Research Article Open Access
Canadian Practice Patterns of Venous Thromboembolism Prophylaxis for Adults with Spinal Cord Injury
Ethans K1*, Deng G1, Townson A2, Jacquemin G3, Smith K4, O'Connell C4, Askari S5 and Ho C6
1Section of Physical Medicine and Rehabilitation, Department of Internal Medicine, University of Manitoba, Winnipeg, Canada.
2UBC Division of Physical Medicine and Rehabilitation, University of British Columbia, Vancouver, Canada
3Université de Montréal, Quebec, Canada.
4Dalhousie University, Stan Cassidy Centre for Rehabilitation, Canada.
5Department of Physical Medicine & Rehabilitation, Queen's University, Canada.
6Division of Physical Medicine & Rehabilitation, Department of Clinical Neurosciences, University of Calgary, Canada.
- *Corresponding Author:
- Ethans K
Section of Physical Medicine and Rehabilitation
Department of Internal Medicine
University of Manitoba, Winnipeg, Canada
Fax: 204-787-1476
E-mail: kethans@hsc.mb.ca
Received Date: April 18, 2016; Accepted Date: June 06, 2016; Published Date: June 13, 2016
Citation: Ethans K, Deng G, Townson A, Jacquemin G, Smith K, et al. (2016) Canadian Practice Patterns of Venous Thromboembolism Prophylaxis for Adults with Spinal Cord Injury. J Pediatr Neurol Disord 2:106. doi: 10.4172/2572-5203.1000106
Copyright: © 2016 Ethans K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pediatric Neurological Disorders
Abstract
Context: According to current reviews and guidelines, venous thromboembolism (VTE) prophylaxis in spinal cord injury (SCI) includes low molecular weight heparin (LMWH) in combination with mechanical prophylaxis. The level of evidence for VTE prophylaxis is varied among the recommendations. National best practice consensus is extremely important in the care of patients especially in situations when the evidence are vague and varied. Objective: To ascertain practice patterns of VTE prophylaxis by Canadian SCI rehabilitation physiatrists in adults admitted to a rehabilitation unit for spinal cord injury rehabilitation. Method: An invitation to participate in this project was distributed to Canadian SCI Rehabilitation physiatrists through the “SCI Hallways”, a private online forum for consultation between Canadian physiatrists. Results: A total of 10 physiatrists from 8 of 13 Canadian academic rehabilitation programs participated. All participants stated that their practice involved using a form of mechanical VTE prophylaxis and LMWH for 8 to 12 weeks. Conclusion: Use of VTE prophylaxis for SCI is consistent among Canadian physiatrist and matches guidelines for VTE prophylaxis in spinal cord injury.
Abstract
Context: According to current reviews and guidelines, venous thromboembolism (VTE) prophylaxis in spinal cord injury (SCI) includes low molecular weight heparin (LMWH) in combination with mechanical prophylaxis. The level of evidence for VTE prophylaxis is varied among the recommendations. National best practice consensus is extremely important in the care of patients especially in situations when the evidence are vague and varied.
Objective: To ascertain practice patterns of VTE prophylaxis by Canadian SCI rehabilitation physiatrists in adults admitted to a rehabilitation unit for spinal cord injury rehabilitation.
Method: An invitation to participate in this project was distributed to Canadian SCI Rehabilitation physiatrists through the “SCI Hallways”, a private online forum for consultation between Canadian physiatrists.
Results: A total of 10 physiatrists from 8 of 13 Canadian academic rehabilitation programs participated. All participants stated that their practice involved using a form of mechanical VTE prophylaxis and LMWH for 8 to 12 weeks.
Conclusion: Use of VTE prophylaxis for SCI is consistent among Canadian physiatrist and matches guidelines for VTE prophylaxis in spinal cord injury.
Keywords
Thromboembolism; Spinal cord injury; Prophylaxis
Introduction
Venous thromboembolism (VTE) is the third most common cause of death in people with spinal cord injury (SCI) [1]. VTE encompasses both deep vein thrombosis (DVT) and pulmonary embolism (PE). The incidence of DVT among people with SCI ranges from 49% to 100%, with the most significant risk occurring in the first two weeks postinjury [2]. Up to 50% of DVTs can lead to a PE, which is potentially life threatening. Therefore, it is vital for clinicians to implement effective prophylaxis to prevent this potentially fatal complication.
