Case Report of Huge Esthesioneuroblastoma
Received: 02-Jul-2016 / Accepted Date: 08-Aug-2016 / Published Date: 15-Aug-2016 DOI: 10.4172/2161-119X.1000256
Abstract
Esthesioneuroblastoma is a rare malignant tumor, account for only 1-5% of all malignant tumors of the paranasal sinuses; usually it presents with locally invasive disease, the delayed diagnosis of these tumors leads to tragic prognosis and bad results of surgery or conservative management. In this case, the diagnosis was too late in spite of followed up by medical doctors in deferent specialties; as a result it must be rules to avoid this problem like the mandatory of nasal endoscopy in all patients with nasal complaints (specially with refractory symptoms) and also radiologicinvestigations must be mandatory when epistaxis, nasal blockage, anosmia or headache does not respond to medical treatment.
Keywords: Esthesioneuroblastoma; Olfactory neuroblastoma; Epistaxis; CT; MRI
252671Introduction
Esthesioneuroblastoma is a rare malignant tumor, account for only 1–5% of all malignant tumors of the paranasal sinuses; usually it presents with locally invasive disease, the delayed diagnosis of these tumors leads to tragic prognosis and bad results of surgery or conservative management. In this case, the diagnosis was too late in spite of followed up by medical doctors in deferent specialties; as a result it must be rules to avoid this problem like the mandatory of nasal endoscopy in all patients with nasal complaints (specially with refractory symptoms) and also radiologic investigations must be mandatory when epistaxis, nasal blockage, anosmia or headache does not respond to medical treatment.
Case Report
Patient 50 year old, male came to ENT clinic with complaint of severe recurrent epistaxis 6 months ago, he underwent a lot of medications but without any improvement, recently he aggravated with right nasal obstruction, complete anosmia, right eyelids edema associated with epiphora, severe frontal headache unresponsive to pain killers and balance disorder without specific nervous signs.
By clinical examination there was huge mass filled completely right nasal cavity without any anatomical landmarks in the right nose. It was polypoid mass in shape, brown red color, soft fragile and associated with moderate bleeding when touch it. Examination of the left nasal cavity, mouth, ears, neck and cranial nerves were within normal limited.
Investigations
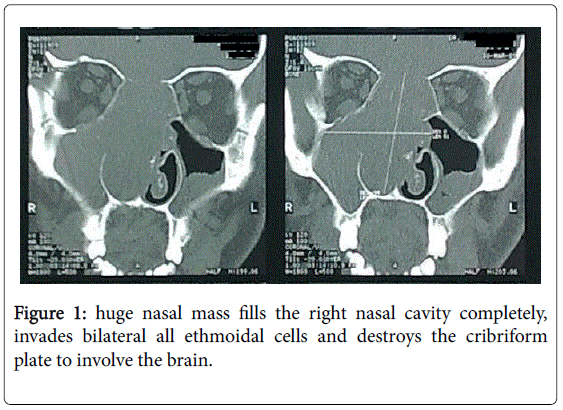
Computed tomography scan of paranasal sinuses done and it showed a huge nasal mass fills the right nasal cavity completely, invades bilateral all ethmoidal cells and destroys the cribriform plate to involve the brain (Figure 1).
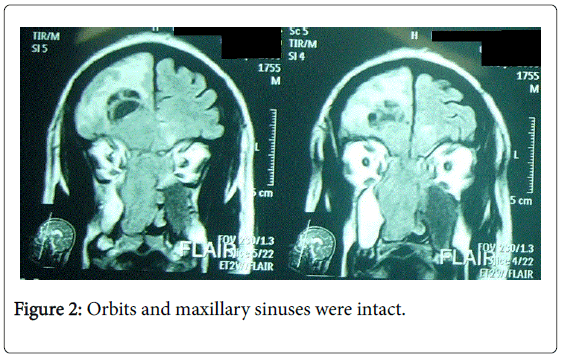
Magnetic resonance imaging of the head done and it showed that the mass invades frontal lobe of the brain, measures 4*5 cm in dimensions, push the midline of the brain to the left side, and associated with wide edema in right frontal lobe. Orbits and maxillary sinuses were intact (Figure 2).
Surgical biopsy
Small surgical biopsy from the nasal cavity was taken under local anesthesia and histopathology result was Olfactory Neuroblastoma (Esthesioneuroblastoma).
