Research Article Open Access
Calcifying Tendonitis of the Shoulder: Risk Factors and Effectiveness of Physical Therapy
Marcos Edgar Fernández-Cuadros1,2,*, Olga Susana Pérez-Moro1, Javier Nieto-Blasco3, Victoria Rivera-García3, Adela Olazar-Pardeiro3and Jose Antonio Mirón-Canelo41Department of Rehabilitation, Santa Cristina's University Hospital, Madrid, Spain
2Santisima Trinidad Foundation’s Hospital, Salamanca, Spain
3Department of Rehabilitation, Salamanca's University Complex, Salamanca, Spain
4Department of Preventive Medicine and Public Health. University of Salamanca, Spain
- *Corresponding Author:
- Marcos Edgar Fernández-Cuadros
Hospital Universitario Santa Cristina
Madrid, España, Calle del Maestro
Vives 2 y 3, Spain
Tel: 0034620314558
E-mail: marcosefc@hotmail.com
Received date: October 10, 2015; Accepted date: November 16, 2015; Published date: November 23, 2015
Citation: Fernández-Cuadros ME, Pérez-Moro OS, Nieto-Blasco J, Rivera-García V, Olazar-Pardeiro A, et al.(2015) Calcifying Tendonitis of the Shoulder: Risk Factors and Effectiveness of Physical Therapy". Occup Med Health Aff 3:220. doi: 10.4172/2329-6879.1000220
Copyright: © 2015 Fernández-Cuadros ME, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Occupational Medicine & Health Affairs
Abstract
The aim of this study is to determine the different risk factors associated with Calcifying tendonitis (CT), to characterize it epidemiological-clinical-radiological, in a number of cases, and to assess the effect of physical therapy in improving mobility and decreasing pain.
A prospective experimental intervention to a series of 50 patients (40 experimental group and 10 control group) diagnosed of CT referred to the Rehabilitation Department of the University Welfare Complex of Salamanca was performed, during October 2011 to February 2013.
In the initial assessment the demographics, personal history, predisposing factors and type of calcification (formative/resorptive), were collected. The evaluation of the shoulder Range of Movement (initial ROM) was performed. Pain was valued according to visual analog scale (initial VAS). The intervention consisted in prescribing Kinesiotherapy (KT) (if restricted mobility) or various electrotherapy modalities (US ultrasound, TENS, Microwave MW, Shortwave SW, Interferential IF) (if pain). In the final evaluation mobility (final ROM) and pain (final VAS) was re-evaluated, in addition to the global patient satisfaction. CT is more common in women (n=36; 72%) than in men (n=14; 28%) (p=0.00). The CT occurs in middle age/working life (53.96 years, SD=±11.99). The most common occupation were housekeeper and assistant. They presented forced postures, repetitive movements and cargo handling. CT prevailed in right shoulders (n=33; 66%), in the SE tendon (n=46; 92%) and all patients had radiological, ultrasound (n=24; 48%) and MRI (n=8; 16%) evaluation. Most patients had formative (n=38; 76%) rather than resorptive calcifications (n=12; 24%) (p=0.00). The average number of rehabilitation sessions was 28.6 ± 12.9 days. VAS diminished from 5.96 to 3.26 points after kinesiotherapy/electrotherapy treatment. KT treatment recovers ROM significantly (p<0.05). Resorptive calcifications had more chronic pain. The treatment group decreased VAS significantly (p=0.00) from 5.47 to 2.28 points, while the control group diminished VAS not significantly from 6.92 to 5.75 (p=0.06). The significant risk factors for developing CT are female, Caucasian, middle-age/working-life, with repetitive manual movements or forced positions, right SE tendon, formative calcification. Kinesiotherapy improves mobility and electrotherapy reduces pain significantly in the experimental group
Keywords
Calcifying tendonitis; Shoulder pain; Physical therapy; Electrotherapy; Kinesiotherapy
Introduction
Calcifying tendonitis (CT) is the intratendinous deposit of calcium on a previously healthy rotator cuff tendon [1]. This deposit can be of calcium phosphate or carbonate [2]. Its incidence ranges between 2.7 and 20% in asymptomatic patients, with an average age between 30 and 50 years and affects more women than men [3,4]. The etiology is unknown, but is believed to be a tendon fibrosis and necrosis with associated degeneration which could favor the deposition of crystals [5,6]. However, some authors believe it is not a degenerative process [4,6,7]. CT is a debilitating, painful and frequent disease, which causes high socio economic impact and work absenteeism [8]. Three stages with clinical, histological and radiographic correlation are described [4], but sometimes overlap: pre-calcification, calcification (with a formative and a resorptive phase) and post-calcification (with restitution of the tendon architecture) [1]. The clinical picture is highly variable. There are patients with chronic pain conditions, patients with acute painful crises often associated with the resorptive phase of the deposit; and asymptomatic patients [1]. CT is more frequent in asymptomatic patients [9].