Many studies have attempted to clarify the ideal form of prophylaxis and the level of evidence for the recommendations are varied [3-5]. Current guidelines and recommendations stem from three main sources: Antithrombotic Therapy and Prevention of Thrombosis 9th edn. by the American College of Chest Physicians in 2012 (this is not specific for SCI), Spinal Cord Injury Rehabilitation Evidence (SCIRE) systematic review in the journal Archives of Physical Medicine and Rehabilitation from 2009, and the Paralyzed Veteran’s Association Guidelines from 1999 [3-5].
These three publications recommend two methods of VTE prophylaxis in people with SCI: mechanical and pharmacological [3-5] (See Table 1 for a summary of the recommendations from each publication).
| ACP 2012 | SCIRE 2009 | PVA 1999 | ||
|---|---|---|---|---|
| Pharmacological Prophylaxis | LMWH or UH (Grade 2C) | LMWH more effective than UH (Level 1a) | LMWH or UH (Level II) | |
| Duration | 3 months | Unspecified | 8-12 Weeks | |
| Mechanical Prophylaxis | Preferably IPCD (Grade 2C) | IPCD or TEDS (Level 4) | IPCD or TEDS (Level I) | |
| Duration | Unspecified | Unspecified | 2 Weeks | |
Table 1: Summary of recommendations from the three sets of recommendations for VTE prophylaxis in adults with SCI. Each journal used a different grading system for the level of evidence. In the recommendations from the American College of Chest Physicians, Grade 2C corresponds to weak recommendations based on low-quality evidence. In the recommendations from SCIRE, Level 1a evidence corresponds to data from 2 randomized control trials and Level 4 corresponds to data from pre-post study and case series. In the recommendations from PVA, Level I correspond to data from large randomized trials with definitive results, and Level II corresponds to data from small randomized trials with uncertain results.
The care of SCI patients, after their acute injury and associated surgeries, are usually under the responsibility of physiatrists. Canada is a geographically large country with multiple major rehabilitation centers spread throughout. Because of the large geographical distance between rehabilitation centers, and the variations in the level of evidence within VTE prophylaxis recommendations, a survey was conducted to assess the current Canadian practices for VTE prophylaxis for people with SCI.
Methods
The question, “What are you using for VTE and PE prophylaxis at your center?” was posted on a private online forum called “SCI Hallways” whose members consist exclusively of Canadian physiatrists engaging in SCI rehabilitation. Over the course of two weeks, various Canadian physiatrists posted their responses on the forum. The majority of the responses consisted of the specific name of the pharmacological and mechanical prophylaxis, but given the nature of using an online forum, five participants gave vague responses. These participants posted that they used an unspecified LMWH, an unspecified mechanical form of prophylaxis and or just posted “same as above”. These five participants were contacted directly via email for clarifications.
Given that there are only a handful of physiatrists involved in inpatient SCI rehabilitation, it can be difficult to organize a face-to-face meeting to discuss local practice patterns. The “SCI Hallways” is an online forum used to bridge geographical distance, allowing Canadian clinicians who treat people with SCI to engage in discussion in a convenient way. In addition to aiding in facilitating a national consensus, it has also been used regularly to assist physicians in clinical decision making and with research. Most academic Canadian physiatrists engaging in SCI rehabilitation have access to, and have previously participated on this forum. Responses can be accessed by members at any time
Results
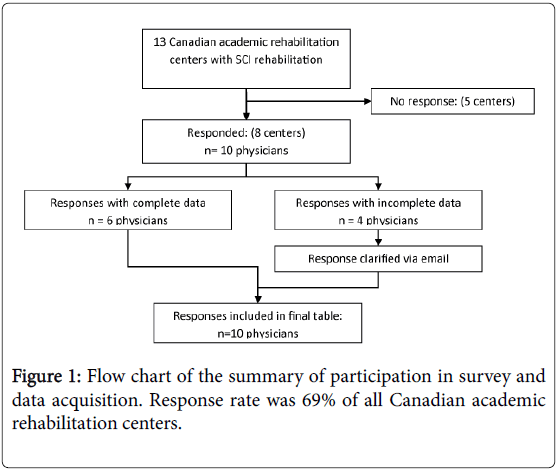
There are a total of thirteen academic centers across Canada with physicians engaging in SCI rehabilitation [6]. Some centers have dedicated SCI rehabilitation wards, while others admit patients needing SCI rehabilitation into a general rehabilitation ward. Ten physicians from eight centers participated in this practice pattern assessment. (See Figure 1 for a flow chart of the summary of participation and data acquisition).
