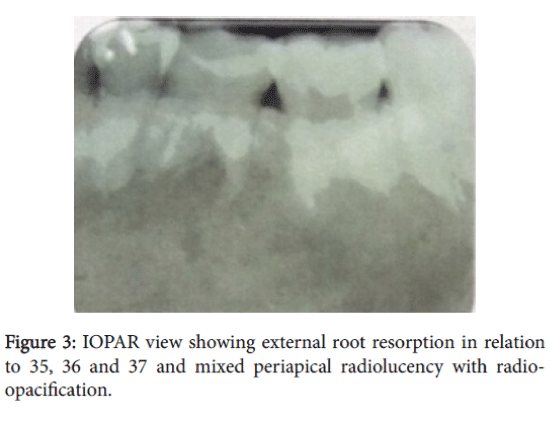
A 27 years old female patient reported to the outpatient department with a chief complaint of pain in the lower left back tooth region since a week. She gave history of sudden onset, with lancinating type of pain which is severe in nature. Pain aggravates on chewing food, on taking any hot and cold fluids and relieves on its own after sometime. Pain is associated with mild swelling which she noticed 15 days back and there was no increasing in size since then and not associated with any discharge, trauma or paraesthesia. On extra-oral examination, a diffuse swelling is seen in the lower 1/3rd of face on left side extending from angle of mandible to approximately 2 cm in front of it, in anteroposterior direction and inferio-superiorly from inferior border of mandible to 1 cm above it with no signs of neither discharge, bleeding nor visible pulsations (Figure 1). On palpation, soft to firm in consistency with no signs of tender, crepitus and non-fluctuant. A single left submandibular lymph node, mobile, non-tender, firm, measuring approximately about 0.5×0.5 mm in size is palpable. On intraoral examination, a deep occlusal wear facet is seen in relation to 36 which was non tender on percussion (Figure 2). A diffuse swelling is seen in the lower left buccal vestibule extending from distal of 35 to mesial of 37 and superior-inferiorly from attached gingiva of 36 to depth of vestibule measuring approximately about 1×0.5 cm in size and on palpation, firm, non-tender, no crepitus, no discharge and no pulsations are felt. Needle aspiration was negative. Based on the patient's history and clinical findings, the case was provisionally diagnosed as benign odontogenic tumour in relation to lower left buccal vestibule of 36. Clinical differential diagnosis of radicular cyst ameloblastoma, odontogenic keratocyst, and odontogenic myxoma were considered. An Intra-Oral Periapical Radiograph (IOPAR) shows, well defined radiolucency involving enamel and dentin in relation to 36 with no abnormality in periodontal ligament space but apical root shows irregularities is seen in relation to 35 and 36 indicating external root resorption with diffuse radiolucency interspersed radiopaque foci can be appreciated at the periapical region of 35 and 36 (Figure 3).
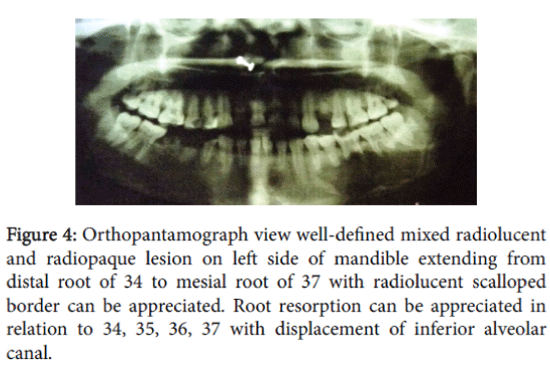
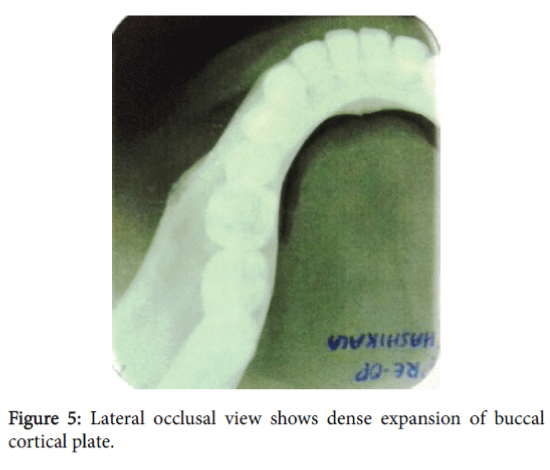
Panoramic radiograph shows a well-defined mixed radiolucent and radiopaque lesion on left side of mandible extending from distal root of 34 to mesial root of 37 with radiolucent scalloped border without any cortication is seen. Root resorption can be appreciated with respect to 34, 35, 36, 37 and inferior alveolar canal has been pushed inferiorly (Figure 4). A lateral occlusal mandibular radiograph shows mild buccal cortical plate expansion with respect to 36 and 37 (Figure 5).