Treatment of CT is initially conservative and depends on its evolution [10]. It varies from therapeutic abstention in asymptomatic patients to conservative treatments: non-steroidal anti-inflammatory drugs (NSAIDs), physiotherapy [11], electrotherapy (micro waves, short waves, TENS, ultrasounds, iontophoresis, interferentials, pulsed electromagnetic therapy), ultrasonic shock waves therapy [12], antiinflammatory radiotherapy and washing guided/blinded techniques. Finally, surgical treatment can be performed by arthroscopic [13] or open surgery [14]. Surgical techniques should be performed in patients with progressive symptoms or with constant pain that interferes with normal activity and where conservative treatments have failed [1].
The aim of this study is to determine the different risk factorsassociated with CT, to characterize it epidemiological-clinicalradiological, in a number of cases, and to assess the effect of physical therapy in improving mobility and decreasing pain, and its possible association with clinical factors, at our Rehabilitation Department.
Material and Methods
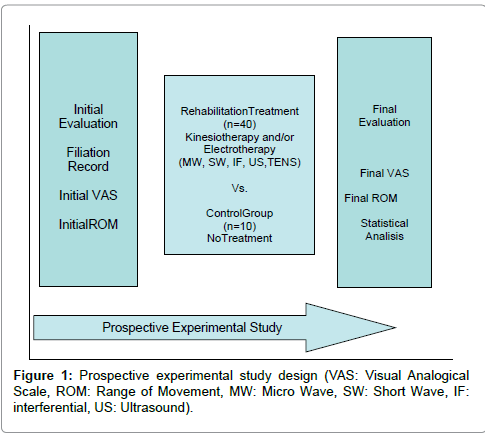
We performed a prospective experimental intervention to a series of 50 patients (40 experimental group and 10 control group) diagnosed of CT referred to the Rehabilitation Department of the University Welfare Complex of Salamanca, during the period October 2011 to February 2013. In the first consultation (initial assessment) the demographics (age, sex, occupation, laterality, dominance), personal history (previous pharmacological treatments, rehabilitation, shock waves or surgery), predisposing factors and type of calcification (formative/resorptive), were collected. The evaluation of the shoulder initial Range of Movement (initial ROM) in its four movements (flexion, abduction, internal and external rotation) was performed. Pain was valued according to the visual analog scale (initial VAS). The intervention consisted in prescribing treatment as appropriate: Kinesiotherapy (KT) (if restricted mobility) or various electrotherapy modalities (US ultrasound, TENS, Microwave MW, Shortwave SW, Interferential IF) (if pain), or a combination of both were prescribed. Ten patients (20%) constituted the control group. They were evaluated with the same parameters, at the beginning and at the end of the treatment, in order to see the natural history of the disease. In the post-intervention consultation (final evaluation) mobility (final ROM) and pain (final VAS) was re-evaluated, in addition to the global patient satisfaction (Figure 1).