All physicians that participated use mechanical prophylaxis. One participant did not specify the type they use. Of the other nine, one used intermittent pneumatic compression devices (IPCD) until starting LMWH and then switched to thrombo-embolic deterrent stockings (TEDS), while the other eight used TEDS with IPCD in the acute setting for up to 2 weeks and then transitioned to TEDS only (Table 2). Ideally, both IPCD and TED stockings are worn around the clock. However, certain activities cannot be done with these on, such as during maintenance of hygiene and skin integrity assessments.
| Pharmacologic Prophylaxis | Mechanical Prophylaxis | |||
|---|---|---|---|---|
| ID # | Duration | Acute Care | Rehabilitation | |
| 1 | Enoxaparin | 8-12 weeks | IPCD + TEDS for 2 weeks | TED Stocking for duration of LMWH |
| 2 | Dalteparin | 8-12 weeks | IPCD + TEDS for 2 weeks | TED Stocking for duration of LMWH |
| 3 | Dalteparin | 8-12 weeks | IPCD + TEDS for 2 weeks | TED Stocking for duration of LMWH |
| 4 | Dalteparin | 8-12 weeks | IPCD + TEDS for 2 weeks | TED Stocking for duration of LMWH |
| 5 | Dalteparin | 8-12 weeks | IPCD + TEDS for 2 weeks | TED Stocking for duration of LMWH |
| 6 | Dalteparin | 8-12 weeks | IPCD + TEDS for 2 weeks | TED Stocking for duration of LMWH |
| 7 | Dalteparin | 8-12 weeks | IPCD + TEDS for 2 weeks | TED Stocking for duration of LMWH |
| 8 | Unspecified LMWH | 8-12 weeks | IPCD + TEDS for 2 weeks | TED Stocking for duration of LMWH |
| 9 | Enoxaparin or Dalteparin | 8-12 weeks | IPCD only until LMWH started | TED Stocking for duration of LMWH |
| 10 | Unspecified LMWH | 8-12 weeks | Unspecified | Unspecified |
Table 2: Tabulated results from respondents with names substituted with identification numbers. LMWH stands for low molecular weight heparin. IPCD stands for intermittent pneumatic compression devices. TEDS stands for Thrombo-Embolic Deterrent Stockings also known as Thrombo-Embolic Deterrent Hose.
All physicians that participated use pharmacological prophylaxis with low molecular weight heparin (LMWH). Six used dalteparin exclusively, one enoxaparin exclusively, and three did not specify (Table 2).
Discussion
Relevance of guidelines
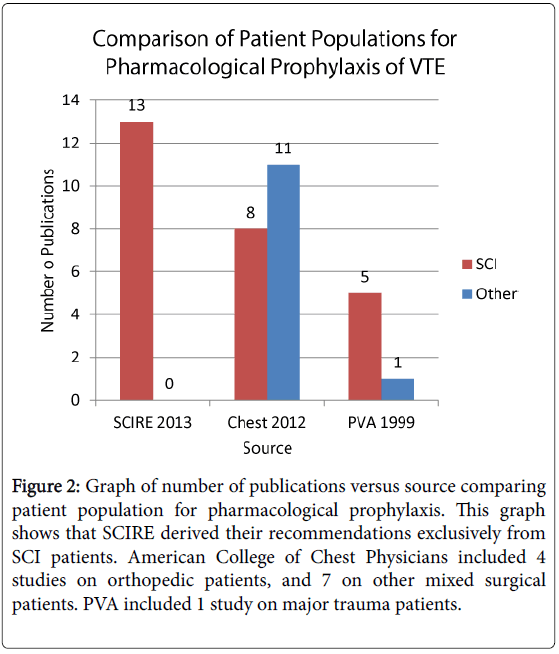
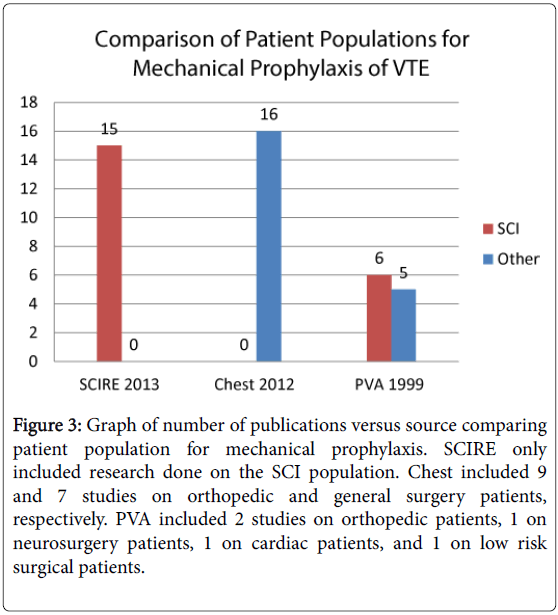
The practice patterns of Canadian SCI rehabilitation physicians reflect recommendations that state that there is evidence, although inconsistent, for both mechanical and pharmacological prophylaxis for patients with SCI [3-5]. The inconsistency may be because of the difference between the inclusion and exclusion criteria used by the authors to generate their conclusions. (See Figures 2 and 3 for comparison of patient population for pharmacologic and mechanical prophylaxis used in the three papers).