Figure 4: Orthopantamograph view well-defined mixed radiolucent and radiopaque lesion on left side of mandible extending from distal root of 34 to mesial root of 37 with radiolucent scalloped border can be appreciated. Root resorption can be appreciated in relation to 34, 35, 36, 37 with displacement of inferior alveolar canal.
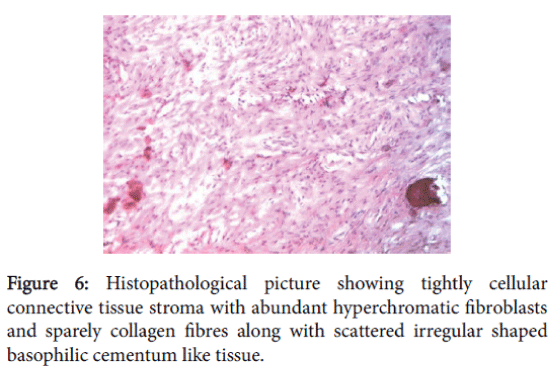
An incisional biopsy was performed, histological examination revealed as tightly cellular connective tissue stroma with abundant spindle shaped hyperchromatic fibroblasts and sparely collagen fibres along with scattered numerous irregular shaped basophilic cementum like tissue. Along with this, bone like tissue is also evident in the form of irregular trabeculae with osteocytes in lacunae (Figure 6).
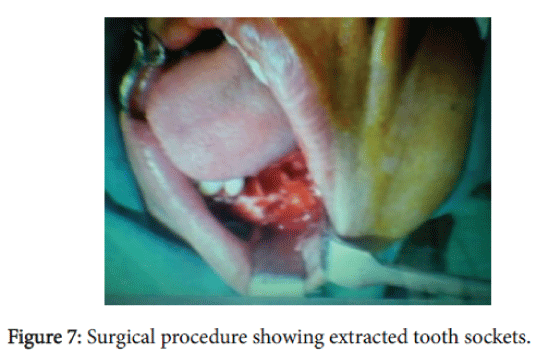
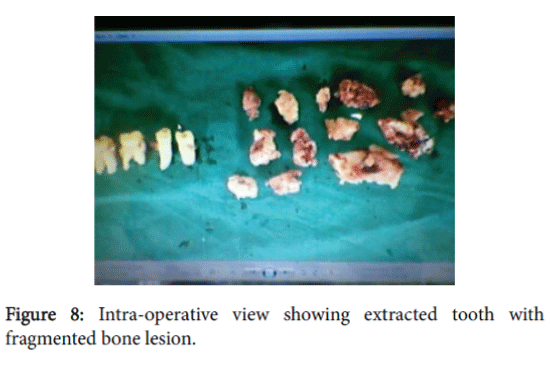
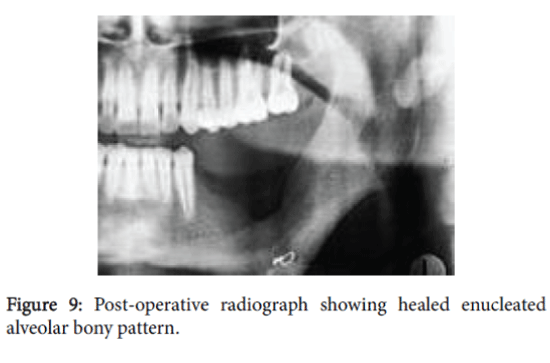
Periphery shows few blood vessels and numerous extravasated red blood cells. Based on radiological and histological findings, case was diagnosed as central cemento-ossifying fibroma. Complete surgical removal of the lesion was done (Figures 7 and 8) and patient was reviewed after 4 months (Figure 9).