The statistical program SPSS version 20.0 was used. In the descriptive statistics of the variables means and standard deviations for quantitative variables were used. Frequencies and percentages were used for qualitative variables. The Chi-square test was used to contrast qualitative variables. The T-Student test was used to evaluate quantitative variables.
Results
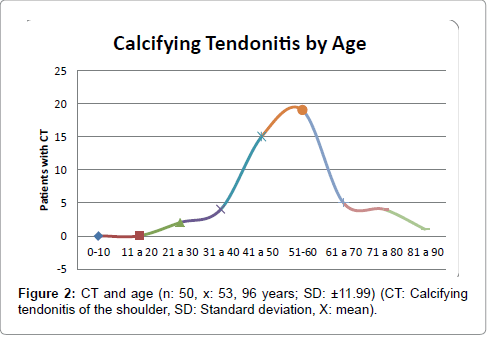
CT is more common in women (n=36; 72%) than in men (n=14; 28%) and with statistical difference (p=0.00) (Table 1). The CT occurs in middle age/working life, with an average of 53.96 years, with a SD=±11.99 (Figure 2).
| Variables | n | % | SS | |
| Sex | Female | 36 | 72.00% | 0.00 |
| Male | 14 | 28.00% | ||
| Calcification | Formative | 39 | 76.47% | 0.00 |
| Resorptive | 12 | 23.53% | ||
| Previous treatment | Yes | 46 | 92.00% | 0.00 |
| No | 4 | 8.00% | ||
| Rhb | Yes | 9 | 18.00% | 0.00 |
| No | 41 | 82.00% | ||
| Pain | Yes | 48 | 96.00% | 0.00 |
| No | 2 | 4.00% | ||
| Rx | Yes | 49 | 98.00% | 0.00 |
| No | 1 | 2.00% | ||
| MRI | Yes | 9 | 18.00% | 0.00 |
| No | 41 | 82.00% | ||
| ECO | Yes | 23 | 46.00% | 0.21 |
| No | 27 | 54.00% | ||
| Muscle | SE | 48 | 96.00% | 0.02 |
| IE | 4 | 8.00% | ||
| SEsc | 4 | 4.00% | ||
| Laterality | Left | 17 | 34.00% | 0.03 |
| Right | 33 | 66.00% | ||
| Intensity | Mild | 5 | 10.20% | 0.00 |
| Moderate | 28 | 57.14% | ||
| Severe | 16 | 32.65% | ||
| Time of pain | < 1 month | 3 | 6.00% | 0.00 |
| 1-6 month | 15 | 30.00% | ||
| 6-12 month | 11 | 22.00% | ||
| > 1 year | 21 | 42.00% | ||
| Rhb: Rehabilitation;Rx: Radiography; MRI: Magnetic Resonance Imaging; ECO: Ecography;SE: Supraespinatus Muscle; IE: Infraespinatus Muscle; SEsc: Subescapularis Muscle;SS: Statistical Significance. | ||||
Table 1: Resume of the frequency, percentage and statistical significance of CT and its main variables/risk factors analysed.
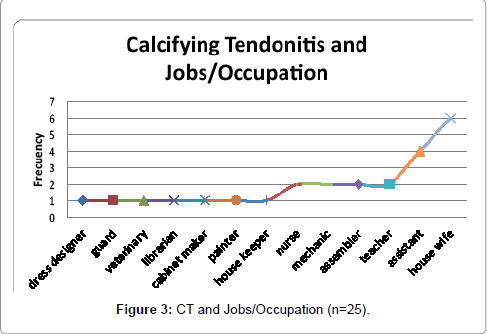
The most common occupation of the patients was housekeeper or assistant, while all occupations had risk factors for the presentation of shoulder pain (forced postures, repetitive movements and cargo handling) (Figure 3).
