Can a Diagnosis be Ruled Out Based on One Cortisol Result? A Case Report on Delayed Diagnosis of Hypopituitarism
Received: 30-May-2015 / Accepted Date: 07-Jul-2015 / Published Date: 10-Jul-2015 DOI: 10.4172/2161-0681.1000237
Abstract
There are numerous potential causes for hyponatraemia including hypovolaemia; oedema; syndrome of inappropriate ADH secretion; and acute episodes of Addison’s disease (hypopituitarism and adrenal insufficiency) [1]. Hyponatraemia can have serious consequences for patients and there are many ways to investigate the cause. Here we present a case of an elderly patient presenting with hyponatraemia and highlight the limitations of the standard dose (250 mcg) short synacthen test (SST) for the investigation of adrenal insufficiency as a potential cause of hyponatraemia.
Introduction
There are numerous potential causes for hyponatraemia including hypovolaemia; oedema; syndrome of inappropriate ADH secretion; and acute episodes of Addison’s disease (hypopituitarism and adrenal insufficiency) [1]. Hyponatraemia can have serious consequences for patients and there are many ways to investigate the cause. Here we present a case of an elderly patient presenting with hyponatraemia and highlight the limitations of the standard dose (250 mcg) short synacthen test (SST) for the investigation of adrenal insufficiency as a potential cause of hyponatraemia.
Case Report
An 85 year old male patient arrived at Accident and Emergency in mid-2013 with presentation of general unwellness and weight loss over three months. The only significant finding on clinical examination was hypotension. Admission biochemistry results are shown in Table 1.
| Test | Result | Reference Range |
|---|---|---|
| Sodium | 128 | 133-146 nmol/L |
| Potassium | 4.6 | 3.5-5.3 nmol/L |
| Urea | 4.6 | 2.5-7.8 mmol/L |
| Creatinine | 100 | 60-120 umol/L |
| C-Reactive Protein | 85 | 0-10 mg/L |
| Haemoglobin | 130 | 130-180 g/L |
Table 1: Admission biochemistry results.
The patient was admitted to the acute medical unit for the investigations of hyponatraemia. 9am cortisol was measured and reported as 81 nmol/L (138 to 620 nmol/L). The low cortisol result prompted clinicians to perform a standard dose SST to investigate adrenal insufficiency. Baseline cortisol was 239 nmol/L and 30 minute cortisol increased to 504 nmol/L. It was thought that thirty minute post synacthen cortisol>500 nmol/L would rule out significant hypocortisolism [2,3]. The patient was monitored and discharged a week later following improvements in biochemistry results. There was no documented cause for the hyponatraemia seen at this time.
The patient continued to be monitored in primary care over the following months with continued weight loss and anaemia. The biochemistry tests requested gave little indication of abnormality in the patient, but his haemoglobin was generally slightly lower than reference intervals. In early 2014 GP requested tests revealed sodium 128 nmol/L and potassium 4.2 nmol/L; thyroid stimulating hormone (TSH) of 4.9 miu/L (0.30-5.00) and free thyroxine 4 (fT4) of 6.5 pmol/L (9.0-25.0). The TSH was inappropriately low for the level of fT4 so a pituitary screen was added by the duty biochemist (Table 2).
| Test | Result | Reference Range |
|---|---|---|
| TSH | 4.9 | 0.30-5.0 miu/L |
| fT4 | 6.5 | 9.0-25.0 pmol/L |
| Prolactin | 404 | 50-400 miu/L |
| Luteinising Hormone | <0.5 | 1.0-10.0 iu/L |
| Follicle Stimulating Hormone | 1.1 | 1.0-10.0 iu/L |
| Testosterone | <3.0 | 9.4-37 nmol/L |
| Cortisol | 41 nmol/L | (11:29am) |
Table 2: Results from Pituitary screen.
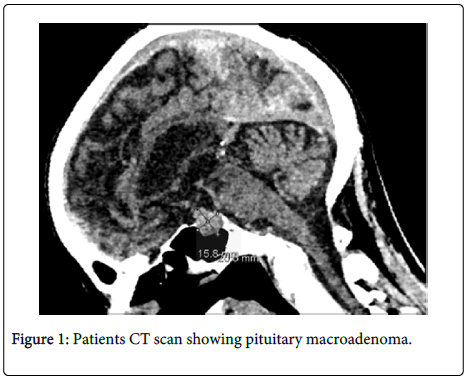
Around this time the patient was also investigated for memory loss and confusion by computed tomography (CT) scan of the brain which showed pituitary adenoma measuring 20 mm by 15 mm with expansion to sella (Figure 1). The patient was referred to an endocrinologist for further management and prescribed hydrocortisone and levothyroxine replacement. His notes document clear improvements in his outward health and well-being and note that he bounded into his follow-up consultation after replacement therapy.
Case Discussion
SST can be performed using low dose (1 mcg) synacthen or standard dose (250 mcg) synacthen. The standard dose SST is supraphysiological and known to transiently increase plasma cortisol in patients with documented secondary adrenal insufficiency [3]. Additionally, in patients with recent onset hypopituitarism, adrenal glands may not be sufficiently atrophic to indicate presence of disease and give measureable 30 minute cortisol greater than the clinical cut-offs [4]. At cortisol levels>500 nmol/L the standard dose SST has 95% specificity and 97.5% selectivity for primary adrenal insufficiency but is less sensitive for secondary adrenal insufficiency (57%). Therefore, whilst an abnormal response has a high predictive probability for primary adrenal insufficiency, a normal 30 minute response may not completely exclude secondary adrenal insufficiency (hypopituitarism) [5].
Another consideration when interpreting results for measurement of steroid hormones is analytical imprecision. The analytical coefficient of variation for this assay in the laboratory is between 5 and 10%.
This case provides an example where cortisol results near clinical cut-offs should have been interpreted with caution. It highlights how understanding the performance characteristics of the analytical methods used to generate results and the limitations of clinical investigations should be considered when interpreting a result. This case demonstrates that a single stress test cortisol result may not be sufficient to make or rule out a diagnosis and other biochemical tests or clinical investigations maybe required.
References
- Diederich S, Franzen NF, Bähr V, Oelkers W (2003) Severe hyponatremia due to hypopituitarism with adrenal insufficiency: report on 28 cases. Eur J Endocrinol148: 609-617.
- Ferrante E, Morelli V, Giavoli C, Mantovani G, Verrua E, et al. (2012) Is the 250 µg ACTH test a useful tool for the diagnosis of central hypoadrenalism in adult patients with pituitary disorders? Hormones 11:428-435.
- Thaler LM, Blevins LS Jr (1998) The low dose (1-microg) adrenocorticotropin stimulation test in the evaluation of patients with suspected central adrenal insufficiency. J ClinEndocrinolMetab83:2726-2729.
- Streeten DH, Anderson GH, Bonaventura MM (1996) The potential for serious consequences from misinterpreting normal responses to the rapid adrenocorticotropin test. J ClinEndocrinolMetab 81:285-290.
- Dorin RI, Qualls CR, Crapo LM (2003) Diagnosis of adrenal insufficiency. Ann Intern Med 139: 194.
Citation: James P, Gupta P, Patel P (2015) Can a Diagnosis be Ruled Out Based on One Cortisol Result? A Case Report on Delayed Diagnosis of Hypopituitarism. J Clin Exp Pathol 5:237. DOI: 10.4172/2161-0681.1000237
Copyright: © 2015 James P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 14695
- [From(publication date): 8-2015 - Dec 19, 2024]
- Breakdown by view type
- HTML page views: 10269
- PDF downloads: 4426