Figure 2: Graph of number of publications versus source comparing patient population for pharmacological prophylaxis. This graph shows that SCIRE derived their recommendations exclusively from SCI patients. American College of Chest Physicians included 4 studies on orthopedic patients, and 7 on other mixed surgical patients. PVA included 1 study on major trauma patients.
Figure 3: Graph of number of publications versus source comparing patient population for mechanical prophylaxis. SCIRE only included research done on the SCI population. Chest included 9 and 7 studies on orthopedic and general surgery patients, respectively. PVA included 2 studies on orthopedic patients, 1 on neurosurgery patients, 1 on cardiac patients, and 1 on low risk surgical patients.
The SCIRE recommendations published in 2009 is the most recent of the three publications and reviewed studies exclusively in the SCI patient population. The SCIRE recommendations suggest that there is strong evidence for LMWH, but poor evidence for mechanical prophylaxis [4]. The guideline from American College of Chest Physicians in 2012 is not directed at only patients with SCI, but at all non-orthopedic major trauma patients (including traumatic brain injury and spinal surgery) [5]. Additionally, the guideline from PVA (Paralyzed Veteran’s Association) in 1999 is based on research from the 1990s [3]. From our correspondence with the PVA, they have currently stopped distributing their guideline and are in the process of producing an updated guideline from more current literature.
The three guidelines and recommendations derive their conclusion from a variety of sources with minor overlap between them. For pharmacological prophylaxis, 4 studies were included in all three papers. These 4 studies were all published on or prior to 1990 [7-10]. The recommendations from the American College of Chest Physicians are derived from a total of 19 studies with 11 of the 19 studies done in the non-SCI population [5]. The recommendations from SCIRE were derived from 13 studies and the recommendations from PVA were derived from 6 studies with the newest study from 1995 [3,4].
There is even less overlap between the sources used by the major three recommendations for mechanical prophylaxis [3-5]. There are zero studies that all three recommendations cited [3-5]. The only overlap of sources occurs in the SCIRE and PVA guidelines for two studies with one done in 1982 and the other in 1992 [11,12]. Additionally, the primary sources all evaluated a vast number of interventions (including range of motion exercises, massage, bandages, rotating tables, electrical stimulation, venous foot pump, compression stockings, intermittent compression devices) and various patient populations (including SCI, general surgery, orthopedic surgery, neurosurgery, cardiac surgery and abdominal surgery) [10-39].
Mechanical prophylaxis
The options for mechanical prophylaxis includes IPCDs and TED stockings [3-5]. IPCDs are inflatable cuffs placed around the lower limbs that are intermittently inflated via an electrically powered pneumatic pump [40]. TED stockings are compression stockings with a decreasing gradient of pressure in a distal to proximal direction [40]. IPCDs simulate the actions of lower limb muscles to intermittently force the blood in the deep veins back to the heart, and TED stockings increase the velocity of blood flow and prevents the activation of extrinsic coagulation pathway from the venous distention exposing subendothelial tissue 40. One of the biggest advantages of mechanical prophylaxis is the cost effectiveness and the infrequent and minor adverse events (consisting of foot abrasions, superficial thrombophlebitis, and subjective warmth) [41].