Discussion
Fibro-osseous lesions of the jaws have been classified by Waldron and Kramer et al. [1]. These benign fibro-osseous lesions can arise from any part of the facial skeleton and skull with over 70% of cases arising in the head and the neck region and principally in the jaws [5]. Various classifications were proposed to classify these lesions, Menzel [6] gave the first description of a variant of ossifying fibroma, which was a benign fibro-osseous neoplasm, calling it as a cemento-ossifying fibroma in 1872. Larger lesions with size over 80 mm in their greatest diameter have been termed as giant ossifying fibroma [7]. The recent WHO (2005) edition of the classification of odontogenic neoplasms has replaced the term Cemento-ossifying fibroma with Ossifying Fibroma [8]. The origin of cemento-ossifying fibroma is not clearly understood, in most of cases reported in literature have found to have history of trauma which is not seen in our case. Few authors have considered that these lesions arose either by reactive or developmental origin, from the periodontal membrane which contains multi-potential cells, that under certain pathologic conditions, are capable of producing tumours which are composed of cementum, lamellar bone or fibrous tissue [9]. Based on their pathogenesis, Waldron, in 1985, subclassified cemento-ossifying fibroma as medullary or periodontal ligamentous in origin [1]. A more aggressive form of COF which occurs in younger individuals has been designated as Juvenile cemento-ossifying fibroma [10]. The recommended treatment for COF is complete excision of the tumour. The entire tumour should be removed along with the involved site. They are insensitive to radiotherapy and recurrences are uncommon. In the literature, recurrence has been reported in as many as 28% of patients with mandibular lesions [11]. The aetiology for such type of cases may be because of history of trauma [12] as it acts a possible triggering factor, postulating the lesion to be a connective tissue reaction rather than a genuine neoplasm [13]. An interdisciplinary approach is required [14] to diagnose a COF from clinical, radiographic and microscopic features. A study of 43 cases of ossifying fibromas presented by Eversole and collegues in 1985 found about 6 radiological variations among which, 9% of cases showed features of radiolucency with radiopaque dense foci, ground glass opacification along with root divergent or resorption, as these features can also been seen in our case [15]. These tumours may exhibit variations in their neoplastic behaviour, it is therefore, important to take into account the individual tumour behaviour when one is planning a proper surgical treatment, in order to eliminate the tumour completely and avoid tumour recurrence and at the same time improve the patient’s cosmetic and functional problems. The present case shows all the features related to cement-ossifying fibroma whose aetiology is of unknown origin and added one more incidence of COF and will be helpful in the literature.
References
- Waldron CA (1985) Fibro-osseous lesions of the jaws. J Oral MaxillofacSurg 43: 249-262.
- Liu Y, Wang H, You M, Yang Z, Miao J, et al. (2010) Ossifying fibromas of the jaw bone: 20 cases. DentomaxillofacRadiol 39: 57-63.
- Eversole LR, Leider AS, Nelson K (1985) Ossifying fibroma: a clinicopathologic study of sixty-four cases. Oral Surg Oral Med Oral Pathol 60: 505-511.
- Granizo RM, Cuellar AS, Falahat F (2000) Cemento-ossifying fibroma of the upper gingivae. Otolaryngol Head Neck Surg 122: 775.
- Kramer IR, Pindborg JJ, Shear M (1992) Histological typing of odontogenictumours. Berlin: Springer-Verlagpp: 27-33
- Mitrani M, Remsen K, Lawson W, Biller HF (1988) Giant ossifying fibroma of the paranasal sinuses. Ear Nose Throat J 67: 186-192.
- Khanna JN, Andrade NN (1992) Giant ossifying fibroma. Case report on a bimaxillary presentation. Int J Oral MaxillofacSurg 21: 233-235.
- Jankowski DSM (2009) Ossifying fibroma: a systematic review. DentomaxillofacRadiol 38: 495-513.
- Sarwar HG, Jindal MK, Ahmad SS (2008) Cemento-ossifying fibroma--a rare case. J Indian SocPedodPrev Dent 26: 128-131.
- Slootweg PJ, Panders AK, Koopmans R, Nikkels PG (1994) Juvenile ossifying fibroma. An analysis of 33 cases with emphasis on histopathological aspects. J Oral Pathol Med 23: 385-388.
- Sanchis JM, Peñarrocha M, Balaguer JM, Camacho F (2004) Cemento-ossifying mandibular fibroma: a presentation of two cases and review of the literature. Med Oral 9: 69-73.
- Ram R, Singhal A, Singhal P (2012) Cemento-ossifying fibroma. ContempClin Dent 3: 83-85.
- Feller L, Buskin A, Raubenheimer EJ (2004) Cemento-ossifying fibroma: case report and review of the literature. J IntAcadPeriodontol 6: 131-135.
- Kaushik SK, Haranal S, Naresh N (2015) Cemento-ossifying Fibroma of the Mandible: A Benign but Potentially Destructive Tumor. Oral MaxillofacPathol J 2015 6: 561-564
- Eversole LR, Merrell PW, Strub D (1985) Radiographic characteristics of central ossifying fibroma. Oral Surg Oral Med Oral Pathol 59: 522-527.
Relevant Topics
- 3D Mammograms
- Alternative Cancer Medicines
- Aromatase Inhibitors
- Breast Reconstruction Surgery
- Cancer and Nutrition
- Cancer Prevention from Nuts
- Cancer Screening
- Chemoprevention
- Dietary Supplements
- Exercise and Cancer
- Naturopathic Treatments
- Oncoplastic Surgery
- Scintimammography
- Stem Cell Transplants for Cancer Prevention
Recommended Journals
Article Tools
Article Usage
- Total views: 14409
- [From(publication date):
October-2016 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 13320
- PDF downloads : 1089