Calculating Additional Risk of Concomitant Laparoscopic Surgery in Living Kidney Donors: Cholecystectomy in Combination with Living Donor Nephrectomy
Received: 27-Jan-2016 / Accepted Date: 03-May-2016 / Published Date: 09-May-2016 DOI: 10.4172/2475-7640.1000102
Abstract
Background: During the evaluation of a donor candidate for living kidney donation, occasionally a concomitant benign abdominal disease is diagnosed. Combining organ donation and surgical treatment of that disease could be beneficial to the donor. This paper quantified the additional risk to the donor if the two operations were combined. Study design: The clinical database of 155 academic medical centers and affiliated hospitals of University HealthSystem Consortium was used to predict the minimum expected surgical risk of a combined laparoscopic cholecystectomy and laparoscopic donor nephrectomy. Results: Our model predicted that a minimum of 8.64% of patients undergoing laparoscopic cholecystectomy at the same time as a donor nephrectomy would experience at least one complication. This represents an increase of 2.3% (relative risk=1.24) from the 6.34% risk for patients undergoing only the cholecystectomy. Conclusion: The estimation of increased risk is a necessary step to obtain informed consent from a donor offered or who wants to undergo multiple procedures simultaneously.
Keywords: Cholecystectomy; Decision analysis model; Living donor kidney transplantation; Nephrectomy; Relative risks; Risk assessment model; Surgical complications
7506Abbreviations
UHC: University Health System Consortium
Introduction
Each year in the United States approximately 6000 laparoscopic donor nephrectomies are performed. Donor selection criteria have become less strict, and now candidates with hypertension and obesity are considered. Even prior abdominal surgery is not an absolute contraindication to donation. In the evaluation process, it is not uncommon to discover a benign intraabdominal disease process that requires surgical treatment, such as cholelithiasis, ovarian cysts, or abdominal hernias. There may be patients with cholelithiasis who are in need of an elective laparoscopic cholecystectomy but may wish to become an altruistic donor. Although these benign pathologies could be easily addressed at the same time as the laparoscopic nephrectomy, consideration must be given to the additional risk the donor faces with multiple procedures.
Although many transplant surgeons may have performed combined laparoscopic procedures during the donor nephrectomy such as: cholecystectomy, hepatic wedge resection or hernia repair, there has been very little published in this area except for case reports and small series [1-3]. Previous case series have not addressed the risk of particular combined procedures in combination with donor nephrectomy, or have considered renal surgery but not donor nephrectomy in particular [1-3]. A proper assessment of the risk of any surgery is a necessary step in obtaining informed consent, and this is especially true for donor operations. The surgeon encountering a potential donor with a concomitant surgical problem that could be treated at the same time as the laparoscopic nephrectomy should be able to provide an estimate of the aggregate risk of a combined operation. For this reason, we constructed a theoretical risk assessment model that would provide an accurate calculation of the risks associated with combined laparoscopic procedures performed in conjunction with donor nephrectomy.
In this paper, we used a decision analysis model to analyze the minimum estimated complication risk of kidney donation when combined with laparoscopic cholecystectomy. By comparing our estimate to the complication risk of a normal laparoscopic cholecystectomy, we can extrapolate an estimate of the “donation risk” for a combined laparoscopic cholecystectomy and donor nephrectomy [4].
The analysis presented in this paper provides a reasonably accurate estimation of the minimum expected risk of combining a laparoscopic kidney donation with a cholecystectomy. The estimation of the increased risk is necessary information for the donor candidate who is deciding whether to consent to a combined procedure. In the short term, there are a variety of surgical complications associated with donor nephrectomy [5-9]. Our analysis is limited to consideration of these short-term surgical risks, and their interplay with simultaneous procedures.
Materials and Methods
Patient identification
Patient information was collected from the UHC clinical database, which contains patient records from 155 hospitals located in 40 states. The hospitals included are diverse with respect to size (number of licensed beds ranging from 16 to 1156), academic affiliation (68% university based), and geography (Southeast, Mid-Atlantic, Mid- Continent, Midwest, West, New England). A retrospective analysis was performed between 2002 to 2008 comprising 21,769,201 hospital discharges.
