Case Report: High-Sensitivity C-Reactive Protein is a Potentially Useful Marker of the Need for Psychotic Treatment for Cognitive Dysfunction Related to Low-Grade Inflammation
Received: 08-Sep-2017 / Accepted Date: 17-Nov-2017 / Published Date: 24-Nov-2017 DOI: 10.4172/2161-0460.1000402
Abstract
We encountered a 79 year old female patient with mild cognitive impairment who showed sustained improvement to an almost normal level of global cognitive function for >1 year when treated with donepezil. Her levels of high-sensitivity C-reactive protein (hs-CRP) also showed a sustained decrease with treatment. Here, we describe the clinical changes in her cognition and discuss the relationship between cognitive function and low-grade inflammation, focusing on three important issues. First, cognitive dysfunction may be related to low-grade inflammation. Second, hs-CRP may be a suitable marker for this low-grade inflammation. Third, treatment with cholinesterase inhibitors was effective, either by suppressing this low-grade inflammation or by upregulating acetylcholine, which suppresses such inflammation. In this patient, inflammation appeared to be related to the cholinergic anti-inflammatory pathway.
Keywords: Acetylcholine; Cholinergic anti-inflammatory pathway; High sensitive C-reactive protein; Low grade inflammation; Pseudodementia
Abbreviations
ACh: Acetylcholine; AD: Alzheimer’s Disease; ChAT: Choline Acetyltransferase; ChEI: Cholinesterase Inhibitor; hs-CRP: High Sensitive C-Reactive Protein; MCI: Mild Cognitive Impairment; MMSE: Mini-Mental State Examination
Introduction
Neuropsychiatric disorders are thought to be related to hyperactivity of the inflammatory system [1,2] as well as low-grade inflammation [3,4]. However, to date there has not been an adequate tool for quantitatively measuring the relationships between inflammatory states and neuropsychiatric disorders, so this issue has not been evaluated objectively. We recently encountered a 79 year old female patient with mild cognitive impairment (MCI) who experienced improvement in global cognitive function after being treated with the cholinesterase inhibitor (ChEI) donepezil. Her cognitive state was maintained at almost normal levels for >1 year. Treatment also produced a sustained decrease in her levels of high-sensitivity C-reactive protein (hs-CRP).
In this article, we describe the clinical changes in the patient’s cognition, focusing on the relationship between the cognitive state in pseudodementia and low-grade inflammation. The patient herself and her proxy have provided written consent authorizing publication of this report.
Case Presentation
A 79 year old woman presented at our outpatient clinic complaining of forgetfulness, which she had first noticed 5 or 6 years earlier. She lived with her daughter, who reported that her mother had been forgetful for 3 years before coming to our clinic. For 10 years the patient, who had a subarachnoid hemorrhage 23 years earlier, had cared for her husband who had dementia. This caused her to experience sustained stress because her husband had been apathetic with little capacity for self-care, which placed a large burden on her. In addition, he had periodic episodes of extreme anger
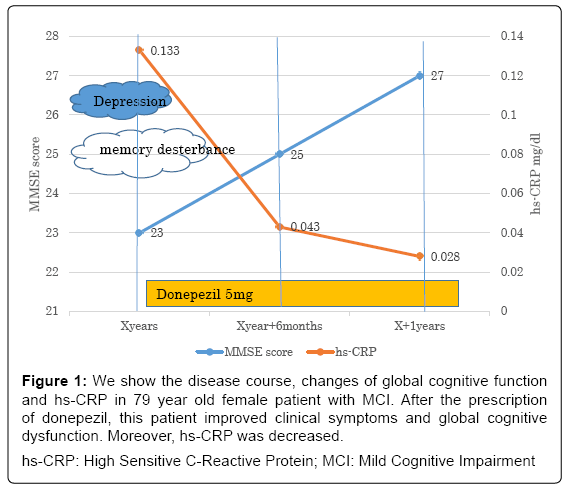
The patient’s Mini-Mental State Examination (MMSE) [5,6] score was 23, her CT findings showed no atrophy of the hippocampal region, and her hs-CRP was 0.133 mg/dl. We diagnosed MCI due to Alzheimer’s disease (AD) [7] and prescribed donepezil 5 mg/day. In Japan, 5 mg donepezil is approved for mild to moderate AD. At 6 months and 1 year of treatment, respectively, MMSE scores were 25 and 27 and her hs-CRP levels were 0.043 mg/dl and 0.028 mg/dl (Figure 1). In addition, both the patient and her daughter felt that the patient’s cognitive function was comparable with that of people of the same age with normal cognitive function.
