Case Report Open Access
Candida Albicans Ventriculitis Post Trans-Sphenoidal Surgery. Case Report and Literature Review
Bukhari EE1*, Ajlaan A2, Bakheet MH1, Albarag A3, Alotibi EF3 , Alrabiaah AA1 and Alzamil AF1
1Department of Pediatric Infectious Diseases, College of Medicine, King Khalid University Hospital and King Saud University, King Saud University Medical City, Riyadh, Saudi Arabia
2Department of Neurosurgery, College of Medicine, King Khalid University Hospital and King Saud University, King Saud University Medical City, Riyadh, Saudi Arabia
3Department of Pathology , College of Medicine, King Khalid University Hospital and King Saud University, King Saud University Medical City, Riyadh, Saudi Arabia
4Discipline of Pharmaceutics, School of Pharmacy, University of the Western Cape, Bellville 7535, South Africa
- *Corresponding Author:
- Elham Essa Bukhari
Department of Pediatric Infectious Diseases
College of Medicine
King Khalid University Hospital and King Saud University
King Saud University Medical City, Riyadh, Saudi Arabia
Tel: +966114679963
E-mail: ebukhari@ksu.edu.sa
Received date: April 25, 2016; Accepted date: May 05, 2016; Published date: May 09, 2016
Citation: Bukhari EE, Ajlaan A, Bakheet MH, Albarag A, Alotibi EF, et al. (2016) Candida Albicans Ventriculitis Post Trans-Sphenoidal Surgery.Case Report and Literature Review. J Infect Dis Ther 4:280. doi:10.4172/2332-0877.1000280
Copyright: © Bukhari EE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Infectious Diseases & Therapy
Abstract
Central nervous system (CNS) infection with Candida in children is rare. In this report, we describe a Saudi child diagnosed with suprastellar astrocytoma brain tumor who experienced Candida albicans meningitis with ventriculitis post-trans-sphenoidal brain tumor resection. The patient was treated successfully with intravenous amphotericin B and fluconazole.
Keywords
Candida albicans ; Infection; Meningitis
Introduction
Candida infection of the central nervous system (CNS) is relatively unusual in children. It is commonly reported among premature neonates and immunocompromised or post-surgical patients. Patients undergone neurosurgical procedure are at particular risk as the use of CSF shunt devices is a common practice in neurosurgery and infection of the shunt is the most frequently reported complication [1-3].
Herein, we report an unusual presentation of Candida albicans meningitis and ventriculitis in a young child who underwent transsphenoidal surgery.
Case report
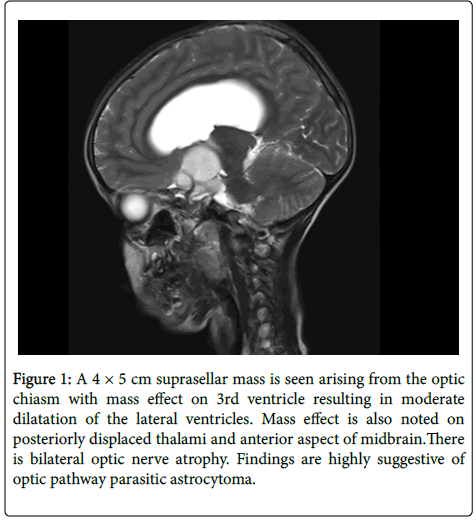
A four and half-year-old female child was admitted to the pediatric ward of our hospital with fever and excessive sleep since one week. Two weeks before admission she underwent trans-sphenoidal removal of suprasellar pilocytic astrocytoma complicated by ventricular dilatation (Figure 1). Three days post-operatively, she developed CSF rhinorrhea, the leakage was treated with closure of a small defect by artificial flap using Cadaveric fascia lata. On examination: she was afebrile (98°F); her pulse and blood pressure were 120/min and 110/60 mmHg, respectively and respiration was normal. Pupils were bilaterally of normal size and reacting. Neurological examination showed conscious child with positive neck stiffness. The other system examination was normal.