We identified two distinct patient groups using ICD-9 codes for the time period 2002 to 2008. The first group was the laparoscopic cholecystectomy group (n=107,561 patients) with only the single procedure code 51.23 during the time of hospitalization. Similarly, we identified the living laparoscopic donor nephrectomy group by including patients who had the procedure codes 54.21 (laparoscopy), 55.51 (nephroureterectomy), and v59.4 (kidney donor) (n=4,762 patients).
A subset of patients from the laparoscopic cholecystectomy group who were between the ages of 18 and 64 was defined. From this age subset, we excluded laparoscopic cholecystectomy patients who had diagnoses that were contraindications to laparoscopic donor nephrectomy for donation in order to include only those patients who would be considered healthy enough to donate a kidney. Specifically, we excluded mental disorders (ICD-9 290-319), chronic obstructive pulmonary disease and allied conditions (ICD-9 490-496), neoplasms (ICD-9 140-239), end-stage renal disease (ICD-9 585.1-585.6), and diabetes (ICD-9 249-250.9). A total of 50,567 patients were considered eligible to undergo combined laparoscopic cholecystectomy and nephrectomy.
Outcome measures
For the eligible laparoscopic cholecystectomy and laparoscopic donor nephrectomy groups, we collected detailed complication data, readmission rates, and reoperation rates. The detailed complication data were broken into categories by the UHC complication profiler. This profiler is used to identify potentially avoidable complications that were not present at the time of admission. The UHC compilation profiler applies research originally conducted at Beth Israel Hospital in Boston, Massachusetts, and funded by the Agency for Health Care Policy and Research, through which Dr. Lisa Iezzoni and colleagues found that quality screening using computers can be performed using ICD-9-CM codes from standard administrative databases. The complication profiler screens for 25 potentially avoidable complications (categories) based on the patient’s procedures and diagnoses. Two of these categories are “miscellaneous complications” and “other complications,” which represent instances where the ICD- 9 coding fails to fit into the 23 defined categories. A single patient can experience more than one complication type; the value reported for each complication is the absolute probability of that particular complication occurring.
Results
Basic outcomes data
Patients undergoing laparoscopic cholecystectomy alone had a 6.34% complication rate, and a 2.21% 30 day readmission rate (Table 1). In comparison, patients undergoing laparoscopic donor nephrectomy had an increased complication rate of 7.45%, and a decreased readmission rate of 1.22%.
| ICD-9 procedure/diagnosis codes | Complication(s) | 30-day related readmission | Conversion to open |
|---|---|---|---|
| 51.23: laparoscopic cholecystectomy (N=50,567) | 6.34% | 2.21% | 0.2% |
| 55.51: nephroureterectomy + 54.21: laparoscopy + V59.4: kidney donor (N=4762) |
7.45% | 1.22% | 0.11% |
| Difference, absolute value (95% confidence interval) |
1.12%* (0.43, 1.88) |
0.99%* (0.56, 1.42) |
0.09% (–0.03, 0.22) |
*Statistically significant
Table 1: Rates for complications, readmission, and conversion to an open procedure for laparoscopic cholecystectomy and laparoscopic donor nephrectomy.