Figure 1: We show the disease course, changes of global cognitive function and hs-CRP in 79 year old female patient with MCI. After the prescription of donepezil, this patient improved clinical symptoms and global cognitive dysfunction. Moreover, hs-CRP was decreased.
hs-CRP: High Sensitive C-Reactive Protein; MCI: Mild Cognitive Impairment
Discussion
We initially diagnosed MCI due to AD and prescribed the ChEI donepezil 5 mg/day, after which the patient’s cognitive dysfunction almost completely resolved. This result seems to indicate that her cognitive impairment as related to a disorder of the cholinergic system. Treatment with donepezil 5 mg/day improved the patient’s cognitive function to almost-normal levels, which were maintained for over 1 year; therefore we changed the diagnosis to pseudodementia due to depression, which we speculate was caused by excessive sustained stress. However, because depression is also considered a prodromal symptom of AD [8], it is challenging to distinguish depression from AD in the elderly, which makes an accurate diagnosis difficult. Therefore, we plan to follow this patient carefully.
Psychiatric disorders such as depression and AD have also been reported to be related to low-grade inflammation [9-11] and increased levels of hs-CRP [12,13]. However, there is no consensus on what degree of inflammation corresponds to low-grade inflammation. Krogh et al. [14] found a relationship between CRP levels and depression, reporting that hs-CRP was higher in depressed patients (range 0.6 to 2.6 mg/l) compared with normal controls (range 0.06 to 0.26 mg/dl). Based on his report and, when our patient presented with MCI (MMSE=23) due to depression and needed treatment, her hs-CRP level was 0.133 mg/ dl; when her cognitive function had resolved to an almost normal state, her hs-CRP level was 0.043 mg/dl (MMSE=25) at 6 months and 0.028 mg/dl (MMSE=27) at 1 year. From these results, we speculate that a CRP level of ≥ 0.1mg/dl might constitute low-grade inflammation, and that a level <0.05 mg/dl might not, i.e., there might be cut-off point between from 0.05 to 0.1 mg/dl whether low grade inflammation or not. However, in only one case we can’t confirm the conclusion. Larger studies of the relationships between clinical symptoms and hs-CRP in depression and AD are needed. Moreover, in our hospital, the normal range of CRP is regarded as <0.30 mg/dl. Therefore, the patient was not considered to have high-grade inflammation when she developed cognitive dysfunction. However, her inflammatory system was considered to be related with “low grade inflammation”. CRP and hs- CRP are measured the same protein. CRP is measured by turbidimetric immunoassay method and measurement limes is 0.1 mg/dl. However, more low level of CRP is considered to be related with arterial sclerosis and gets possible to measure CRP which is microdose more by latex coagulating method method and calls it with hs-CRP [15]. However, a report suggests that there does not appear to be a significant relationship between depression and hs-CRP levels after adjusting for confounding factors such as body mass index, diabetes mellitus, and cardiovascular disorders [16]. Therefore, we consider that when confounding factors are controlled for, there is a significant relationship between cognitive function and hs-CRP levels, and that the assessment of hs-CRP is a suitable marker for assessing cognitive function in individual patients who have been diagnosed with depression (pseudodementia) or dementia (true dementia) by longitudinal observation. Although we did not have the data between our patient’s first visit to our clinic and her visit 1 year later, we do not think she experienced any notable changes in disease state or body weighs. Moreover, she had not had peri-odontoid disease and/or metabolic syndrome as a source of chronic inflammation during this period.
We also speculate that amelioration of cognitive dysfunction was related to suppression of inflammation related to the cholinergic antiinflammatory pathway [17-19] because treatment with the ChEI donepezil was followed by a decrease in hs-CRP levels and improvement of cognitive function. Our patient was 79 years old when she visited our hospital the first time. Therefore, her ACh should have been downregulated. However, at this stage, compensatory upregulation of choline acetyltransferase (ChAT) [20,21], an enzyme that makes ACh, might have kept her ACh at normal levels. In this case, mental stress was present, which possibly prevented upregulation of ChAT and compensation. We speculate that hyperactivation of inflammation, and ameliorating the symptoms of cognitive dysfunction (pseudodementia) caused by “low grade inflammation”, which is regulated by the “cholinergic anti-inflammatory pathway”.
