Research Article Open Access
Carbon-dioxide Laser in the Treatment of Trigeminal Neuralgia: A Preliminary Study
Somchai Sessirisombat*Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Chulalongkorn University, Bangkok, Thailand
- *Corresponding Author:
- Somchai Sessirisombat
Department of Oral and Maxillofacial Surgery
Faculty of Dentistry, Chulalongkorn University
Bangkok, Thailand
Tel: (66) 2218-8587
Fax: (66) 2218-8581
E-mail: somchaiomfs@gmail.com
Received Date: January 29, 2017; Accepted Date: February 08, 2017; Published Date: February 15, 2017
Citation: Sessirisombat S (2017) Carbon-dioxide Laser in the Treatment of Trigeminal Neuralgia: A Preliminary Study . J Interdiscipl Med Dent Sci 5: 208. doi:10.4172/2376-032X.1000208
Copyright: © 2017 Sessirisombat S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Objective: This study was performed to evaluate the results of carbon dioxide laser in the treatment of trigeminal neuralgia (TN). Methods: Thirty six patients (11 men, 25 women) with refractory TN underwent peripheral nerve ablation with CO2 laser using low power defocused mode. Pain intensity was determined by numerical rating scales at preoperation, 1 week, 1 month, 3 months, 6 months, and 12 months post-operation. One way ANOVA was used to determine statistical significance. Results: There were significant differences in pain between pre-operation and 1 week, 1 month, 3 months, 6 months, and 12 months post-operation (pain score=9.38 ± 0.91, 3.15 ± 3.24, 1.00 ± 1.41, 0.63 ± 1.18, 0.75 ± 1.16 and 1.63 ± 1.99 respectively; p<0.05). Thirty four patients had some degree of prolonged paresthesia of the effected nerves, while two patients had no sensory alteration but the pain was relieved. Conclusions: Neural ablation with CO2 laser can be an alternative treatment for patients with TN who do not respond to the medical treatment or cannot tolerate the side effects of medication or do not want to have intracranial surgery. The only complication was prolonged paresthesia of the effected nerve. However, further study with a larger group of patients and longer observation period are recommended to evaluate the outcome of this treatment.
Keywords
Trigeminal neuralgia; Carbon dioxide laser
Introduction
TN is a sudden, usually unilateral, severe, brief, stabbing, recurrent pain in the distribution of one or more branches of the trigeminal nerve. Pain is commonly evoked by trivial stimuli including washing, shaving, smoking, talking and brushing teeth, but may also occur spontaneously. The pain may remit for varying periods [1,2]. TN affects women more than men and usually occurs in the sixth or seventh decades of life. The painful attacks are most common in the second and third division of trigeminal nerve and effect the right side more than the left side [1]. The cause of TN may be from pathologies of the nerve roots. Most cases are caused by compression of the trigeminal nerve root by an intracranial arterial or venous loop.
However, compression by tumors and arteriovenous malformations are rare. In a few cases, TN is caused by a primary demyelinating disorder which is common in patients with multiple sclerosis [2]. The first line of treatment for this condition is medication. Carbamazepine is the drug of choice, and there are some alternative drugs such as phenytoin, oxcarbazepine, and gabapentin. Most of these medications have some side effects such as drowsiness, dizziness, ataxia, vertigo, blur vision, nausea, vomiting, aplastic anemia, and impaired liver function [2]. Drug tolerance can also occur in some patients who take a long term medication. When patients do not respond to the drugs or develop intolerable side effects, surgical treatment should be considered [3]. There are several surgical procedures to treat TN, including microvascular decompression (MVD) which is the most accepted procedure due to its safety and high success rate [4], Gasserian ganglion ablative procedures and stereotactic radiosurgery that aims at destroying the sensory function, and gamma knife, a recently sophisticated tool and less invasive peripheral nerve surgery. The peripheral nerve surgery aims to block the afferent pathway to the central nervous system [5]. As the risk of complications is small, it can be justified as an effective palliative treatment prior to a much more complicated neurosurgical procedure. In this study, we used Carbon dioxide (CO2) laser which is one of the most widely used lasers in oral tissue and also neural tissue [6,7]. As a previous study demonstrated that heat can be used to interrupt pain conduction pathway [8], thus it is believed that heat produced from laser energy can also be used to reduce the neuropathic pain by creating injury to the peripheral nerve. The aim of this study was to evaluate the effects of CO2 laser used for the treatment of TN.