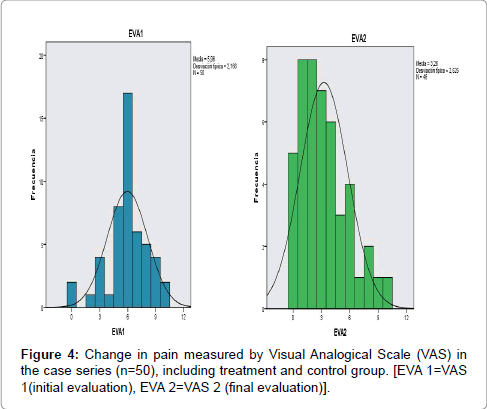
As for the laterality, 66% (n=33) were right CT, 30% (n=15) were left CT and 4% (n=2) were bilateral. As for tendon, in 46 patients (92%) CT affected the supraspinatus (SE), 4 patients (8%) to the infraspinatus (IE) and 4 patients (8%) the subscapularis (SESC). For diagnosis, all patients (n=50, 100%) had radiograph examination, 24 patients (48%) were examined by ultrasound, and 8 patients (16%) were also carried out a magnetic resonance imaging (MRI). That is, CT prevailed in right shoulders, in the SE tendon and all patients had radiological, ultrasound and MRI confirmation, in that order. Most patients had formative (n=38; 76%) rather than resorptive calcifications (n=12; 24%) which was statistically significant (p=0.00) (Table 1). Most patients (n=46; 92%) received some type of prior treatment (drugs, injections, shockwave or rehabilitation), they have not undertaken prior rehabilitation (n=41; 82%) had pain (n=48; 96%), chronic pain greater than 6 months (n=33; 66%), and limited mobility (n=20; 40%), with statistical significant difference (p=0.00) (Table 1). Most patients preoperatively had moderate pain (n=28, 56%), severe (n=16, 32%) and only slight (n=6, 12%), with statistical significant difference (p=0.00) (Table 1). The total of patients with restricted mobility made kinesiotherapy (KT) treatment (n=20; 40%) and 80% underwent electrotherapy, whether TENS, US, SW or MW (n=40) to reduce pain (Table 1). The average number of rehabilitation sessions was 28.6 ± 12.9 days in our series. VAS diminished from 5.96 to 3.26 points after kinesiotherapy and/or electrotherapy treatment (Figure 4).
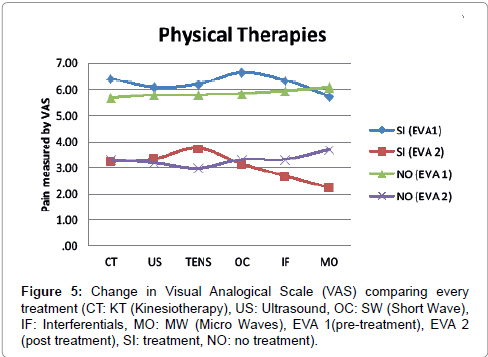
In general, people with restricted mobility receive kinesiotherapy treatment (p=0.004), whereas patients with pain also receive different treatments of electrotherapy (US, MW, SW, IF, TENS) without defined protocol and without statistical association among them (p>0.05). However, it has been observed statistical association between treatment combination of KT+MW (p=0.012) (Table 2). When we compare the effect of treatment on pain, we see that the combination of different treatments reduces pain, but this decline is more pronounced when MW, IF, SW and KT (Figure 5) is prescribed. While different types of treatment reduce the VAS, there is no statistical significant difference. MW, IF and SW (in that order) decrease VAS more than other treatments (Table 3).
| Treatment | n | % | SS |
| KT | 20 | 100 | 0.004 |
| US | 30 | 60 | 0.47 |
| TENS | 20 | 40 | 0.642 |
| MW | 25 | 50 | 0.012 |
| SW | 8 | 16 | 0.529 |
| IF | 3 | 6 | 0.808 |
| KT: Kinesiotherapy; US: Ultrasound; MW: Microwaves; SW: Short Waves; IF: Interferentials; SS:Statistical Significance. | |||
Table 2: Statistical association of the different treatments (kinesiotherapy and electrotheraphy) in the treatment group.