The SCIRE review stated that there is Level 4 evidence (weak) for all forms of mechanical prophylaxis [4]. SCIRE evidence is based on two studies which although showing a positive effect for mechanical prophylaxis, were weak (a case series in 2001 and a pre-post study in 1999) [4]. The guideline from American College of Chest Physicians in 2012 stated that the evidence is grade 2C (recommendations based on low-quality evidence) [5]. American College of Chest Physician’s guideline is derived from multiple studies from major trauma patients and all were described as having various limitations [5]. The guideline from PVA in 1999 stated that the evidence is level I (data from large randomized trials with definitive results) [3]. The guidelines from PVA were based on studies from the 1970s and 1980s, including studies involving orthopedics, neurosurgery, cardiac surgery and minor surgeries, and outdated forms of mechanical prophylaxis (range of motion exercises, massage, electrical stimuli, and venous foot pump) [3].
The three recommendations had varying grades of evidence for mechanical prophylaxis [3-5]. However, the options, especially TED stockings, have mild and infrequent side effects [40]. In our study, all participants stated that SCI patients used TED stockings and IPCDs during the initial 2 weeks and continued with the TED stockings for the duration of needing LMWH.
Pharmacological Prophylaxis
The SCIRE review states that there is Level 1a evidence (strong) for LMWH being superior to unfractionated heparin (UH) and that all LMWH are equally efficacious 4. However, guidelines from American College of Chest Physicians in 2012 and from PVA in 1999 state that the evidence for pharmacological prophylaxis is not strong: Grade 2C (weak recommendations based on low-quality evidence) and Level II (data from small randomized trials with uncertain results, although this statement is relatively outdated), respectively [3,5] (Table 1). The majority of studies analyzed by the American College of Chest Physicians were in non-SCI patients and all the studies by PVA were done prior to 1995 (Table 2).
As reflected by the data, the respondents all use a variety of LMWHs. There was a variety of responses with the majority (60%) using Dalteparin. We suspect that because there is no data in literature suggesting one type of LMWH is superior to another, the rationale for choosing the specific LMWH is based on the hospital’s pharmacy formulary. Interestingly, one clinician stated that he/she choose prophylaxis based on previous experiences, and used Dalteparin for non-traumatic SCI patients and Enoxaparin for traumatic SCI patients.
Limitations of the Study
Limitations of this study include a possible reporting bias due to the transparent nature of the study design, and a selection bias due to this study being voluntary.
Additionally, the guidelines for the timeframe for VTE prophylaxis are vague or unspecified. The only recommendations for the timeline come from PVA and they suggest a total of 8-12 weeks [3]. This range means that there are four weeks of potential variability that are up to the clinician’s own discretion and interpretation of a patient’s risk for VTE.
Finally, only physiatrists participated in this study and the trauma team, surgeons, and the intensivists were not involved. Because physiatrists are predominantly involved after a patient has been stabilized in the surgical and trauma units, they are not intimately involved in the decision making process for VTE prophylaxis during a patient’s acute admission.
Conclusion
Use of pharmacological VTE prophylaxis for SCI is consistent among Canadian physiatry physicians and matches current guidelines for VTE prophylaxis in spinal cord injury. Although there is inconsistency in the level of evidence for mechanical VTE prophylaxis in current recommendations, these physicians all use mechanical VTE prophylaxis for SCI.
Acknowledgments
We would like to acknowledge Cathy Craven, Christine Short, Karen Smith, and Denise Hill for providing their center’s practice patterns for venous thromboembolism prophylaxis for spinal cord injury patients.
References
- DeVivo MJ, Krause JS, Lammertse DP (1999) Recent trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil 80: 1411-1419.
- Merli GJ, Crabbe S, Paluzzi RG, Fritz D (1993) Etiology, incidence, and prevention of deep vein thrombosis in acute spinal cord injury. Arch Phys Med Rehabil 74: 1199-1205.
- Green D, Biddle AK Fahey, V (1997) Prevention of thromboembolism in spinal cord injury. Consortium for Spinal Cord Medicine. J Spinal Cord Med 20: 259-283.
- Teasell RW, Hsieh JT, Aubut JA, Eng JJ, Krassioukov A, et al. (2009) Venous thromboembolism after spinal cord injury. Arch Phys Med Rehabil 90: 232-245.