Materials and Methods
Thirty six patients (11 men and 25 women) with refractory TN who attended the Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Chulalongkorn University were enrolled in this study. Demographic data and clinical characteristics of the patients were assessed. Clinical characteristics of pain were recorded. All patients had been treated with high dose medication but became refractory or could not tolerate adverse effects of the drugs. None had been treated with any surgical procedures prior to the CO2 laser treatment. Informed consents were obtained from all patients. The study was approved by the ethics committee of the Faculty of Dentistry, Chulalongkorn University.
Surgical techniques
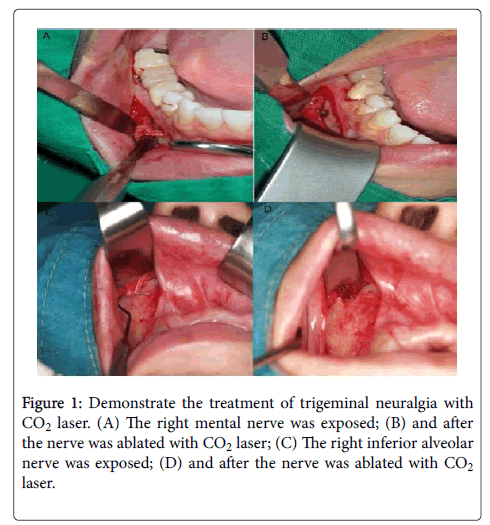
A CO2 laser unit, Captain 30 (SM Medical, Korea) was used in all patients. After local anesthetic block and infiltrate, the mucoperiosteal flaps were raised near the foramen that the affected nerve came from the bone, the nerves were exposed approximately 1 cm. in length and were lased with CO2 laser using a power of 5 W, continuous, defocused mode to the entire exposed nerves for about 30 seconds (Figure 1), then the flaps were closed with 3-0 Vicryl Rapide* sutures (Johnson and Johnson, USA). Post-operative analgesic was prescribed using 400 mg Ibuprofen for postoperative pain. Pain intensity was evaluated using numerical rating scales (NRS) at pre-operation then 1 week, 1 month, 3 months, 6 months and 12 months after operation. Postoperative complications were also assessed.
Statistical analysis
All the data were analyzed with SPSS 17.0 for statistical analysis. Pain intensity before and 1 week, 1 month, 3 months, 6 months and 12 months after operation were analyzed using One-way ANOVA. A Pvalue <0.05 was considered to be statistically significant.
Results
The demographic data and clinical characteristics of the patients in this study were shown in Table 1. All patients had taken carbamazepine for an average of 6.4 years and chose surgical intervention. There were significant differences in pain scores between preoperative (day 0) and 1 week, 1 month, 3 months, 6 months and 12 months postoperative (Table 2). Five patients experienced postoperative pain and swelling at the surgical site. Thirty four patients had some degree of prolong paresthesia of the effected nerves, while two patients had no sensory alteration after 6 months post-operation but the pain was relieved. The paresthesia of the nerves was gradually improved in most patients and they felt more favorable than pain.
| Gender | |
|---|---|
| Female | 25 |
| Male | 11 |
| Age range (mean±SD) | 41-84 (61.02±12.43) |
| Duration of pain prior to surgery: years (mean±SD) | 1-20 (6.71±6.43) |
| Number of affected nerve division | |
| Maxillary branch | 16 |
| Mandibular branch | 20 |
| Number of affected sides | |
| Right | 22 |
| Left | 14 |
Table 1: Clinical data of thirty six TN patients.
| Visit | Pain scores (Mean ± SD) | P-value |
|---|---|---|
| Preop | 9.38±0.91 | 0.000 |
| 1 week postop | 3.15±3.24 | |
| Preop | 9.38±0.91 | 0.000 |
| 1 month postop | 1.00±1.41 | |
| Preop | 9.38±0.91 | 0.000 |
| 3 months postop | 0.63±1.18 | |
| Preop | 9.38±0.91 | 0.000 |
| 6 months postop | 0.75±1.16 | |
| Preop | 9.38±0.91 | 0.000 |
| 12 months postop | 1.63±1.99 |
Table 2: Comparison of preoperative NRS scores with 1 week, 1, 3, 6 and 12 months postoperative NRS scores.