Model development
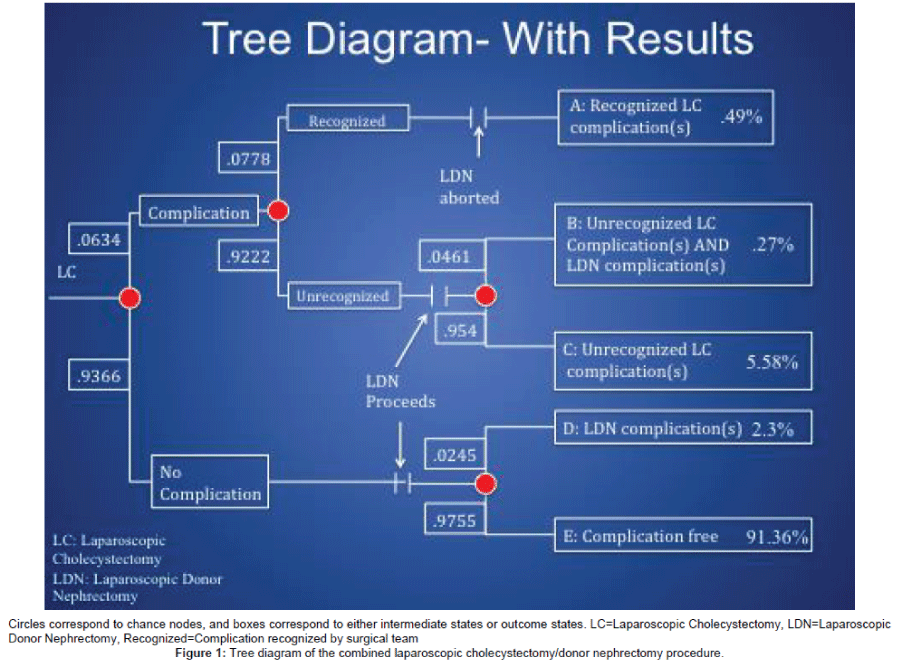
Modeling a theoretical dual procedure like the one proposed is possible using decision analysis techniques [3]. The combined surgical procedure would have two distinct steps. First, the laparoscopic cholecystectomy would be performed. Since the existing cholelithiasis either was symptomatic or could become symptomatic in the near future, thus requiring surgical attention, treating the existing pathology took precedence over the donation. After the laparoscopic cholecystectomy was performed, the patient’s condition would be assessed. If the patient suffered a complication or was compromised in any way, the donor nephrectomy would be aborted. If no complication was found, the donor nephrectomy would be performed as planned. In the tree diagram representation of the proposed procedure (Figure 1), the model has 52 inputs, 4 chance nodes, and 5 outcome states. The probabilities associated with each of the four nodes were as follows: one or more complications during laparoscopic cholecystectomy, .0634; intraoperative recognition of a laparoscopic cholecystectomy complication, 0.0778; one or more additional complications during donor nephrectomy if a patient suffered a complication during the cholecystectomy, 0.0461; one or more complications during donor nephrectomy if the patient did not suffer a complication during the cholecystectomy, 0.0245 (Appendix).
The “ideal case” approximation of the additional risk of donation
The critical assumption in this model was the approximation of the risk of continuing with the donor nephrectomy after having completed the cholecystectomy. Clearly, this risk was greater than zero, as the patient was being subjected to additional time under anesthesia, new port incisions, and the actions involved with the nephrectomy itself (e.g. dissection of the renal vasculature and the ureter, removal of the kidney). To approximate this risk as an increase in the probability of suffering one or more complications, we classified the 25 UHC complication categories into two groups based on their relative occurrence in laparoscopic cholecystectomy and laparoscopic donor nephrectomy. If the complication occurred more often in laparoscopic cholecystectomy than in donor nephrectomy, we assumed that the additional risk of that complication occurring in the combined procedure was zero. If the complication occurred more often in donor nephrectomy, we assumed that this led to an “additional risk” to the patient of a value such that the patient’s total probability of suffering the complication was equal to the probability of it occurring in normal donor nephrectomy. In other words, in our model, a combined laparoscopic cholecystectomy and donor nephrectomy increased the patient’s probability of suffering any particular complication to the probability of that complication occurring in donor nephrectomy alone. These assumptions defined the minimum probability of each complication occurring during the donor nephrectomy component of the dual procedure. This concept is represented in equation form as follows:
RA i ≥ 0 if Ci>Ni
RA i ≥ Ni - Ci if Ni>Ci
Where Ni=The probability complication i occurs during a normal laparoscopic donor nephrectomy, Ci=The probability complication i occurs during a normal laparoscopic cholecystectomy; and RAi=The probability complication i occurs during the laparoscopic donor nephrectomy portion of a combined laparoscopic cholecystectomy and donor nephrectomy. In this derivation, we kept only first-order terms (Appendix, Table 2).