- Gould MK, Garcia DA, Wren SM, Karanicolas PJ, Arcelus JI, et al. (2012) Prevention of VTE in nonorthopedic surgical patients: antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. Chest Journal 141: e227S-e277S.
- Program descriptions. CaRMS.
- Frisbie JH, Sasahara AA (1981) Low dose heparin prophylaxis for deep venous thrombosis in acute spinal cord injury patients: a controlled study. Paraplegia 19: 343-346.
- Green D, Lee MY, Ito VY, Cohn T, Press J, et al. (1988) Fixed- vs adjusted-dose heparin in the prophylaxis of thromboembolism in spinal cord injury. JAMA 260: 1255-1258.
- Green D, Lee MY, Lim AC, Chmiel JS, Vetter M, et al. (1990) Prevention of thromboembolism after spinal cord injury using low-molecular-weight heparin. Ann Intern Med 113: 571-574.
- Merli GJ, Herbison GJ, Ditunno JF, Weitz HH, Henzes JH, et al. (1988) Deep vein thrombosis: prophylaxis in acute spinal cord injured patients. Arch Phys Med Rehabil 69: 661-664.
- Merli GJ1 (1992) Management of deep vein thrombosis in spinal cord injury. Chest 102: 652S-657S.
- Green D, Rossi EC, Yao JS, Flinn WR, Spies SM (1982) Deep vein thrombosis in spinal cord injury: effect of prophylaxis with calf compression, aspirin, and dipyridamole. Paraplegia 20: 227-234.
- van Hove E (1978) Prevention of thrombophlebitis in spinal injury patients. Paraplegia 16: 332-335.
- Smith RC, Elton RA, Orr JD, Hart AJ, Graham IF, et al. (1978) Dextran and intermittent pneumatic compression in prevention of postoperative deep vein thrombosis: multiunit trial. Br Med J 1: 952-954.
- Barnes RW, Brand RA, Clarke W, Hartley N, Hoak JC (1978) Efficacy of graded-compression antiembolism stockings in patients undergoing total hip arthroplasty. ClinOrthop 61–67.
- Ohlund C, Fransson SG, Starck SA (1983) Calf compression for prevention of thromboembolism following hip surgery. ActaOrthopScand 54: 896-899.
- Bergqvist D, Lindblad B (1984) The thromboprophylactic effect of graded elastic compression stockings in combination with dextran 70. Arch Surg 119: 1329-1331.
- Wille-Jørgensen P, Hauch O, Dimo B, Christensen SW, Jensen R, et al. (1991) Prophylaxis of deep venous thrombosis after acute abdominal operation. SurgGynecolObstet 172: 44-48.
- Becker DM, Gonzalez M, Gentili A, Eismont F, Green BA (1987) Prevention of deep venous thrombosis in patients with acute spinal cord injuries: use of rotating treatment tables. Neurosurgery 20: 675–677.
- Salzman EW, McManama GP, Shapiro AH, Robertson LK, Donovan AS, et al. (1987) Effect of optimization of hemodynamics on fibrinolytic activity and antithrombotic efficacy of external pneumatic calf compression. Ann Surg 206: 636-641.
- Rasmussen A, Hansen PT, Lindholt J, Poulsen TD, Toftdahl DB, et al. (1988) Venous thrombosis after abdominal surgery. A comparison between subcutaneous heparin and antithrombotic stockings, or both. J Med 19: 193-201.
- Fredin H, Bergqvist D, Cederholm C, Lindblad B, Nyman U (1989) Thromboprophylaxis in hip arthroplasty. Dextran with graded compression or preoperative dextran compared in 150 patients. ActaOrthopScand 60: 678-681.
- Törngren S (1980) Low dose heparin and compression stockings in the prevention of postoperative deep venous thrombosis. Br J Surg 67: 482-484.
- Fordyce MJ, Ling RS (1992) A venous foot pump reduces thrombosis after total hip replacement. J Bone Joint Surg Br 74: 45-49.
- Wilson NV, Das SK, Kakkar VV, Maurice HD, Smibert JG, et al. (1992) Thrombo-embolic prophylaxis in total knee replacement. Evaluation of the A-V Impulse System. J Bone Joint Surg Br 74: 50-52.
- Wells PS, Lensing AW, Hirsh J (1994) Graduated compression stockings in the prevention of postoperative venous thromboembolism. A meta-analysis. Arch Intern Med 154: 67-72.
