Case Study: An Uncommon Case of Bilateral Superior Semicircular Canal Dehiscence Associated with Sudden Sensoryneural Hearing Loss
Received: 02-Dec-2018 / Accepted Date: 28-Dec-2018 / Published Date: 04-Jan-2019 DOI: 10.4172/2161-119X.1000359
Abstract
Superior Canal Dehiscence (SCD) is a rare condition described for the first time by Minor in 1998. Bilateral superior canal dehiscence is even less frequent (0.6% of all SCD).
We present the case of a patient with bilateral superior canal dehiscence associated with sudden sensorineural hearing loss on one ear. The diagnosis of SCD was based on the symptoms of the patient (intolerance to loud noises, disequilibrium, hearing loss), based on the CT scan that revealed the bilateral dehiscence and based on the audiogram and the VEMP (Vestibular Evoked Myogenic Potential) testing with low cVEMP threshold bilaterally. All the data gathered were consistent with the diagnosis we made.
The particularity of the case consists in the fact that although the patient diagnosis was made according to all diagnostic criteria available and the CT scan and VEMP testing showed bilateral dehiscence, the symptoms were installed acutely and were evident only for one ear. In our opinion this can be explained by the fact that the patient had a more extended dehiscence in the left ear and also suffered a concomitant Sudden Sensorineural Hearing Loss (SSHL) that required additional testing making possible the correct diagnosis of the condition.
Keywords: Superior Canal Dehiscence (SCD); Vestibular Evoked Myogenic Potentials (VEMP); Sudden Sensorineural Hearing Loss (SSHL)
Introduction
In the beginning of the twentieth century Pietro Tullio was the first to describe a phenomenon of sensibility to loud sounds in pigeons with fenestration of the SC [1].
In 1998 Minor et al. draw the attention on a disease produced by a dehiscence on the superior semicircular canal thus creating a third window in the labyrinth [2]. This author was the first one who used this term for the diagnosis of the patients with symptoms such as hearing loss, vertigo and nystagmus induced by pressure and loud noises and also chronic disequilibrium.
The existence of the third window in the bony labyrinth explains the pathophysiology of the disease [3]. This window dissipates the energy of the sound wave permitting the fluid pressure to divert into the vestibular portion of the inner ear. Another result of this dehiscence is the lowered sensitivity to air conducted stimuli coexisting with an increased sensitivity to bone conducted stimuli. This is the result of the incoordination in the normal impedance relationship between the oval and the round window. Another characteristic of the disease is the fact that the stapedian reflex is not influenced. The result is a conductive hearing loss associated with a presence of the stapedian reflex [4].
The vestibular symptoms are explained by the modified flow of the endolymph in the superior canal produced by this additional window. Concerning the etiology, the superior canal dehiscence is thought to be caused by congenital malformations [5], head trauma [6] and increased intracranial pressure. Some authors suggest that the pulsations of the brain might have a role in the formation of the dehiscence.
Imagistic studies revealed a 5/1000 prevalence of SCD and a thinning (less than 0.1 mm) in 14/1000 cases. Other authors found a prevalence of 9% in a study on a consecutive series of temporal bone CT (Computerized Tomography) scans [7].
The size of the dehiscence seems to be related to symptoms, the larger the dehiscence the greater the symptoms.
The main signs and symptoms produced by the superior canal dehiscence are vertigo, disequilibrium, oscillopsia related to sound. The audiologic signs and symptoms are aural fullness, autophony, amplified body noises and hearing loss with low frequency air-bone gap, with normal immittance. The vestibular signs and symptoms are Tullio phenomenon, oscillopsia, chronic disequilibrium, positional vertigo, head tilt in response to sound [8,9].
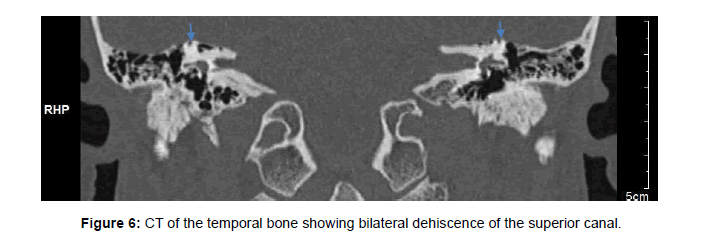
The diagnose of SCD is based on history, audiologic and vestibular testing but the the “gold standard” is the CT scan showing the absence of the bone that separates the superior semicircular canal from the floor of the middle cranial fossa.