Conclusion
In summary, this case highlights three important issues. First, cognitive dysfunction due to depression (pseudodementia) may be related to low-grade inflammation. Second, hs-CRP may be a suitable marker for low-grade inflammation. Third, treatment with ChEI may suppress this low-grade inflammation, although upregulation of ACh may also suppress it. In our patient, inflammation appeared to be related to the cholinergic anti-inflammatory pathway. To confirm this finding, larger studies of the relationships between clinical symptoms and hs-CRP in depression and AD are warranted.
Conflicts of Interest
Koji Hori received lecture fees from Eisai Co. Ltd., Pfizer Japan Inc., Novartis Pharma KK, Daiichi Sankyo Inc., Ono Pharmaceutical Co. Ltd., Janssen Pharmaceutical KK, Yoshitomi Yakuhin Co. Meiji Seika Pharma Co. Ltd., and Mitsubishi Tanabe Pharma Co. Mitsugu Hachisu received lecture fees from Meiji Seika Pharma Co. Ltd. and Mitsubishi Tanabe Pharma Co. However, the sponsors had no role in the study design, data collection and analysis (including in our previous published articles), decision to publish, or preparation of this manuscript.
Disclosure Statement
There is no need for measuring hs-CRP because this evaluation is one of the clinical evaluations of the elaborated assessment of her inflammatory system. The Patient and her daughter were understood this. Proofreading fee and fee for publishing will be paid by Department of Neuropsychiatry in St. Marianna University School of Medicine. Koji Hori received funding from Eisai Co. Ltd., Daiichi Sankyo Inc. Ono Pharmaceutical Co. Ltd. and Ito Memorial Fundings. Mitsugu Hachisu received funding from Astellas Pharma Inc., Meiji Seika Pharma Co. Ltd., Dainippon Sumitomo Pharm Co. Ltd., Eli Lilly Japan KK and Shionogi & Co. Ltd. However, the sponsors had no role in the study design, data collection and analysis (including in our previous published articles), decision to publish, or preparation of this manuscript.
Author Contributions
Koji Hori mainly coordinated this report. Misa Hosoi, Kimiko Konishi, Mitsugu Hachisu, and Hiroi Tomioka are all members of the Showa University Dementia Study Group and critically checked the drafts of the manuscript. Michiho Sodenaga and Ouga Sasaki are members of the geropsychiatry study group in the Department of Neuropsychiatry, St. Mariana University School of Medicine and critically checked the drafts of the manuscript.
References
- Leboyer M, Oliveira J, Tamouza R, Groc L (2016) Is it time for immunopsychiatry in psychotic disorders? Psychopharmacology (Berl) 233: 1651-1660.
- Suvisaari J, Mantere O (2013) Inflammation theories in psychotic disorders: A critical review. Infect Disord Drug Targets 13: 59-70.
- Haring L, Koido K, Vasar V, Leping V, Zilmer K, et al. (2015) Antipsychotic treatment reduces psychotic symptoms and markers of low-grade inflammation in first episode psychosis patients, but increases their body mass index. Schizophr Res 169: 22-29.
- Singh B, Chaudhuri TK (2014) Role of C-reactive protein in schizophrenia: An overview. Psychiatry Res 216: 277-285.
- Folstein MF, Folstein SE, M Hugh RP (1975) “Mini-Mental State.†A practical method for grading the cognitive state of patients for the clinician. J Psychiatry Res 12: 95-112.
- Kitamura T (1991) Mini-Mental State (MMS) In: Otsuka T, Homma A (eds). Assessment of manual of intellectual function for demented elderly. (In Japanese) Tokyo, Japan world Planning Co., LTD: 35-38.
- Petersen RC (2004) Mild cognitive impairment as a diagnostic entity. J Intern Med 256: 183-194.