General considerations
Esthesioneuroblastoma, first described by Berger et al. in 1924, [1] is an uncommon neoplasm that arises from olfactory epithelium high in the nasal vault and frequently invades the skull base, cranial vault, and orbit. Although esthesioneuroblastoma accounts for up to 3% of intranasal neoplasms in some series, fewer than 400 unique cases have been reported in the world literature. The recent apparent increase in incidence is at least in part attributable to improvements in diagnostic imaging and pathologic recognition of this relatively rare entity. Because of the limited number of subjects treated in different eras of medical and surgical practice, in addition to nonuniform treatment schemes and follow-up, management recommendations regarding these tumors have been based largely on anecdotal data and limited series.
Pathology
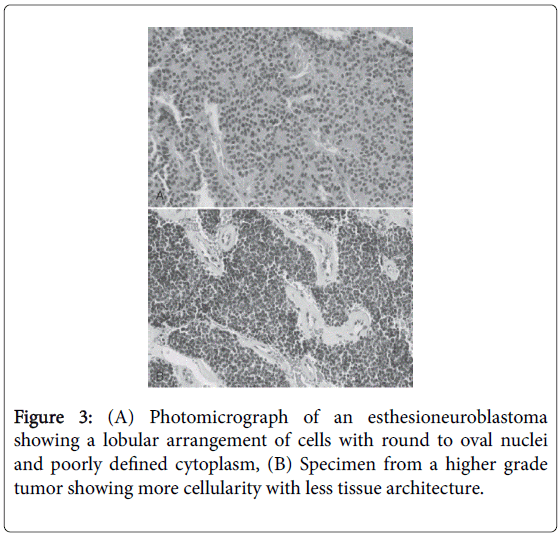
The morphologic, ultrastructural, and immunohistochemical features of esthesioneuroblastoma are similar to those of neuroblastoma of the adrenal glands and sympathetic nervous system. Light microscopy reveals a lobular architecture with sheets of cells in a dense neurofibrillary background. Individual cells have round to oval nuclei with scant, poorly defined cytoplasm. Occasionally, olfactory rosettes or pseudorosettes are present. A grading system based on histology has been proposed as a prognostic tool but has achieved varying success (Table 1 and Figure 3) [2].
| Grade | I | II | III | IV |
|---|---|---|---|---|
| Cytoarchitecture | Lobular | Lobular | +/- | +/- |
| Mitotic rate | 0 | Low | Moderate | High |
| Nuclear pleomorphism | Absent | Slight | Moderate | Marked |
| Rosettes | +/- | +/- | True rosettes | None |
| Necrosis | Absent | Absent | Mild | Extensive |
Table 1: Hyams’ Histologic Grading System for Esthesioneuroblastoma.
Ultrastructurally, dense membrane-bound neurosecretory granules are seen along with neurofilaments and microtubules. On immunohistochemical staining, most esthesioneuroblastomas are positive for neuron-specific enolase (NSE), neurofilament, synaptophysin, chromogranin, and Leu-7 and variably positive for S-100. Although similar to neuroblastoma histologically, correlated coexpression of NSE and cytokeratin points to an epithelial rather than neural crest origin of these tumors [3].
Staging
Several staging systems, including Hymans, Kadish, and TNM systems, have been proposed as a guide to choosing treatment modalities. Tumor staging is an important guide for prognosis and therapy.
Kadish et al. were the first to propose a staging classification for esthesioneuroblastoma (ENB) [4]. ENBs were divided into 3 categories: groups A, B, and C. Group A is limited to tumors of the nasal fossa; in group B, extension is to the paranasal sinuses; and group C is defined as extension beyond the paranasal sinuses and nasal cavity.
Some authors have noted that effectively stratifying patients with the Kadish system can be difficult. Recognizing these inadequacies, Morita et al. in 1993 published a revised Kadish system that redefined stage C (consisting of local disease spreading beyond the paranasal sinuses) and included a stage D (distant metastasis) [5].
In 1992, Dulguerov and Calceterra proposed a classification based on the tumor, node, metastasis (TNM) system, which is predicated on CT and MRI findings that can be identified before treatment [6]. Although this classification system has gained popularity, attempts have been made to further modify the Kadish system for ENB.