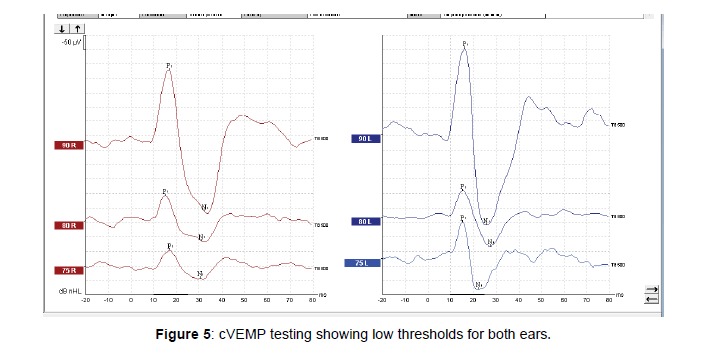
VEMP tests can be used to assess the presence of superior semicircular canal dehiscence [10,11]. These tests are able to detect whether a dehiscence is causing pathological pressure propagation in the vestibular labyrinth. The SDC produces larger amplitude VEMP waves and decrease the threshold used to elicit the specific waves [12,13]. Average cVEMP threshold using air conduction tone burst of 500 Hz in a normal ear is around 85-98 nHL while average cVEMP threshold in an SCD ear is between 61-81 dB nHL.
SCD is a great otologic mimicker, it might be confused with eustachian tube dysfunction, perylimphatic fistula, otosclerosis, Meniere’s disease.
Ward et al. [9] proposed diagnostic criteria for SCD (Table 1). Patients should meet the following conditions:
| 1. High-resolution computed tomography images (≤ 0.625-mm slice thickness) reformatted in the plane of the superior SCC (Squamous Cell Carcinoma) demonstrating a dehiscence |
| 2. At least one of the following symptoms consistent with SCDS |
| A. Bone conduction hyperacusis (in the form of autophony, audible eye movements, audible footsteps, etc.) |
| B. Sound-induced vertigo |
| C. Pressure-induced vertigo (via nasal or glottic Valsalva or pressure applied to the external auditory canal) |
| D. Pulsatile tinnitus |
| 3. At least one of the following diagnostic tests indicating a third mobile window |
| A. Negative bone conduction thresholds on pure tone audiometry |
| B. Enhanced VEMP responses (low cervical VEMP thresholds or high ocular VEMP amplitudes) |
| C. Elevated summating potential to action potential ratio on electrocochleography in the absence of a sensorineural hearing loss |
Table 1: Diagnostic criteria for SCD.
The treatment of SCD may either be conservative or a surgical, the latter consisting in plugging the canal or resurfacing, but there are also described round window procedures [14-16].
From 1998 until now, over 600 cases of SCD have been reported [9]. Bilateral SCD is even less frequent, 0.6% according to some authors.
Case Study
We present the case of a 41 years old male examined in our hospital accusing hearing loss on the left ear. The hearing loss was installed 24 hours before the consultation and the patient also reported that prior to the event he experienced a minor head trauma in the context of alcohol intake. No other relevant data were considered relevant from his medical history. The tympanic membrane had a normal appearance.
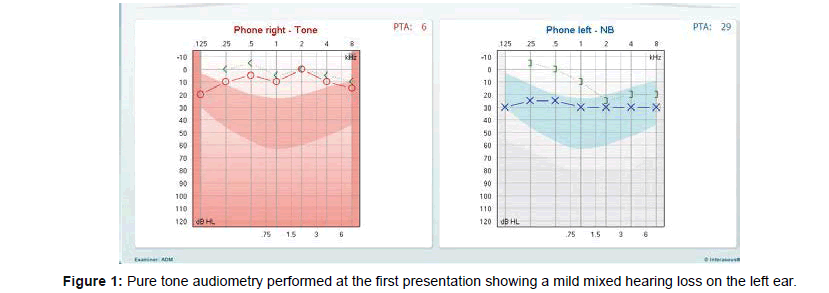
The audiogram performed at admission showed a mixed type of hearing loss with lowered thresholds at the left ear involving mainly the low frequencies that did not exceed 30 dB with only a minor conductive component (Figure 1).