- Li P, Hsiao IT, Liu CY, Chen CH, Huang SY, et al. (2017) Beta-amyloid deposition in patients with major depressive disorder with differing levels of treatment resistance: A pilot study. EJNMMI Res 7: 24.
- Zalli A, Jovanova O, Hoogendijk WJ, Tiemeier H, Carvalho LA (2016) Low-grade inflammation predicts persistence of depressive symptoms. Psychopharmacology (Berl) 233: 1669-1678.
- van Dooren FE, Schram MT, Schalkwijk CG, Stehouwer CD, Henry RM, et al. (2016) Associations of low grade inflammation and endothelial dysfunction with depression - The Maastricht Study. Brain Behav Immun 56: 390-396.
- Misiak B, Leszek J, Kiejna A (2012) Metabolic syndrome, mild cognitive impairment and Alzheimer's disease--The emerging role of systemic low-grade inflammation and adiposity. Brain Res Bull 89: 144-149.
- Cubała WJ, Landowski J (2014) C-reactive protein and cortisol in drug-naïve patients with short-illness-duration first episode major depressive disorder: Possible role of cortisol immunomodulatory action at early stage of the disease. J Affect Disord 4: 534-537.
- Mommersteeg PM, Meeuwis SH, Denollet J, Widdershoven JW, Aarnoudse W et al. (2014 C-reactive protein and fibrinogen in non-obstructive coronary artery disease as related to depressive symptoms and anxiety: Findings from the TweeSteden Mild Stenosis Study (TWIST). J Psychosom Res 77: 426-429.
- Krogh J, Benros ME, Jørgensen MB, Vesterager L, Elfving B, et al. (2014) The association between depressive symptoms, cognitive function and inflammation in major depression. Brain Behav Immun 35: 70-76.
- Gomez-Marcos MA, Recio-RodrÃguez JI, Patino-Alonso MC, Agudo-Conde C, Gomez-Sanchez L, et al. (2012) Relationships between high-sensitive C-reactive protein and markers of arterial stiffness in hypertensive patients. Differences by sex. BMC Cardiovasc Disord 12: 37.
- Hayashino Y, Mashitani T, Tsujii S, Ishii H; Diabetes Distress and Care Registry at Tenri Study Group (2014) Elevated levels of hs-CRP are associated with high prevalence of depression in Japanese patients with type 2 diabetes: The Diabetes Distress and Care Registry at Tenri (DDCRT 6). Diabetes Care 37: 2459-2465.
- Bernik TR, Friedman SG, Ochani M, DiRaimo R, et al. (2002) Pharmacological stimulation of the cholinergic anti-inflammatory pathway. J Exp Med 195: 781-788.
- Pavlov VA, Ochani M, Gallowitsch-Puerta M, Ochani K, Huston JM, et al. (2006) Central muscarinic cholinergic regulation of the systemic inflammatory response during endotoxemia. Proc Natl Acad Sci U S A 103: 5219-5223.
- Mabley JG, Pacher P, Szabo C (2009) Activation of the cholinergic anti-inflammatory pathway reduces ricin-induced mortality and organ failure in mice. Mol Med 15: 166-172.
- Gilmor ML, Erickson JD, Varoqui H, Hersh LB, Bennett DA, et al. (1999) Preservation of nucleus basalis neurons containing choline acetyltransferase and the vesicular acetylcholine transporter in the elderly with mild cognitive impairment and early Alzheimer's disease. J Comp Neurol 411: 693-704.
- DeKosky ST, Ikonomovic MD, Styren SD, Beckett L, Wisniewski S, et al. (2002) Upregulation of choline acetyltransferase activity in hippocampus and frontal cortex of elderly subjects with mild cognitive impairment. Ann Neurol 51:145-155.
Citation: Hori K, Konishi K, Hosoi M, Sodenaga M, Kamatani H, et al. (2017) Case Report: High-Sensitivity C-Reactive Protein is a Potentially Useful Marker of the Need for Psychotic Treatment for Cognitive Dysfunction Related to Low- Grade Inflammation. J Alzheimers Dis Parkinsonism 7: 402. DOI: 10.4172/2161-0460.1000402
Copyright: © 2017 Hori K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6074
- [From(publication date): 0-2017 - Oct 19, 2025]
- Breakdown by view type
- HTML page views: 5092
- PDF downloads: 982