| VAS 1 | KT | Yes | N | Media | |||
| 20 | 6.40 | Tipical Desviation | Tipical Error of the media | SS | |||
| VAS 1 VAS 2 |
KT US |
No | 30 | 5.67 | 1.569 | .351 | 0.24 |
| Yes | 19 | 3.21 | 2.468 | .451 | |||
| VAS 2 VAS 1 |
No | 27 | 3.30 | 2.463 | .565 | 0.91 | |
| Yes | 32 | 6.06 | 2.614 | .503 | |||
| VAS 1 VAS 2 |
US TENS |
No | 18 | 5.78 | 1.917 | .339 | 0.66 |
| Yes | 28 | 3.32 | 2.602 | .613 | |||
| VAS 2 VAS 1 |
No | 18 | 3.17 | 2.510 | .474 | 0.84 | |
| Yes | 22 | 6.18 | 2.618 | .617 | |||
| VAS 1 VAS 2 |
TENS SW |
No | 28 | 5.79 | 2.015 | .430 | 0.53 |
| Yes | 18 | 3.72 | 2.299 | .434 | |||
| VAS 2 VAS 1 |
No | 28 | 2.96 | 2.372 | .559 | 0.32 | |
| Yes | 8 | 6.63 | 2.617 | .495 | |||
| VAS 1 VAS 2 |
SW IF |
No | 42 | 5.83 | 1.408 | .498 | 0.35 |
| Yes | 8 | 3.13 | 2.273 | .351 | |||
| VAS 2 VAS 1 |
No | 38 | 3.29 | 1.808 | .639 | 0.87 | |
| Yes | 3 | 6.33 | 2.670 | .433 | |||
| VAS 1 VAS 2 |
IF MW |
No | 47 | 5.94 | 1.528 | .882 | 0.76 |
| Yes | 3 | 2.67 | 2.211 | .322 | |||
| VAS 2 VAS 1 |
No | 43 | 3.30 | .577 | .333 | 0.68 | |
| Yes | 15 | 5.73 | 2.605 | .397 | |||
| VAS 1 VAS 2 |
MW | No | 35 | 6.06 | 1.624 | .419 | 0.63 |
| Yes | 13 | 2.23 | 2.376 | .402 | |||
| VAS 2 | No | 33 | 3.67 | 2.127 | .590 | 0.082 | |
| CK:Kinesiotherapy; US:Ultrasound; MW:Microwaves; SW:Short Waves; IF:Interferentials; SS:Statistical Significance. | |||||||
| All patients after any of the different treatments reduce pain but without statistical difference from one to another. | |||||||
Table 3: Effect of the different treatments on the change of pain measured by Visual Analogical Scale (VAS) analysed individually.
There is statistical significant improvement (p<0.05) in mobility (ROM) after KT treatment in all ranges of motion (Table 4).