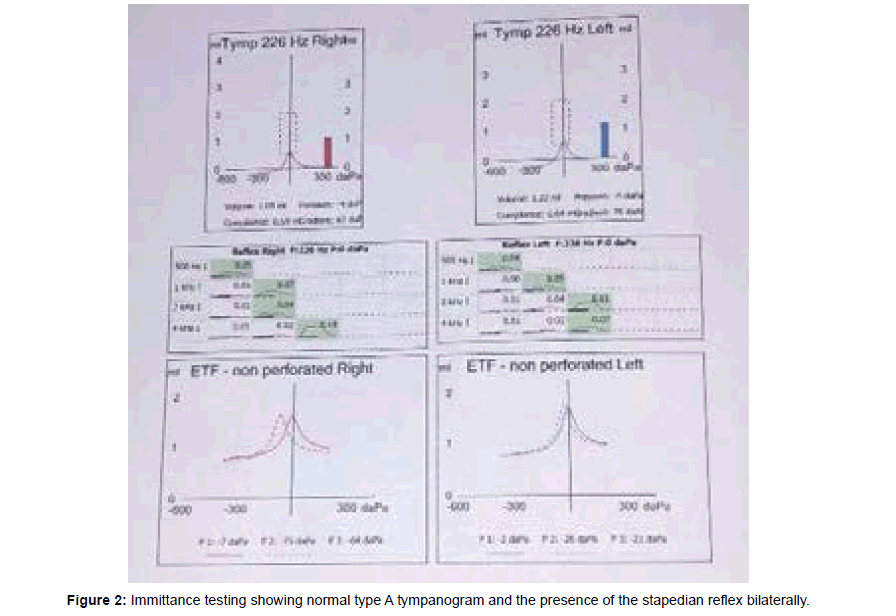
The tympanogram was a type A, the stapedian reflex was present in both ears (Figure 2). We must note the fact that the patient had no vertigo or dizziness during the impedance testing.
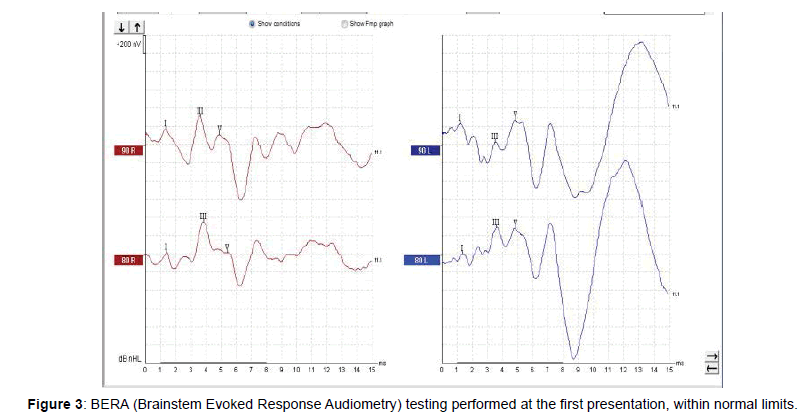
The brainstem evoked response audiometry we performed was within normal limits (Figure 3). Otoaccoustic emissions were present in both ears. The IRM (Interference Reflection Microscopy) imaging performed in that period showed no pathologic modifications.
The data gathered were interpreted as a mild sudden sensorineural hearing loss on account of the normal timpanogram with the intact stapedian reflex (although we could not explain the conductive component in the audiogram) and treated accordingly. The patient received medical therapy with corticosteroids and vasoactive substances for a period of 10 days. The evolution was good but the hearing on the left ear did not totally recover. We recommended hyperbaric oxygen therapy. The patient could not pursue the therapy accusing intense pain in the left ear.
Two weeks afterwards we continued the treatment with local intratympanic corticotherapy using dexamethasone. Subsequently the hearing was almost totally restored. The patient was satisfied with the result. Three months after this event the patient came to the hospital accusing important hearing loss on the left ear and tinnitus. The hearing loss was installed suddenly two days prior to the admission, also after alcohol intake. The patient could not recall any recent head trauma. He noticed that loud noises were very annoying for him and that extremely loud noises made him lose equilibrium. He compared the sensations to small earthquakes he felt when exposed loud noises.