| Complication | Recognized by surgical team? | Complication rate | ||
|---|---|---|---|---|
| Donor nephrectomy | Chole-cystectomy | Additional risk from donor nephrectomy | ||
| Aspiration pneumonia | No | 0% | 0.08% | 0% |
| Cellulitis or decubitus ulcer | No | 0% | 0.04% | 0% |
| Central or peripheral nervous system | No | 0.02% | 0.02% | 0% |
| Mechanical complication due to device or implant | Yes | 0.06% | 0.26% | 0% |
| Miscellaneous complications | No | 0.94% | 0.69% | 0.25% |
| Other complications of procedures | No | 4.43% | 2.88% | 1.55% |
| Post procedure hemorrhage or hematoma | No | 1.18% | 0.83% | 0.35% |
| Post/intraoperative shock due to anesthesia | No | 0.02% | 0% | 0.02% |
| Postoperative AMI | No | 0% | 0.05% | 0% |
| Postoperative GI hemorrhage or ulceration | No | 0% | 0.02% | 0% |
| Postoperative cardiac abnormality except AMI | No | 0.02% | 0.02% | 0% |
| Postoperative coma or stupor | No | 0% | 0.01% | 0% |
| Postoperative infections, not pneumonia/wound | No | 0% | 0.09% | 0% |
| Postoperative physical and metabolic derangements | No | 0.04% | 0.05% | 0% |
| Postoperative pneumonia | No | 0.40% | 0.17% | 0.23% |
| Postoperative pulmonary compromise | No | 0.25% | 0.42% | 0% |
| Postoperative urinary tract complication | No | 0% | 0.05% | 0% |
| Postoperative stroke | No | 0% | 0.01% | 0% |
| Procedure-related perforations or lacerations | Yes | 0.78% | 1.23% | 0% |
| Reopening of surgical site | Yes | 0.08% | 0.08% | 0% |
| Septicemia | No | 0.04% | 0% | 0.04% |
| Shock or cardiorespiratory arrest | Yes | 0% | 0.01% | 0% |
| Venous thrombosis/pulmonary embolism | No | 0.04% | 0.25% | 0% |
| Other complications related to anesthesia agents/CNS agents | No | 0% | 0% | 0% |
AMI=Acute Myocardial Infarction; GI=Gastrointestinal; CNS=Central Nervous System
Table 2: Complication rate for laparoscopic cholecystectomy, laparoscopic donor nephrectomy, and the additional risk from donor nephrectomy when added to cholecystectomy.
We also addressed the scenario of a patient having a complication during the cholecystectomy that went undetected by the surgical team. The data indicated that the probability of experiencing a second complication during either procedure was greater than the first (i.e., the first complication predisposed the patient to the second). Analyzing the data, we determined that the second complication was roughly 1.89 times more likely to occur than the first (Appendix) and therefore we weighted the probability of a second complication occurring based on these data.
Outcomes of a combined laparoscopic cholecystectomy/ nephrectomy
Generally, the patient would have an 8.64% chance of experiencing at least one complication (i.e., being in outcome states A-D). Compared with the probability of experiencing at least one complication in normal laparoscopic cholecystectomy (6.34%), performing the donor nephrectomy led to a minimum absolute increase of 2.3% (relative risk=1.24) in the chance that the patient would experience at least one complication (Table 3 and Figure 1).
| Outcome state | % of overall |
|---|---|
| A: Recognized cholecystectomy complication(s) | 0.49% |
| B: Unrecognized cholecystectomy complication(s) plus donor nephrectomy complication(s) | 0.27% |
| C: Unrecognized cholecystectomy complication(s) | 5.58% |
| D: Donor nephrectomy complication(s) | 2.3% |
| E: No complications | 91.36% |
Table 3: Probability of complications determined by risk assessment model.
