Case Study: Ectopic Molar Pregnancy-Is it an Iceberg Phenomenon?
Received: 25-Oct-2018 / Accepted Date: 12-Nov-2018 / Published Date: 19-Nov-2018 DOI: 10.4172/2161-0681.1000354
Keywords: Ectopic pregnancy; Tubal ectopic; Molar pregnancy; Partial mole; Trophoblastic disease
Introduction
Gestational trophoblastic disease is a spectrum of abnormal gestation and neoplasms arising from villous or extravillous trophoblast that are associated with pregnancy. They are the lesions of trophoblast with different proliferative capacities including nonneoplastic hydatidiform moles (complete mole, partial mole and invasive mole) and neoplastic conditions (gestational choriocarcinoma, placental site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor (ETT)).
Ectopic pregnancy is yet another common complication of pregnancy of which fallopian tube is the commonest site. The occurrence of both ectopic and molar pregnancy is a rare event. One of such rare cases is presented in this article.
Case History
A 23-year-old gravida 2, para 1, live 0 pregnant woman with 45 days of amenorrhea attended at Trichy SRM Medical College Hospital & Research Centre (Affiliated by Dr. MGR Medical University, Chennai), Trichy, Tamil Nadu, India with abdominal pain. Per vaginal examination revealed left forniceal fullness, but non-tender with normal sized uterus. On ultrasonography there was a 3 x 3 cm left adnexal mass with cardiac activity suggestive of left tubal ectopic pregnancy. Laparotomy revealed a unruptured left tubal ectopic pregnancy with a mass of size 2.5 x 2 cm seen in the ampullary region. No hemoperitoneum was noted. Left partial salpingectomy was done and sent for histopathological examination.
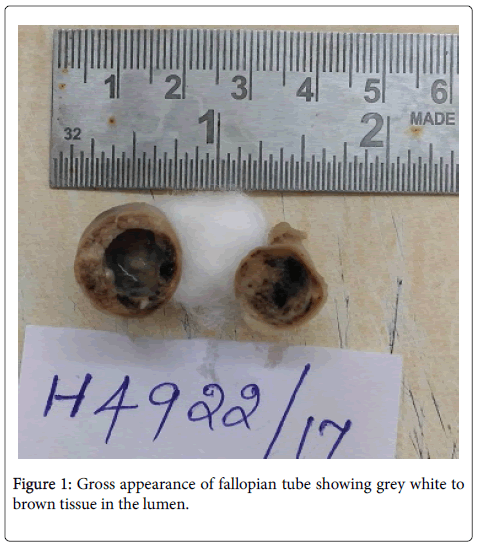
We received a portion of fallopian tube with fimbriae measuring 3.5 cm in diameter. External surface showed grossly enlarged tube with no signs of rupture. Cut surface showed dilated lumen filled with white to grey brown material (Figure 1).
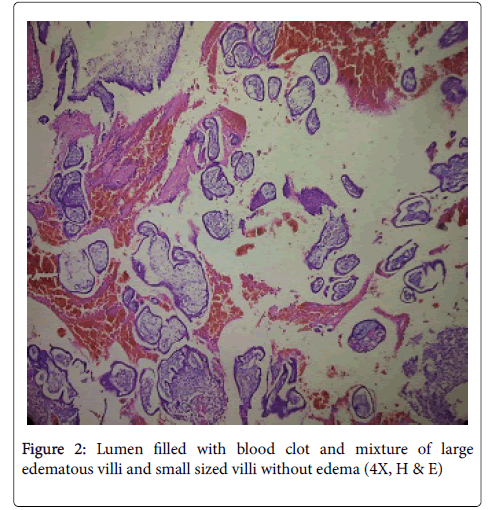
Microscopic examination showed thinned out fallopian tube wall with disrupted smooth muscle and chronic inflammatory infiltrate and congested blood vessels. Also seen occasional intact tubal plicae. Lumen was filled with blood clot and showed mixture of large edematous villi and small sized fibrotic villi (Figure 2).