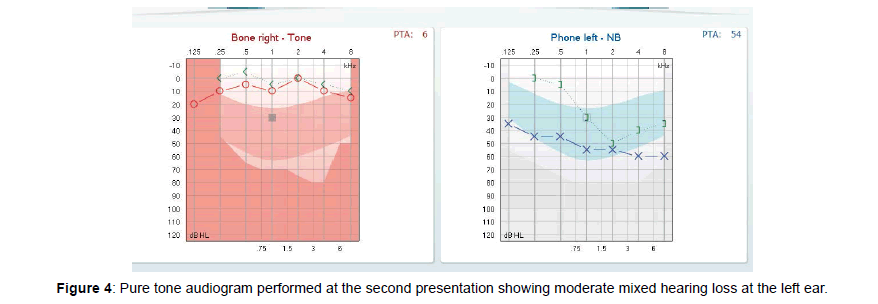
The audiogram we performed showed a moderate mixed hearing loss on the left ear (Figure 4). Weber test lateralized on the left ear. The result of the cVEMP test we performed was consistent with bilateral superior canal dehiscence, with extremely low cVEMP thresholds in both ears (Figure 5).
We tried to elicit the Tulio phenomenon by exposing the patient to loud noises but the VNG recording did not show any abnormal nystagmus. We ordered a CT of the temporal bone which highlighted important bilateral dehiscence of the superior canal 7-8 mm on the left ear and 4 mm on the right ear (Figure 6).
The patient did not accept surgery and opted for a conservative treatment. With the avoidance of all the increments of pressure in the middle ear or intracranial pressure, the vestibular symptoms disappeared but the hearing loss did not improve.
Discussion
Superior canal dehiscence seems to be a situation not so frequently encountered. In a study on 164 ears Masaki found a prevalence of asymptomatic SCD of 3% [17]. Bilateral SCD is even more rare with a prevalence of 0.6% among all SCD. The diagnosis of superior canal dehiscence cannot be established only based on the CT scan because of the false positive results (80% of cases).
The case we studied can be considered a rare case of bilateral SCD and it meets all the criteria proposed by Ward et al. but even so, there are some aspects we cannot totally explain. Starting by discussing the history of this case, the first thing we thought about is whether the minor head trauma had something to do with the symptoms the patient experienced. There is a possibility that this caused the fracture of a thin bone covering the superior canal. On the other hand the patient had no vestibular symptoms at the first presentation. Another question we had taken into consideration was if the alcohol intake had a role in producing the signs and symptoms of the disease but we could not find any connection. The fact that the patient could not continue the hyperbaric oxygen therapy due to left ear pain might also be an indicator that there was a bone dehiscence from the first presentation.
The history with the sensations of instability at loud noises and the hearing loss appeared at the second episode, conducted us to a probable diagnostic of SCD but the final diagnosis was established through CT scan. The VEMP testing was consistent with the CT findings showing high amplitude and low threshold for eliciting cVEMP for both ears. The finding that was unexpected was the SCD in both ears although only one ear had symptoms that were consistent with this diagnostic. The fact that the larger the dehiscence is in the left ear might offer an explanation.
We should remark the fact that the immittance testing showed type A tympanogram with present acoustic reflexes bilaterally, also a finding consistent with this diagnostic. But the Weber test lateralized to the left ear and the mixed hearing loss should have raised the suspicion that there is not a sensorineural hearing loss. In this aspect we should also emphasize the fact that the otoacoustic emissions were present in the beginning.
In the second episode the hearing loss was still of a mixed type but a lot more severe compared to the debut and it could not be accounted in our opinion only by the SCD. We also could not elicit and record at the VNG any nystagmus during stimulation with loud sounds and the posturography was normal.
There are other authors that also reported SCD with conductive hearing loss without vertigo [18]. We consider that the patient had an initially asymptomatic bilateral canal dehiscence and in addition he experienced a sudden sensorineural hearing loss on the left ear that drew attention to the disease. The hearing loss was evident only on one side but the dehiscence was bilateral. On the other hand, the cVEMP testing was consistent with the CT scan findings, showing lowered thresholds for both ears. This might be explained, on our opinion, by the fact that the dehiscence was bigger in the left side (7-8 mm). The concomitance with the SNSHL can be responsible for the course of this patient’s disease.
Conclusion
The diagnosis of SCD need to be based on a combination of typical symptoms, CT (Computerized Tomography) scan findings, clinical findings and laboratory testing (audiogram and VEMP testing).