Comparison of donation risks
The results as presented in Table 3 are useful in informing patients who are considering a combined laparoscopic cholecystectomy and donor nephrectomy. The risk of a laparoscopic cholecystectomy and laparoscopic donor nephrectomy need to be compared to demonstrate the risk profile for the dual procedure. Therefore, we created two broad outcome categories, assumed risk and donation risk. The assumed risk category contains both of the outcome states (A and C in Table 3) related only to complications from the cholecystectomy portion of the procedure. This category captures those patients who experienced no additional complications from nephrectomy, so therefore, the probabilities of these two states can be said to constitute the risk the patients elected to take on when they chose to get a laparoscopic cholecystectomy. The donation risk category contains the risks that were not part of the risk profile for laparoscopic cholecystectomy, where patients experienced a complication during the nephrectomy portion of the procedure (outcome states B and D, Table 3). This represents the accumulated risk the patients accepted when choosing to donate their kidney in the dual procedure.
In comparing the risk of the proposed operation to a typical laparoscopic donor nephrectomy, it is appropriate to use the donation risk category. The donation risk category contains only the states that are not part of the risk profile of a laparoscopic cholecystectomy, so it can be thought of as the “cost of donation,” or the accumulated risk of donor nephrectomy. The donation risk is equal to a 2.57% increase in the probability of one or more complications occurring. In normal laparoscopic donor nephrectomy, the donor has a 7.45% chance of suffering one or more complications. Therefore, we have predicted that the probability of one or more complications will be relatively smaller in the dual procedure than if a donor underwent surgery solely for the purpose of donation (7.45%) (Table 4).
| Variable | Risk of complications |
|---|---|
| Laparoscopic cholecystectomy only | 6.07% |
| Laparoscopic donor nephrectomy only | 7.45% |
| Cost of donation: Additional risks from nephrectomy beyond those for cholecystectomy | 2.57% |
| Risk reduction to society from combining procedures | 4.88% |
Table 4: Summary of risk for simultaneous cholecystectomy and donor nephrectomy procedures.
Sensitivity analysis
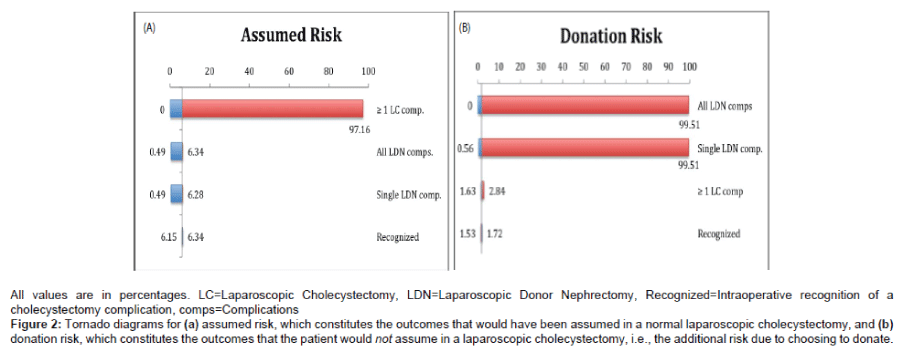
Because the model has 52 inputs, we performed one-way sensitivity analysis for both donation risk and assumed risk using only four critical inputs: 1) Probability of experiencing one or more complication in laparoscopic cholecystectomy, 2) Probability of recognizing a laparoscopic cholecystectomy complication, 3) Probability of a single additional complication during the donor nephrectomy, and 4) Probability of getting all 25 complications during the donor nephrectomy. We chose postoperative/intraoperative shock due to anesthesia for our single complication, as it had the greatest additional risk of occurring out of all 25 categories. Setting the probability of getting all 25 complication categories to the same value generated the all laparoscopic donor nephrectomy complications category.
Two tornado diagrams were constructed displaying the effect size of each of the 4 input categories on the 2 risk categories (Figures 2A and 2B). For the assumed risk outcome category, the probability of experiencing one or more complications during the laparoscopic cholecystectomy had the greatest magnitude of effect. For the donation risk category, the two additional donor nephrectomy complication input categories were by far the largest in effect. The probability of experiencing one or more laparoscopic cholecystectomy complications had a small positive effect due to the fact that the probability of outcome state B (i.e., unrecognized cholecystectomy complication and nephrectomy complication) increases. It is important to note that the ability to recognize complications did not have a substantial impact on the probability the patient ended up in the donation risk category.