| KinesioTherapy | SS | |||||||
| Yes | No | |||||||
| n | % Column | % Row | n | % Column | % Row | |||
| Inicial Flexion | Complete | 2 | 10.00% | 6.90% | 27 | 90.00% | 93.10% | 0.000 |
| Incomplete | 18 | 90.00% | 85.70% | 3 | 10.00% | 14.30% | ||
| Final Flexion | Complete | 12 | 66.70% | 29.30% | 29 | 100.00% | 70.70% | 0.000 |
| Incomplete | 6 | 33.30% | 100.00% | 0 | 0.00% | 0.00% | ||
| Inicial Abduction | Complete | 2 | 10.00% | 6.50% | 29 | 96.70% | 93.50% | 0.000 |
| Incomplete | 18 | 90.00% | 94.70% | 1 | 3.30% | 5.30% | ||
| Final Abduction | Complete | 12 | 66.70% | 29.30% | 29 | 100.00% | 70.70% | 0.000 |
| Incomplete | 6 | 33.30% | 100.00% | 0 | 0.00% | 0.00% | ||
| Inicial ER | Complete | 6 | 31.60% | 16.70% | 30 | 100.00% | 83.30% | 0.000 |
| Incomplete | 13 | 68.40% | 100.00% | 0 | 0.00% | 0.00% | ||
| Final ER | Complete | 15 | 83.30% | 34.10% | 29 | 100.00% | 65.90% | 0.023 |
| Incomplete | 3 | 16.70% | 100.00% | 0 | 0.00% | 0.00% | ||
| Inicial IR | Complete | 4 | 21.10% | 12.90% | 27 | 90.00% | 87.10% | 0.000 |
| Incomplete | 15 | 78.90% | 83.30% | 3 | 10.00% | 16.70% | ||
| Final IR | Complete | 10 | 55.60% | 25.60% | 29 | 100.00% | 74.40% | 0.000 |
| Incomplete | 8 | 44.40% | 100.00% | 0 | 0.00% | 0.00% | ||
| ER: External Rotation; IR: Internal Rotation; SS:Statistical Significance. | ||||||||
| All patients regain mobility in all range of movements from the initial to the end of kinesiotherapy treatment. | ||||||||
Table 4: Effect of Kinesiotherapy over mobility of the shoulder, in the different ranges of movement.
Regarding the associations between pain and type of calcification it has been found that patients with resorptive calcifications had more chronic pain, while patients with formative calcifications presented both chronic and acute-subacute pain; although this did not demonstrate statistical significance (p=0.11) (Table 5).
Calcification Formative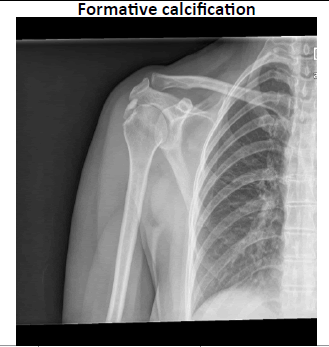 |
Calcification Resorptive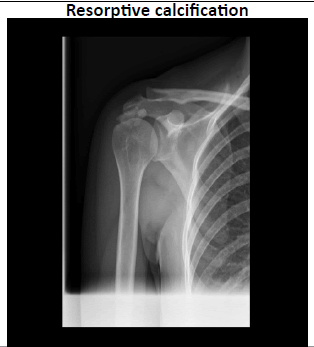 |
SS | ||||||
| n | %column | %row | n | %column | %row | |||
| Time of pain | Acute Subacute |
16 | 42.10% | 88.90% | 2 | 16.70% | 11.10% | 0.11 |
| Chronic | 22 | 57.90% | 68.80% | 10 | 83.30% | 31.30% | ||
| SS:Statistical Significance | ||||||||
Table 4: Effect of Kinesiotherapy over mobility of the shoulder, in the different ranges of movement.
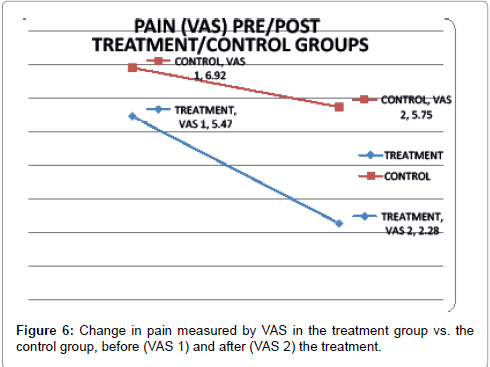
With respect to pain, the rehabilitation treatment group decreased VAS significantly (p=0.00) from 5.47 to 2.28 points, while the control group diminished VAS not significantly from 6.92 to 5.75 (p=0.06) (Table 6). Therefore, in the evolution of pain, patients from the control group showed no change (Figure 6).
| GROUPS | VAS 1 | VAS 2 | SS |
| Treatment(n=40) | 5.47 | 2.28 | 0 |
| Control (n=10) | 6.92 | 5.75 | 0.06 |
| SS:Statistical Significance | |||
Table 6: Relationship between treatment group/control group and change in pain measured by Visual Anological Scale (VAS).