Figure 1: A 4 × 5 cm suprasellar mass is seen arising from the optic chiasm with mass effect on 3rd ventricle resulting in moderate dilatation of the lateral ventricles. Mass effect is also noted on posteriorly displaced thalami and anterior aspect of midbrain.There is bilateral optic nerve atrophy. Findings are highly suggestive of optic pathway parasitic astrocytoma.
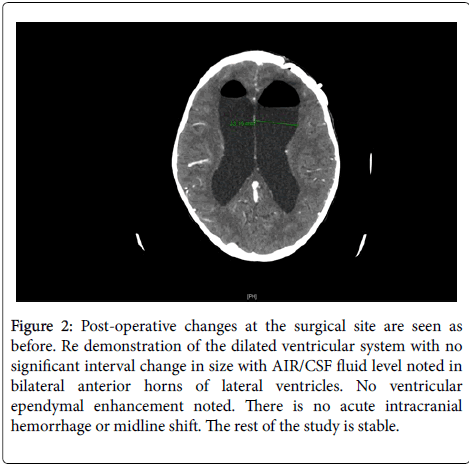
The laboratory work up included; Complete blood picture: Hemoglobin 14.5%, total leukocyte count of 4900/ cumm, neutrophils 67%, lymphocytes 24% and normal platelet number 306,000. Blood biochemistry was normal. Blood culture was negative. A contrast enhanced computed tomography (CT scan) brain scan showed dilated ventricles (Figure 2). Lumbar puncture was done and the cerebrospinal fluid (CSF) sample was evaluated for biochemistry, cell count and culture. The CSF analysis revealed WBC count of 1000 mostly polymorph (90%) and lymphocyte (10%).
Figure 2: Post-operative changes at the surgical site are seen as before. Re demonstration of the dilated ventricular system with no significant interval change in size with AIR/CSF fluid level noted in bilateral anterior horns of lateral ventricles. No ventricular ependymal enhancement noted. There is no acute intracranial hemorrhage or midline shift. The rest of the study is stable.
The CSF glucose was low 30 mg/dl with high CSF protein 28 mg/dl. Blood and CSF culture remain negative. For management of the hydrocephalus, urgent external ventricular drain (EVD) was done. Antibiotics were initiated including meropenum 40 mg/kg (intravenous every 8 hours) and vancomycin (30 mg/kg/dose intravenous every 6 hours). Two days after initiation of therapy, the fever subside down and the child resumed her activity. However daily consecutive collection of the CSF samples collected from the EVD showed persistence of high WBC count (1000-500) mostly polymorphs (80-90%) and lymphocyte (10-20%). The child was referred for evaluation by the infectious disease team. The clinical picture was suggestive of subacute meningitis and therefore the infectious disease consultant requested to send CSF specimen for fungal culture and for viral multiplex PCR including Herpes Simplex Virus (HSV) detection. Repeated CT scan brain revealed the ventricular external drain in situ and there is no evidence of pus collection or inflammation. After 3 days the CSF culture revealed growth of candida albicans sensitive to most of the antifungal drugs except for 5 flucytocin. Viral work up were negative. The patient was immediately started on Amphotericin B (5 mg/kg/day) and fluconazole (12 mg/kg/day). Daily follow up CSF analysis was done including biochemical analysis and cultures. The WBC counts were declining gradually (1000 cell to 100 then 0). The CSF protein decreased to normal level (22 mg/dl) and the CSF sugar increased gradually to normal level (40.0 mg/dl). Repeated CSF culture persistently negative. Amphotericin B and fluconazole infusions were given for a total of four weeks and the patient was continued on oral fluconazole for another two weeks. The patient was discharged in good condition to be followed up regularly in the clinic.