Figure 2: Tornado diagrams for (a) assumed risk, which constitutes the outcomes that would have been assumed in a normal laparoscopic cholecystectomy, and (b) donation risk, which constitutes the outcomes that the patient would not assume in a laparoscopic cholecystectomy, i.e., the additional risk due to choosing to donate.
Discussion
Implications of combined laparoscopic cholecystectomy/ nephrectomy
The performance of simultaneous procedures during surgery and the risk of their concomitant performance have been extensively examined by various surgical fields. The risk of undergoing multiple laparoscopic procedures, such as a laparoscopic cholecystectomy in combination with an additional procedure has been shown to have minimal effects on the duration of the procedure and no effects in regards to length of hospital stay or patient post- operative course [1]. It has been encouraged to perform concurrent elective abdominal surgical procedures without posing additional risk to the patient. However, there is minimal information available in regards to the risk profile posed to the living kidney donors undergoing additional elective procedures at the time of kidney donation.
Previously conducted studies regarding the topic of concomitant elective procedures with laparoscopic nephrectomies have been limited due to the low number of patients involved in the case series, and inability to suitably define the additional risk posed to the donor. Tsivian et al. [2] retrospectively reviewed 19 patients who underwent a laparoscopic renal procedure (5 partial nephrectomies, 12 radical nephrectomies, 2 simple nephrectomies) in combination with a laparoscopic cholecystectomy. The duration of the combined procedure was minimally extended with no immediate complications, and no extension of hospital stay. Molmenti et al. [3] performed a prospective study of 321 patients undergoing living donor nephrectomy, with only 5 of these patients having concomitant elective procedures performed at the time of donation (2 laparoscopic adrenalectomies, 1 colposuspension, 1 laparoscopic cholecystectomy, 1 liver biopsy). No complications, acute or chronic, were noted in these case series. While these studies do reinforce that combined laparoscopic nephrectomy and additional laparoscopic procedures can be performed safely and efficaciously, a statistical figure for the additional risk posed to these patients attributed to the additional procedures performed could not be characterized.
This analysis provides a clear theoretical risk profile that a donor candidate with benign, moderately symptomatic cholelithiasis will face if he or she elects to undergo a combined laparoscopic cholecystectomy and donor nephrectomy. The data record from the UHC clinical database demonstrates that the minimum increased risk to a donor is less than 3% when undergoing a combined procedure. Any informed consent process could now offer a clearer description of the risk of the combined procedure in comparison to the cholecystectomy alone.
The result of our analysis serves two purposes. First, it is critical to explain to patients the relative magnitude of the risk profile. Second, although the analysis was conducted in a retrospective manner, it provides the donor surgeon and the community at large the ability to evaluate the risk profile of patients undergoing cholecystectomy alone, or a combined procedure. Risk is a difficult concept to explain to the donor, but must remain the central focus of any informed consent discussion. The consent process is clearly improved if the surgeon and the donor advocate team are able to quantify the risk profile and determine the difference between undergoing an individual operative procedure alone versus a combined procedure. One may argue that once the benign pathology is diagnosed, treatment should take precedence over the donation, and the donation should be performed at a later date. On the other hand, one may argue that since the discovered disease is indeed benign, and consequently donation should take place, and the donor may or may not address the other pathology at a later date. This would result in the potential need to repeat the preoperative workup, consecutive procedures, and undergoing multiple general anesthetics. It is not easy to quantify whether the risk profile is higher with a combined procedure versus multiple procedures in succession, but the results of our analysis indicate that it is likely that the burden on the donor is greater with sequential procedures.
An indirect but interesting aspect of this risk model is that the donor who has been diagnosed with cholelithiasis now has a clear indication for surgery rather than being “only” a donor. The need for the laparoscopic cholecystectomy creates a situation where the risks of the donation are now partially absorbed in the risks of the cholecystectomy. The model we constructed suggests that for this donor, the so-called “cost of donation” will be of a risk profile than those undergoing a laparoscopic nephrectomy only (Table 4).