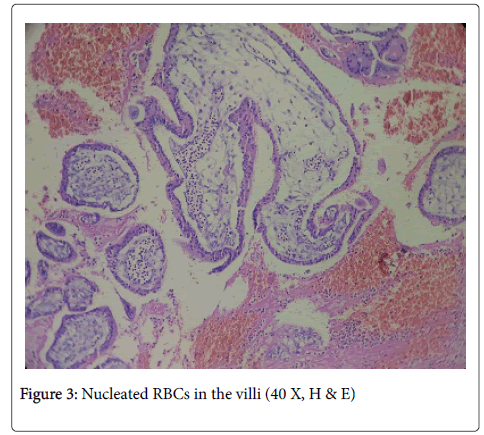
Some of the villi were irregular with scalloped outline and few had focal trophoblastic hyperplasia with mild atypia. Nucleated erythrocytes were seen in the lumen of few villi (Figure 3).
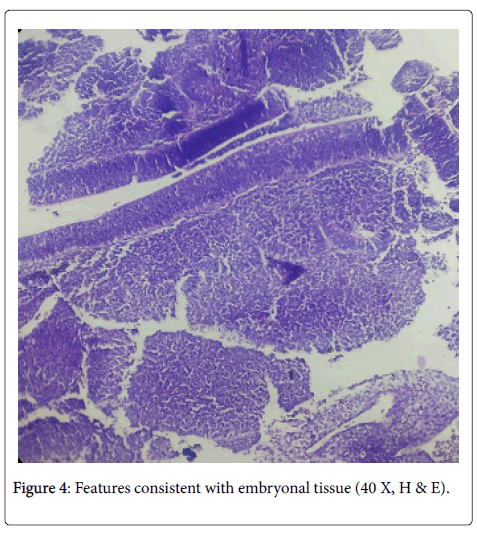
Embryonal tissue was also noted. The final diagnosis was given as partial hydatidiform mole in ectopic pregnancy of fallopian tube (Figure 4).
Discussion
Gestational trophoblastic disease is a disorder of reproductive age, though higher incidence is seen with age less than 20 and more than 40.
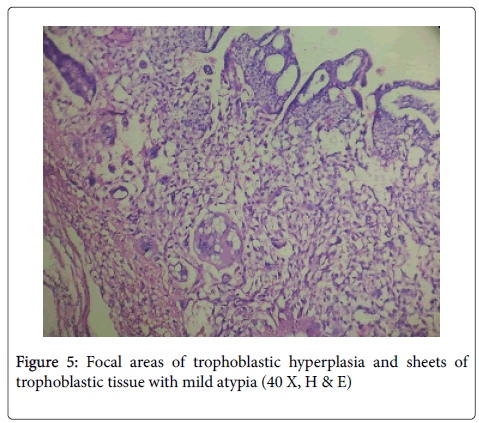
They are the abnormal placenta with trophoblastic hyperplasia, enlargement of chorionic villi with stromal edema (Figure 5).
In 1752, Smellie was the first to relate the terms “hydatid” and “mole” as “bunch of grapes of different sizes”. Hydatidiform moles are the nonneoplastic proliferations of the villous trophoblasts. The distinct subtypes are complete, partial hydatidiform moles and invasive moles. The major molecular mechanism is differential expression of the imprinted genes. At the genetic level, partial moles have typically diandric triploidy, most often arising from two sperms fertilizing an egg (XXY 58% or XXX 40% or XYY 2%) and rarely they are tetraploid. Complete moles on the other hand are most commonly diploid (46 XX) or tetraploid and are entirely paternally derived.
Risk factors for hydatidiform mole are extremes of maternal age (≤ 15 and ≥ 40 years old), previous history of molar pregnancies (0.5-2% risk of recurrence), ethinic variation and familial syndrome of recurrent complete hydatidiform mole (autosomal recessive inheritance) but it is extremely rare [1,2].
The incidence of molar pregnancy is 1 per 500 to 1000 pregnancies; the highest incidence is seen in South-East Asia with peak incidence of 13.0 in Indonesia, followed by Taiwan (8.0), Philippines and China (5.0) and Japan (3.8). The lowest incidence is seen in North America, Europe, and Oceania with rates ranging from 0.5–1.84/1,000 pregnancies [3].
Hydatidiform mole is a premalignant condition of gestational trophoblastic disease where 16% of complete hydatidiform mole and 0.5% of partial hydatidiform mole can undergo malignant transformation into invasive mole or choriocarcinoma.