The TNM classification is as follows:
T1 - Tumor involving the nasal cavity and/or paranasal sinuses (excluding sphenoid), sparing the most superior ethmoidal cells
T2 - Tumor involving the nasal cavity and/or paranasal sinuses (including the sphenoid), with extension to or erosion of the cribriform plate
T3 - Tumor extending into the orbit or protruding into the anterior cranial fossa, without dural invasion
T4 - Tumor involving the brain
N0 - No cervical lymph node metastasis
N1 - Any form of cervical lymph node metastasis
M0 - No metastasis
M1 - Distant metastases present
In our case, pt. was in stage C regarding Kadish staging system and T4N0M0 in TNM classification. The patient was informed that the prognosis is unsecured, the treatment of choice is surgery to resolve or reduce the symptoms, the recurrence is possible, and postoperative radiotherapy is important to reduce the recurrence.
Operation
Surgery was performed in combined approaches: 1. Cranial approach (by Neurosurgeon) (Figure 4) and 2. Intranasal endoscopic sinus surgery (by ENT surgeon). The neurosurgery was performed by Bifrontal approach and removal of the cerebral component of tumor which was consisted of cystic and solid components with moderate vascularity and then pericranial flap was used to close the defect in the skull base.
Intranasal endoscopic sinus surgery performed and it was possible due to the tumor concentrated in the central part of the nasal cavity without erosion of bony structures of the maxillary sinus or orbits, the density in Rt. maxillary sinus was fluid density in MRI (not tumor tissue) and the lamina papyracea in both sides were intact.
The intranasal surgery done by removal of all nasal component of tumor by shaver and create one cavity between the orbits in the upper part of nasal cavity, detection and clean the skull base and tumor’s bed, contact with the pericranial flap which previously repaired by neurosurgeon, too thick mucus was sucked from the Rt. maxillary sinus and support defect’s closure in the skull base by muscular fascia and nasal packs.
Post-operation histopathology
Histopathology was done for cerebral component witch removed by an en-bloc resection technique and it measured 4.0*4.5 cm in size but the nasal component was removed by micro electric surgical Debrider, so no histopathology for nasal component.
Follow up
Patient underwent post-operative adjuvant radiotherapy, standard techniques include external megavoltage beam with 5500 cGy dose. Regular monthly follow up done until 8 months, and it was without any recurrence or complications. After that the follow up was not available.
Conclusion
Diagnosis in this case was too late – despite of the patient previously was seen and treated by several doctors from various specialties - as a result nasal endoscopy must be mandatory in all patients with nasal complaints (specially with unresponded cases). Epistaxis is not always benign symptom and may be it hides underlying disaster, so investigations must be mandatory when epistaxis does not respond to medical treatment. In this case there was history of exposure to Irradiated Uranium and Nuclear Weapons in the war, may be explain the etiology of this tumor, but there is no previous studies about that, may be this form a good idea for new studies and research.
References
- Berger L, Luc H, and Richard A (1924) L’esthesioneuroepitheliomeolfactif. Bull Assoc Franc Etude Cancer 13: 410-421.
- Hyams VJ (1988) Tumors of the upper respiratory tract and ear. In Hyams VJ, Batsakis JG, and Michaels L (eds): Atlas of Tumor Pathology, Second Series, Fascicle 25. Washington DC: Armed Forces Institute of Pathology 240-248
- Banerjee AK, Sharma BS, Vashishta RK (1992) Intracranial olfactory neuroblastoma: evidence for olfactory epithelial origin. J ClinPathol 45: 299-302.
- Kadish S, Goodman M, Wang CC (1976) Olfactory neuroblastoma. A clinical analysis of 17 cases. Cancer 37:1571-1576.
- Morita A, Ebersold MJ, Olsen KD, Foote RL, Lewis JE, et al. (1992)Esthesioneuroblastoma: prognosis and management. Neurosurgery 32:706-714.
- Dulguerov P, Calcaterra T (1992) Esthesioneuroblastomathe UCLA experience 1970-1990. Laryngoscope 102:843-849.
Citation: Fakoury MA (2016) Case Report of Huge Esthesioneuroblastoma. Otolaryngol (Sunnyvale) 6:256. DOI: 10.4172/2161-119X.1000256
Copyright: © 2016 Fakoury MA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11545
- [From(publication date): 8-2016 - Dec 20, 2024]
- Breakdown by view type
- HTML page views: 10730
- PDF downloads: 815