Discussion
Microvascular decompression (MVD) is a safe and effective treatment for TN. Success rates were approximately 90% [4,9]. Mortality and morbidity rates were 0.3% and 3.8% respectively [10]. Surgical manipulations at the Gasserian ganglion such as balloon compression [11], radiofrequency thermocoagulation [12] and percutaneous glycerol rhizolysis [13] damage sensory function of the trigeminal nerve. Sensory disturbances are the most common complications of these ablative procedures. Moreover, there are other complications such as temporary visual disturbance, smell and hearing loss, anesthesia dolorosa, postoperative herpetic eruption resulting from surgical injury to the adjacent structures [3,11-13]. Some elderly or medically compromised patients are not fit for the more invasive intracranial interventions. Thus, peripheral surgery which is less invasive becomes an alternative treatment for these patients and those who wish to avoid risks of the intracranial surgery [14].
There are several peripheral surgical techniques suggested for TN, all of which aim at blocking sensory conduction from the trigger zone [5]. Peripheral surgical procedures included neurectomy, cryotherapy, alcohol injection, glycerol injection, high concentration of anesthetic nerve block, and jaw bone cavity curettage.
Peripheral neurectomy is a simple procedure but sensory disturbance and recurrence are the main problems. Recurrence occurs between 12 and 15 months after neurectomy and between 9 and12 months after a second procedure [15]. While the average duration of pain relief in 145 patients who underwent cryotherapy was only 6 months [16].
Alcohol injection can relief the pain immediately after injection but duration of action is limited and some patients have experienced burning sensation. Moreover, various complications have been reported including diplopia, sensory disturbances and tissue necrosis [17]. The peripheral alcohol injection is complicated when repeated administration due to 6 tissue fibrosis or necrosis [18]. To alleviate the adverse effects of neurolytic agents, peripheral nerve blockage using high concentration of local anesthetic agents had been used. Trigeminal nerve blocked with local anesthesia is reversible and nontraumatic but only for transient relieve of pain, and it is suggested to use in elderly patients or patients with poor systemic conditions [19].
Laser has become an effective surgical tool to manage several pathologic conditions in oral tissue. It is also believed that laser can be used to block pain pathway by creating a minimal peripheral nerve injury with laser energy [8]. Letcher and Go studied the effect of heat on peripheral nerve and found that by heating peripheral nerves could selectively destroy small delta and C fiber that conduct the pain pathways but the large fibers which transmit other kinds of sensory information were preserved [20]. This might provide a postulated mechanism for application of heat from laser energy to manage pain. Therefore, using the defocused beam to reduce the power density of the CO2 laser to lase the peripheral nerve is possible to control the neuralgic pain [21].
This is the first study to use CO2 laser for treatment of TN. In our study, low power of CO2 laser energy was used to treat patients who refused major surgical treatment. The results revealed that there was a significant reduction of pain scores after treatment. This was similar to other studies using other more invasive peripheral surgical procedures which their results showed that pain level was also significantly decreased [22-24] and this allowed patients to continue their normal daily activity and improve their quality of life. The only complication of this technique was prolonged paresthesia which is also common in other peripheral procedures [15-17] but most patients did not concern about numbness. This finding indicated that TN can be managed with CO2 laser which is a cost effective, safe and a simple technique with high patients’ acceptance [7]. However, there were limitations of this technique because it was difficult to apply the laser beam to the whole surface of the nerve with thick soft tissue flap and the poor accessibility especially the infraorbital nerve. Some patients had small diameter of the nerves and it was difficult to decide the optimum and effective laser power and lasing duration that made different responses among the patients.
Conclusion
Nerve lasing with CO2 laser can be an alternative treatment for patients with trigeminal neuralgia who do not respond the medical treatment or cannot tolerate the adverse effects of medications with a satisfactory result. However, further study with a larger group of patients with longer observation of symptom free period should be conducted to evaluate more efficiency of this treatment.
Conflict of Interest
This study had no conflict of interest.
Acknowledgement
This study was financially supported by the 90th Anniversary of Chulalongkorn University Fund (Ratchadaphiseksomphot Endowment Fund).
References
- Mauskop A (1993) Trigeminal neuralgia. J Pain Symptom Manage 8:148-154.