- Lieberman JR, Huo MM, Hanway J, Salvati EA, Sculco TP, et al. (1994) The prevalence of deep venous thrombosis after total hip arthroplasty with hypotensive epidural anesthesia. J Bone Joint Surg Am 76: 341-348.
- Ramos R, Salem BI, De Pawlikowski MP, Coordes C, Eisenberg S, et al. (1996) The efficacy of pneumatic compression stockings in the prevention of pulmonary embolism after cardiac surgery. Chest 109: 82-85.
- Becker DM, Gonzalez M, Gentili A, Eismont F, Green BA (1987) Prevention of deep venous thrombosis in patients with acute spinal cord injuries: use of rotating treatment tables. Neurosurgery 20: 675-677.
- Stannard JP, Harris RM, Bucknell AL, Cossi A, Ward J, et al. (1996) Prophylaxis of deep venous thrombosis after total hip arthroplasty by using intermittent compression of the plantar venous plexus. American journal of orthopedics 25: 127-134.
- Winemiller MH, Stolp-Smith KA, Silverstein MD, Therneau TM (1999) Prevention of venous thromboembolism in patients with spinal cord injury: effects of sequential pneumatic compression and heparin. J Spinal Cord Med 22: 182-191.
- Nash MS, Mintz CD, Montalvo BM, Jacobs PL (2000) A randomized blinded comparison of two methods used for venous antistasis in tetraplegia. J Spinal Cord Med 23: 221-227.
- Aito S, Pieri A, D’Andrea M, Marcelli F, Cominelli E (2002) Primary prevention of deep venous thrombosis and pulmonary embolism in acute spinal cord injured patients. Spinal Cord 40, 300–303 (2002).
- Deep K, Jigajinni MV, McLean AN, Fraser MH (2001) Prophylaxis of thromboembolism in spinal injuries--results of enoxaparin used in 276 patients. Spinal Cord 39: 88-91.
- Maxwell RA, Chavarria-Aguilar M, Cockerham WT, Lewis PL, Barker DE, et al. (2002) Routine prophylactic vena cava filtration is not indicated after acute spinal cord injury. J Trauma 52: 902-906.
- Silbersack Y, Taute BM, Hein W, Podhaisky H (2004) Prevention of deep-vein thrombosis after total hip and knee replacement. Low-molecular-weight heparin in combination with intermittent pneumatic compression. J Bone Joint Surg Br 86: 809-812.
- Eisele R, Kinzl L, Koelsch T (2007) Rapid-inflation intermittent pneumatic compression for prevention of deep venous thrombosis. J Bone Joint Surg Am 89: 1050-1056.
- Chung SB, Lee SH, Kim ES, Eoh, W (2011) Incidence of deep vein thrombosis after spinal cord injury: a prospective study in 37 consecutive patients with traumatic or nontraumatic spinal cord injury treated by mechanical prophylaxis. J Trauma 71: 867–870.
- GiorgiPierfranceschi M, Donadini MP, Dentali F, Ageno W, Marazzi M, et al. (2013) The short- and long-term risk of venous thromboembolism in patients with acute spinal cord injury: a prospective cohort study. ThrombHaemost 109: 34-38.
- Robertson L, Roche A (2013) Primary prophylaxis for venous thromboembolism in people undergoing major amputation of the lower extremity. Cochrane Database Syst Rev p: 12.
- Wade R, Sideris E, Paton F, Rice S, Palmer S, et al. (2015) Graduated compression stockings for the prevention of deep-vein thrombosis in postoperative surgical patients: a systematic review and economic model with a value of information analysis 19: 1-220.
Relevant Topics
- Behavioral Psychology
- Chiari malformation
- Chronic Traumatic Encephalopathy
- Congenital Brain Defects
- Duchenne Muscular Dystrophy
- Epilepsy and Seizures
- Genetic and Metabolic Disorders
- Genetic Epilepsies
- Headaches and Migraines
- Movement Disorders
- Neonatal encephalopathy
- Neurodevelopmental Disorders
- Neurogenetic Disorders
- Neurological Complications of AIDS
- Neuromuscular Disease
- Pediatric Brain Tumour
- Pediatric Sleep Disorders
- Stroke and Perinatal Injuries
Recommended Journals
Article Tools
Article Usage
- Total views: 21909
- [From(publication date):
December-2016 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 20926
- PDF downloads : 983