Case Report: First Branchial Cyst
Received: 11-Oct-2020 / Accepted Date: 19-Nov-2020 / Published Date: 26-Nov-2020
Abstract
Branchial cleft anomalies are not so rare congenital anomalies of neckpresenting as swelling (cyst/abscess), fistula or discharging sinuses. They arise due tomal development of the branchial arches.The most common ions are the second branchialcleft abnormalities. Here is a case report of the clinical presentation of the First branchialcleft cyst along with the relevant anatomy, diagnosis, management and outcome.
Keywords: Branchial cyst; External auditory canal; Blind sac
Introduction
Branchial cleft anomalies are not so rare congenital anomalies of neck presenting as swelling(cyst/abscess), fistula or discharging sinuses. They arise from the developmental errors of thebranchial arches, each level being evident as a distinct abnormality with a characteristicpresentation. Here is a case report of the clinical presentation of the First branchial cleft cystalong with the relevant anatomy, diagnosis, management and outcome.
Case report
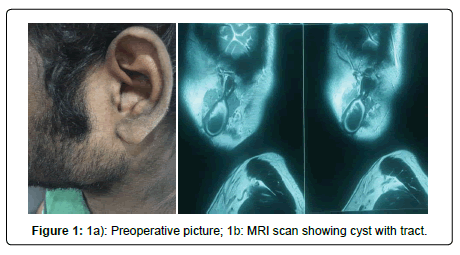
A 23 year old male reported to our OPD with complaints of swelling located above the angle of mandible on left side since past 16 years. The usual course of the swelling for the past years was that it used to progressively increase in size and after reaching a certain size (usually 4x3 cm) decreased in measurements following a serious discharge from the ipsilateral external auditory canal (EAC). The swelling never completely disappeared. Within exception to the above, for past 10 days the patient complained of an increase in the intensity of pain over the swelling and there was no reduction in size even after the discharge from EAC. On examination a well defined swelling measuring 5X 4 cms was found on angle of mandible on left side. It was cystic, fluctuant, mobile, tender, with normal overlying skin and free from underlying structures. The pressure on swelling caused release of mucopurulent discharge,coming out from the ipsilateral ear trough an opening on the floor of EAC. MRI neck described swelling as cystic swelling filled with central debris lying onsubcutaneous plane of left parotid with a track extending from the cranial end of the swelling to the ipsilateral EAC floor at the bony cartilaginous junction (Figures 1 a and 1 b).
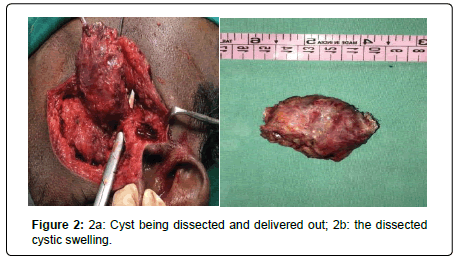
In light of the clinical and radiological data a diagnosis of First Branchial Cleft Cyst Type I was made.The patient was planned for exploration and excision of branchial cyst.Surgery was planned via an anterior superficial parotidectomy approach. A facial nervemonitor was used during the entire duration of operation to identify and preserve the facialnerve in view of anticipated risk of damage to facial nerve for the given location of theswelling. After the incision and superficial dissection a large subcutaneous cystic swellingfilled with keratin and debris was identified and mobilized. All branchesof facial nerve were identified and preserved. The tract seen extending from swelling till floorof EAC, was identified, dissected and excised. Two layered blind sac closure of the remnantEAC floor skin was done. The whole swelling along with tract was excised and sent for histopathological examination (Figures 2 a and 2b).
The histo-pathological reported stated the swelling to be lined by stratified squamous epithelium with surrounding lymphoid tissue, and superimposed inflammatory changes. These findings were suggestive of branchial cleft cyst. Post-operative patient had House- Brackmann Grade 2 facial palsy. This was attributed to the edema of facial nerve during the post-operative period. The patient was followed up for a period of 2 years and showed no recurrence till date with no signs of residual facial palsy (Figure 2 c).
Discussion
Branchial arches are 6 paired arches, embryologically origins of various structures of headand neck. Incomplete regression of these arches during 6th and 7th weeks of gestation givesrise to branchial cleft anomalies. There are various theories of origin of the cleftanomalies. The most popularly excepted ones are: Incomplete obliteration of br anchialmucosa,Prevestigealremanants of cervical sinus,incomplete obliteration ofthymopharyngeal duct and Cystic degeneration of cervical lymph node [1, 2].