Limitations
This model estimates a risk profile and is not designed to have the same clinical predictive power as a surgical risk calculator [8]. Our prediction of an 8.64% probability of experiencing one or more complications is a minimum estimate of complications in a combined procedure and is not equivalent to a complete description of the risk of an established procedure [8]. However, we believe the assumptions made in our model have a basis in surgical reality. If one of these procedures was a surgery requiring anastomoses or other constructive surgery, the increased time on the operating table could be expected to greatly increase the risk package of a dual procedure. Since both cholecystectomy and nephrectomy involve the removal of tissue, the increased operative time may have less of an effect, and our minimal risk package estimate may be more accurate. Finally, the estimate serves mainly to demonstrate the potential benefit in general of combining multiple procedures and the ultimate risk profile of the combined operation will be determined by the complication rates of the individual institutions.
Furthermore, while the difference in probability of experiencing complications between a laparoscopic cholecystectomy and a laparoscopic donor nephrectomy (Table 1) was statistically significant, the differences between each of the 25 complication categories were not. However, by taking the maximum of these two values, we limit the degree to which we could be potentially underestimating the risk by the variability in the larger of the two.
We believe that our results estimate the minimum risk, or risk profile, for a donor undergoing a combined laparoscopic donor nephrectomy and cholecystectomy. While there is an increase of risk to the donor who decides to undergo a combined procedure, we believe that performing a combined procedure has a more beneficial risk profile than sequential procedures. Furthermore, we believe that the results of our analysis will improve the understanding of the risks of combining living kidney donation with a laparoscopic cholecystectomy and thus may improve the donor informed consent process.
Acknowledgement
The authors would like to acknowledge Nathan Cook, PhD candidate in physics at the State University of New York at Stonybrook, for his assistance in defining the third chance node probability. The authors also acknowledge David Blair, MD/PhD candidate, and Matt Nolan, MD candidate at the University of Chicago, for their editing.
References
- Nichitailo ME, Skums VV, Diachenko AN, Litvinenko AN, Ogorodnik PV, et al. (2004)Simultaneous operations during laparoscopic cholecystectomy. Klin Khir 2: 5-7.
- Tsivian A, Konstantinovsky A, Tsivian M (2009) Concomitant laparoscopic renal surgery and cholecystectomy: outcomes and technical considerations. J Endourol 23: 1839-1842.
- Molmenti E, Pinto P, Montogomery R, Li-Ming S, Kraus E, et al.(2003) Concomitant surgery with laparoscopic live donor nephrectomy. Am J Transplant 3: 219-223.
- Sonnenberg FA, Beck JR (1993) Markov models in medical decision making: a practical guide. Med Decis Making 13: 322-328.
- Vollmer CM Jr, Callery MP (2007) Biliary injury following laparoscopic cholecystectomy: Why still a problem? Gastroenterology 133: 1039-1041.
- Ibrahim HN, Foley R, Tan L, Rogers T, Bailey RF, et al. (2009) Long-term consequences of kidney donation. N Engl J Med 360: 459-469.
- Muzaale AD, Massie AB, Wang MC, Montgomery RA, McBride MA, et al. (2014) Risk of end-stage renal disease following live kidney donation. JAMA 311: 579-586.
- Hadjianastassiou VG, Johnson RJ, Rudge CJ, Mamode N (2007) 2509 living donor nephrectomies, morbidity and mortality, including the UK introduction of laparoscopic donor surgery. Am J Transplant 7: 2532-2537.
- Cohen ME, Bilimoria KY, Ko CY, Hall BL (2009) Development of an American College of Surgeons national surgery quality improvement program: morbidity and mortality risk calculator for colorectal surgery. J Am Coll Surg 208: 1009-1016.
Citation: Parker WF, Siegler M, Angelos P, Fernandez H, Medvedev S, et al. (2016) Calculating Additional Risk of Concomitant Laparoscopic Surgery in Living Kidney Donors: Cholecystectomy in Combination with Living Donor Nephrectomy. J Clin Exp Transplant 1: 102. DOI: 10.4172/2475-7640.1000102
Copyright: © 2016 Parker WF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 13526
- [From(publication date): 7-2016 - Apr 08, 2025]
- Breakdown by view type
- HTML page views: 12627
- PDF downloads: 899