The gold standard for diagnosis is still the CT scan but VEMP testing has an important role in determining whether the apparent dehiscence plays a role in the pathologic pressure transmission in the inner ear causing the symptoms.
Conservative treatment is an option that can be taken into account. Although it is not a frequent disease, we should always think at the possibility that a SCD can exist in symptomatic patients.
References
- Addams-Williams J, Wu K, Ray J (2014) The experiments behind the tullio phenomenon. J Laryngol Otol 128: 223-227.
- Minor LB, Solomon D, Zinreich JS, Zee DS (1998) Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol Head Neck Surg 124: 249-258.
- Rosowski JJ, Songer JE, Nakajima HH, Brinsko KM, Merchant SN (2004) Clinical, experimental and theoretical investigations of the effect of superior semicircular canal dehiscence on hearing mechanisms. Otol Neurotol 25: 323-332.
- Minor LB, Carey JP, Cremer PD, Lustig LR, Streubel SO, et al. (2003) Dehiscence of bone overlying the superior canal as a cause of apparent conductive hearing loss. Otol Neurotol 24: 270-278.
- Saxby A, Gowdy C, Fandiño M, Chadha NK, Kozak FK, et al. (2015) Radiological prevalence of superior and posterior semicircular canal dehiscence in children. Int J Pediatr Otorhinolaryngol 79: 411-418.
- Minor LB (2005) Clinical manifestations of superior semicircular canal dehiscence. Laryngoscope 115: 1717-1727.
- Williamson RA, Vrabec JT, Coker NJ, Sandlin M (2003) Coronal computed tomography prevalence of superior semicircular canal dehiscence. Otolaryngol Head Neck Surg 129: 481-489.
- Minor LB (2000) Superior canal dehiscence syndrome. Am J Otol 21: 9-19.
- Ward BK, Carey JP, Minor LB (2017) Superior canal dehiscence syndrome: Lessons from the first 20 years. Front Neurol 8: 177.
- Zuniga MG, Janky KL, Nguyen KD, Welgampola MS, Carey JP (2013) Ocular versus cervical VEMPs in the diagnosis of superior semicircular canal dehiscence syndrome. Otol Neurotol 34: 121-126.
- Niesten MEF, McKenna MJ, Herrmann BS, Grolman W, Lee DJ (2013) Utility of cVEMPs in bilateral superior canal dehiscence syndrome. Laryngoscope 123: 226-232.
- Watson SR, Halmagyi GM, Colebatch JG (2000) Vestibular hypersensitivity to sound (tullio phenomenon): Structural and functional assessment. Neurology 54: 722-728.
- Van Haesendonck G, Van de Heyning P, Van Rompaey V (2016) Retrospective cohort study on hearing outcome after transmastoid plugging in superior semicircular canal dehiscence syndrome: Our experience. Clin Otolaryngol 41: 601-606.
- Goddard JC, Wilkinson EP (2014) Outcomes following semicircular canal plugging. Otolaryngol Head Neck Surg 151: 478-483.
- Crovetto M, Areitio E, Elexpuru J, Aguayo F (2008) Transmastoid approach for resurfacing of superior semicircular canal dehiscence. Auris Nasus Larynx 35: 247-249.
- Silverstein H, Kartush JM, Parnes LS, Poe DS, Babu SC, et al. (2014) Round window reinforcement for superior semicircular canal dehiscence: A retrospective multi-center case series. Am J Otolaryngol 35: 286-293.
- Masaki Y (2011) The prevalence of superior canal dehiscence syndrome as assessed by temporal bone computed tomography imaging. Acta Otolaryngol 131: 258-262.
- Mikulec AA, McKenna MJ, Ramsey MJ, Rosowski JJ, Herrmann BS, et al. (2004) Superior semicircular canal dehiscence presenting as conductive hearing loss without vertigo. Otol Neurotol 25: 121-129.
Citation: Musat GC, Anghel AG, Musat O (2019) Case Study: An Uncommon Case of Bilateral Superior Semicircular Canal Dehiscence Associated with Sudden Sensoryneural Hearing Loss. Otolaryngol (Sunnyvale) 9:359. DOI: 10.4172/2161-119X.1000359
Copyright: © 2019 Musat GC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5066
- [From(publication date): 0-2019 - Oct 17, 2025]
- Breakdown by view type
- HTML page views: 4182
- PDF downloads: 884