One popularly believed theory for defining branchial cleft cyst isKing’s criteria is that, anycyst arising outside the midline of the neck and having lymphoepithelial characteristicsshould be regarded as a branchial cyst[3].First branchial cleft anomalies are rare finding accounting less than 8% of all branchial cleftanomalies with incidence of 1 per million population per year[4]. First branchial arch usually completes its development into various structures by 6th -7th week of intrauterine life. Itcontributes to development of maxilla, mandible and ear (Eustachian tube, EAC and parts ofMiddle Ear). As a result first branchial cleft anomaly can be located anywhere along thenasopharynx, EAC and middle ear. They are further categorized into type I and Type II. Type I are the ones which have openings in the floor of EAC with location of the swellingnear EAC, on parotid or angle of mandible. Type I is ectodermal in origin with stratifiedsquamous epithelium lining and are considered as duplication of membranous part of EAC. Type II is located in region of submandibular gland or anterior triangle of neck. Type II isboth ectodermal and mesodermal in origin. The parotid gland and facial nerve develop laterto the first branchial cleft structures and so the vestigeal branchial cleft remnants are locatedin relation to them. Facial nerve has varied relations to First branchial cleft cyst (FBCC) asconcluded in study article by Solares and associates and D’Souza and colleagues [5, 6]. Thisfact makes it mandatory for the surgeon treating FBCC to be skilled in handling of facialnerve. Clinically the first branchial cleft anomalies may present with cystic swelling/ infected,discharging sinus, fistula in preauricualr region, parotid region or at angle of mandible. Theymay present with unilateral discharging ear. The literature broadly states that presentation ofFBCC as fistulas or sinuses usually occurs in early life and cyst usually in the adolescent oradult. This is in accordance to our present case where an adolescent male presented with anodular swelling at angle of mandible with ipsilateral ear discharge.Inspite of history and clinical examination FBCC is often misdiagnosed due to vast numberof conditions presenting with same location and clinical features. The various differentialdiagnosis being: Odontogenic infection, Parotid swelling, Tuberculouslymphadenitis,Lipoma, Cystic hygroma, Carotid body tumours, Thyroglossal duct cysts, Suppurativelymphadenitis, Dermoid cysts, Neurofibroma, Haemangioma, Lymphangioma ,Teratoma, Ectopic salivary tissue, Pharyngeal diverticulum, Laryngocele,Plunging ranula andMalignancies involving the lymph nodes (elderly). In a case series study by Daniel andcoworkers on 15 cases of nonmalignant mass in the parotid area, most common cause of suchmmasses was first branchial arch anomalies. To aid the diagnosis and treatment radiologicalinvestigations like CT scan and MRI are performed along with FNAC of the swelling. BothCT and MRI are unable to distinguish FBCC from lymphangioma of children and metastaticsquamous cell carcinoma in adults. FNAC may help focus light on these differentials. TheFNC criteria for FBCC mainly include thick yellow, pus-like fluid with nuclear, squamousepithelial cells on a background of amorphous debris [7].Radiologically diagnosis of FBCC is aided with MRI and CT scan. MRI is preferred overCT scan in case of FBCC as it helps in better delineation of cystic nature and relationshipwith surrounding structures. Immunohistochemistry may be used as an additional tool fordiagnosis. The IHC of the cytic fluid reflects positive for co-expression of simple andstratified epithelial cytokeratins[8].Once the diagnosis of FBCC is confirmed the ideal treatment is complete excision of the cystwith tract with preservation of facial nerve and repair of external ear structures if required. Inpresent case, via a superficial parotidectomy approach, the cyst was removed completely withthe tract and two layered closure of remnant EAC skin. The facial nerve was identified andpreserved with the help of facial nerve monitor. No reconstruction was required. Facial nerve monitor has been widely used in various surgeries of the parotid andsubmandibular gland due to their anatomical relation with the facial nerve. As rare is theFBCC so is its surgery and hence the use of facial nerve monitor. Although a rare indicationof facial nerve monitor it is very valuable and a recommended aid to surgery because ofvaried relations of facial nerve to the FBCC.Complication of the treatment of the cyst includes: residual cyst, recurrent cyst and damageto facial nerve and adjoining structures, percutaneous fistula. Alternative treatment likesclerotherapy though sounds promising has not been proven to be effective [9].Recurrence is often nil if the entire cyst wall and tract is removed. In our case no recurrencewas seen in 2 years follow-up period. But in literature recurrence has been found to be 4.2%over 2 year follow up period. The malignant transformation of FBCC is very rare comparedto other cysts of neck.The common causes for recurrence are misdiagnosis and incompletesurgical resection.
Conclusion
FBCC are rare variety of branchial cleft anomalies. Usually present in late childhood andyoung and adulthood. The most common clinical presentation is cystic swelling in parotidregion (near angle of mandible) with fistulous tract present having its opening at or above thelevel of hyoid. As the diagnosis is often difficult, the treatment is either delayed or incorrectresulting into recurrence of the disease and chronic inflammation within the swelling mayresult in malignant transformation.
References
- Ascherson GM. Defistulis Colli congenitis fissuratum branchialium in mammalibus avibusque historica succincta. CH Jonas, Berolini, 1832; 1–21.
- Thomaidis V, Seretis K, Tamiolakis D, Papadopoulos N. (2006) Tsamis Branchial cysts. A report of 4 cases. Acta Dermatoven APA 15: 85–89.
- Bhanote M, Yang GC. (2008) Malignant first brancial cleft cysts presented as submandibular abscesses in fine needle aspiration: Report of three cases and review of literature. Diagn Cytopathol 36:876-881.
- Wei YK, Wang KJ, Jou YL, Chang YH, Chou CS. (2005) Type II first branchial cleft anomaly Am case report. Tzu Chi Med J 357–60.
- Solares CA. (2003) Intracapsular tonsillar reduction (partial tonsillectomy): reviving a historical procedure for obstructive sleep disordered breathing in children. Otolaryngol Head and Neck Surg 129: 532-538.
- Souza AR. (2002) Updating concepts of first branchial cleft defects: a literature review. International J. Paediatr Otorhinolaryngol 62: 103-109.
- Lee HJ, Kim EK, Hong S. (2006) Sonographic detection of intrathyroidal branchial cleft cyst: A case report. Korean J Radiol 7: 149-151.
- Flanagan PM. Roland HJ, Jones AS. (1994) Cervical node metastases presenting with features of branchial cysts. J Laryngol Otol 108: 1068–1071.
- Howard DJ, Lund VJ. ( 2008) Pharynx, larynx and neck—branchial cleft cyst. Indian J Otolaryngol Head Neck Surg 727–729.
Citation: Mishra S (2020) Case Report: First Branchial Cyst. Otolaryngol (Sunnyvale) 10: 501.
Copyright: © 2020 Mishra S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3549
- [From(publication date): 0-2020 - Mar 02, 2026]
- Breakdown by view type
- HTML page views: 2615
- PDF downloads: 934