Discussion
The literature on central nervous system candidiasis is sparse. Most of the reported cases in pediatric age were preterm neonate, immunecompromised or develop the infection following neurosurgical procedures [1-3]. Transsphenoidal surgery is considered a safe procedure but it does carry the risks of various postoperative complications [4]. In one series, A total of 152 patients underwent sublabial transsphenoidal surgery showed different postoperative complications in which CSF leak was the commonest followed by Diabetes insipidus (DI) , Postoperative nausea/vomiting (PONV) and hematoma at operation site [5]. Jung et al and his colleague performed a literature review to study the value of Lumbar drains (LD)s in decreasing the postoperative CSF leak rates in transsphenoidal surgery and the reported perioperative complications in relation to perioperative LD insertion,they included studies with more than 100 patients, in the period from 2000 to 2012. They found that the overall incidence of postoperative CSF rhinorrhea was 1.7%. Out of 6,401 patients, 385 patients (6%) received LD to prevent postoperative CSF leak or as a therapeutic intervention [6].
Debates continue regarding the most appropriate treatment for Candida meningitis and ventriculitis. As per the Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases, initial treatment with AmB deoxycholate, 1 mg/kg intravenous daily, is recommended. An alternative regimen is liposomal AmB, 5 mg/kg daily. The addition of flucytosine, 25 mg/kg 4 times daily, may be considered as salvage therapy in patients who have not had a clinical response to initial AmB therapy, but adverse effects are frequent [7]. Our patient was managed with both Amphotercin B and intravenous Fluconazole for four weeks till all her symptoms disappeared and the CSF analysis and biochemistry normalized and the culture sterilized. Afterward, as she was clinically stable, treatment was continued with oral Fluconazole as step down therapy.
Conclusion
We believe that ,this is the first case report of successful treatment of Candida Albicans meningitis and ventriculitis post trans-sphenoidal resection. A high index of suspicion of Candida meningitis/ ventriculitis should be considered in cases of neurosurgical procedures that might cause interruption of the mucous membrane. Because of high mortality rate associated with Candida meningitis/ ventriculitis, CSF sampling for Candida culture should be considered.
References
- Taneja J, Mishra B, Thakur A, Dogra V, Loomba P (2009) Candida albicans meningitis with ventr iculitis in a four-year-old child. Neurol India 57: 682-684.
- Toprak D, ÖcalDemir S, Kadayifci KE , Türel Ö, Soysal A, et al. (2015) Recurrent Candida albicansVentriculitis Treated with Intraventricular Liposomal Amphotericin B. Case Reports in Infectious Diseases 2015: 340725.
- Ancalle IM, Rivera JA, García I, García L, Valcárcel M (2010) Candida albicans meningitis and brain abscesses in a neonate: a case report. BolAsoc Med P R 102: 45-48.
- Charalampaki P, Ayyad A, Kockro RA, Perneczky A (2009) Surgical complications after endoscopic transsphenoidal pituitary surgery. J ClinNeurosci 16: 786-789.
- Chowdhury T, Prabhakar H, Bithal PK, Schaller B, Dash HH (2014) Immediate postoperative complications in transsphenoidal pituitary surgery: A prospective study. Saudi J Anaesth 8: 335-341.
- Jung H, Shah A, Ajlan A (2014) Perioperative Cerebrospinal Fluid Diversion Utilizing Lumbar Drains in Transsphenoidal Surgery. J NeurolDisord 2: 1-6.
- Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA (2016) Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis 62: e1-e50.
--
Relevant Topics
- Advanced Therapies
- Chicken Pox
- Ciprofloxacin
- Colon Infection
- Conjunctivitis
- Herpes Virus
- HIV and AIDS Research
- Human Papilloma Virus
- Infection
- Infection in Blood
- Infections Prevention
- Infectious Diseases in Children
- Influenza
- Liver Diseases
- Respiratory Tract Infections
- T Cell Lymphomatic Virus
- Treatment for Infectious Diseases
- Viral Encephalitis
- Yeast Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 11812
- [From(publication date):
June-2016 - Jul 02, 2025] - Breakdown by view type
- HTML page views : 10880
- PDF downloads : 932