- Siddiqui MN, Siddiqui S, Ranasinghe JS, Furgang FA (2003) Pain management: Trigeminal neuralgia. Hosp physician 39:64-70.
- Toda K (2008) Operative treatment of trigeminal neuralgia: review of current techniques. Oral Surg Oral Med Oral Pathol Oral RadiolEndod106: 788-805.
- Barker FG, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD (1996)The long-term outcome of microvascular decompression for trigeminal neuralgia. N Eng J Med 334:1077-1083.
- Mason DA (1972) Peripheral neurectomy in the treatment of trigeminal neuralgia of the second and thirds divisions. J Oral Surg 30:113-120.
- Strauss RA, Fallon SD (2004) Lasers in contemporary oral and maxillofacial surgery. Dent Clin N Am 48:861-888.
- Devaux BC, Roux FX (1996) Experimental and clinical standards, and evolution of lasers in neurosurgery. ActaNeurochirurgica 138:1135-1147.
- Xu D, Pollock M (1994) Experimental nerve thermal injury. Brain 117:375-384.
- Apfelbaum R (2002) Comparison of the long term results of microvascular decompression and percutaneous trigeminal neurolysis for the treatment of trigeminal neuralgia. IntCongrSer1247:629-643.
- Kalkanis SN,Eskandar EN, Carter BS, Barker FG (2003) Microvascular decompression surgery in the United States, 1996 to 2000: mortality rates, morbidity rates, and the effects of hospital and surgeon volumes. Neurosurg 52:1251-1261.
- Stomal-Slowinska M, Slowinski J, Lee TK, Uitti RJ, Deen HG, et al. (2011) Correlation of clinical findings and results of percutaneous balloon compression for patients with trigeminal neuralgia. ClinNeurolNeurosurg113:14-21.
- Silverberg GD, Britt RH (1987) Percutaneous radio-frequency rhizotomy in the treatment of trigeminal neuralgia. West J Med 129:97-100.
- Fujimaki T, Fukushima T, Miyazaki S (1990) Percutaneous retrogasserian glycerol injection in the management of trigeminal neuralgia: long-term follow-up results. J Neurosurg 73:212-216.
- Benoliel R, Eliav E (2008) Neuropathic orofacial pain. Oral MaxillofacSurgClin N Am 20:237-254.
- Cerovic R, Juretic M, Gobic MB (2009)Neurectomy of the trigeminal nerve branches: Clinical evaluation of an "obsolete" treatment. J CraniomaxillofacSurg 37:388-391.
- Zakrzewska JM (1991)Cryotherapy for trigeminal neuralgia: A 10 year audit. Br J Oral MaxillofacSurg29:1-4.
- McLeod NM, Patton DW (2007) Peripheral alcohol injections in the management of trigeminal neuralgia. Oral Surg Oral Med Oral Pathol Oral Radio Endod 104:12-17.
- Fardy MJ, Patton DW (1994) Complications associated with peripheral alcohol injection in the management of trigeminal neuralgia. Br J Oral MaxillofacSurg 32:387-391.
- Goto F, Ishizaki K, Yoshikawa D, Obata H, Arii H, et al. (1999) The long lasting effects of peripheral nerve blocks for trigeminal neuralgia using a high concentration of tetracainedissolved in bupivacaine. Pain 79:101-103.
- Letcher FS, Goldring S (1968) The effect of radiofrequency current and heat on peripheral nerve action potential in the cat. J Neurosurg29:42-47.
- Kahraman SA (2004) Low-level laser therapy in oral and maxillofacial surgery. Oral MaxillofacSurgClin N Am 16:277-288.
- Lemos L, Fontes R, Flores S, Oliveira P, Almeida A (2010) Effectiveness of the association between carbamazepine and peripheral analgesic block with ropivacaine for the treatment of trigeminal neuralgia. J Pain Res 3:201-212.
- Dergin G, Gocmen G, Sener BC (2012) Treatment of trigeminal neuralgia with bupivacaine HCL using a temporary epidural catheter and pain pump: preliminary study. J CraniomaxillofacSurg40:124-128.
- Eckerdal A, Bastian HL (1996) Can low reactive-level laser therapy be used in the treatment of neurogenicfacial pain? A double-blind, placebo controlled investigation of patients with trigeminal neuralgia. Laser Therapy8: 247-252.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 5428
- [From(publication date):
February-2017 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 4459
- PDF downloads : 969