Ectopic gestation is a rare pregnancy phenomenon with an incidence rate of 4.5-16.8/1000 pregnancies [3]. Tubal ectopic is the commonest with ampulla being the favourable site. Ectopic molar pregnancy is a rare condition, which can occur at any place in the pelvic cavity. The incidence of tubal ectopic molar pregnancy is very rare with 1.5 per 1,000,000 pregnancies. Molar changes can even be found in cornual and cervical pregnancies. β HCG values also do not provide supportive diagnosis as their levels are not much elevated as in case of uterine molar pregnancies. However need for correct diagnosis is more important as the complications, treatment modalities and follow up varies. Hence histopathological examination is the only confirmative test for this diagnosis [4,5].
Burton et al. had concluded that tubal molar pregnancy is very rare after studying different molar and ectopic pregnancies for a period of ten years and was usually over diagnosed [6]. Sebire et al. insisted that whenever there is florid extravillous trophoblastic hyperplasia in the products of conception, think of molar pregnancy. Histopathological examination of the products of conception is mandatory for all ectopic pregnancies and laproscopy is the main mode of treatment for all ectopic pregnancies [7].
Allen et al. described this entity as a rare event and suggested follow up till β HCG is zero. Histopathology is essential for diagnosis and DNA flow cytometry can be used as a complement for diagnosis [8]. Bousfiha et al. emphasized that molar pregnancy should be distinguished from nonmolar hydropic abortions as blighted ovum is common in ectopic gestations. In such cases, genotyping or chromosome in situ hybridization can be reliable. Further β HCG levels though elevated, are in the lower range as implantation is precluded by tubal implantation. Actually there is no difference in the levels for both tubal ectopic and tubal molar pregnancy [9].
Beena et al. recommended adequate monitoring of β HCG values to diagnose persistent ectopic pregnancy and also to rule out malignant trophoblastic disease. So the titres are monitored till they become undetectable [10].
Conclusion
Tubal molar pregnancy clinically mimics tubal ectopic pregnancy, hence it is difficult to diagnose. Though ultrasonography is good for diagnosing a tubal ectopic pregnancy, it has limited role in identifying the molar pregnancy and there is more chance of missing it. Moreover, clinical diagnosis of a molar pregnancy in an ectopic site is also more difficult. So histopathological examination of products of conception remains the current gold standard for diagnosis.
References
- Kurman, Robert J, Ellenson HL, Ronnett BM (2011) Blaustein's Pathology of the Female Genital Tract. New York: Springer.
- Hui P (2012) Gestational trophoblastic disease. Diagnostic and molecular genetic pathology. Current clinical pathology. New York: Springer.
- Borah T, Raphael V, Panda S, Saharia P (2010) Ectopic Molar Pregnancy: A Rare Entity. J Reprod Infertil 11: 201-203.
- Juan CW (2013) Fallopian tube invasive molar disease. Int J Gynaecol Obst 122: 161-162.
- Ikuma K, Okada I, Shiotani T, Shibahara H, Takemura T (1992) Invasive hydatidiform mole in the fallopian tube: report of a case. Nihon Sanka Fujinka Gakkai Zasshi 44: 1189-1192.
- J L Burton, E A Lidbury, A M Gillespie, Tidy JA, Smith O et al. (2001) Overdiagnosis of hydatidiform mole in early tubal ectopic pregnancy. Histopathology 38: 409-417.
- Sebire NJ, Lindsay I, Fisher RA, Savage P, Seckl MJ (2005) Overdiagnosis of complete and partial hydatidiform mole in tubal ectopic pregnancies. Int J Gynecol Pathol 24: 260-264.
- Allen L, Dawson C, Nascu P, Rous T (2016) A Molar Pregnancy within the Fallopian Tube. Case Reports in Obstetrics and Gynecology 2016: 1-3.
- Bousfiha N, Erarhay S, Louba A, Saadi H, Bouchikhi C, et al. (2012) Ectopic molar pregnancy: a case report. Pan Afr Med J 11: 63.
- Beena D, Teerthanath S, Jose V, Shetty J (2016) Molar Pregnancy Presents as Tubal Ectopic Pregnancy: A Rare Case Report. J Clin Diagn Res 10: ED10-ED11.
Citation: Pawar JG, Suganya R, Pawar GS, Rajajeyakumar M (2018) Case Study: Ectopic Molar Pregnancy-Is it an Iceberg Phenomenon?. J Clin Exp Pathol 8: 354. DOI: 10.4172/2161-0681.1000354
Copyright: © 2018 Pawar JG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4367
- [From(publication date): 0-2018 - Feb 26, 2025]
- Breakdown by view type
- HTML page views: 3671
- PDF downloads: 696