Discussion
CT of the shoulder is a common, painful, crippling disease that produces high socio economic impact [8], great use of medical resources [15] and work absenteeism. It is also the most painful acute disease affecting the shoulder [1]. Pain is the main cause of disability because of the loss of function, symptoms can persist up to one year after the first visit in 50% of patients [15]. CT is more common in women, as demonstrated by most studies (Barrera [1], Juan-García [6], García [8], Jimenez-Garcia-Llorente [9], Jimenez-Martín [13], Esparza- Ferrera [16], Martinez-Rodríguez [17]), including ours. However, other studies show differences in gender. Thus, Jacobelli argues that CT affects both sexes equally; while Hernández-Díaz [18] found predominance in males. Gagliardi and Sutrez-Lissi in his research note that in Caucasians tendinitis occurs more common in sedentary women, over 40 years, while in Asia has been more common in men over 60 years [18]. CT is common in middle age/working life, between 30 and 50 years (Jimenez-García [8], Jimenez-Martín [13] Hernandez-Díaz [18]). In our study, the average age is 53.96 years, which coincides with the findings of Esparza-Ferrera [16] (54 years) and Martinez-Rodríguez [17] (53,1 years), and differs from that of Rioja-Toro [2] (48 years).
Chronic rotator cuff tendon pathology and CT are associated with occupations that are made with elbows in raised position or tighten the tendons or subacromial bursa (forced postures), lifting and reaching actions (cargo handling) or the continued use of the arm in abduction or flexion (repetitive movements), such as painters, plasterers, fitters of structures. In our case series, the occupations of the patients had one or more of these labor risk factors [15]. CT predominantly affects the right shoulder, as argued Rioja-Toro [2] (61.2%), Jimenez-Martín [13] (59.3%), Martinez-Rodríguez [17] (62.5%); although up to 25 to 30% can be bilateral [8,9]. Jimenez-Martín [13] found bilateralism in 18.5% of cases, although reports may have even higher bilateralism (18-47%) [19]. In our series of cases was more frequent right CT laterality (66%), followed by the left (30%) and bilateral (4%). CT is very common in the rotator cuff and more frequently affects the supraspinatus tendon (SE), being less common in the infraspinatus muscle (IE), teres minor (TM), and very rare in the subscapularis (SESC) [1,9,13,16,20]. Specifically, the most common site of onset is between 1 and 2 cm medial to the tendon insertion on the great tuberosity (troquiter) [13], and it is the junction of fibrocartilage with the tendon [8]. The presence of a poorly vascularized tendon area could be a relevant factor for degenerative cuff pathology; being the avascular zone at an average distance of 7.8 mm from the insertion of the muscle [16]. In our series we found involvement of the SE (92%), IE (8%) and SESC (8%). Adamietz [20] reported similar involvement in the SE (80%), IE (15%) and SESC (5%), consistent with our findings and the literature reviewed. The imaging diagnoses can be done with plain radiography, ultrasound or magnetic resonance imaging (MRI) [9,13,16]. Plain radiography has been proven as an effective method [9]; although not having a calcification expression by radiology image will depend on the density of calcium and its size [21]. Plain radiography is the first imaging study, it let us typify the calcification and evaluate the results. The second imaging study must be an ultrasound scan. It detects calcifications better than MRI and it can be used in therapeutic guided/aspiration techniques. MRI is not helpful in neither detecting nor classifying CT of the shoulder. Besides is an expensive technique with false negative/false positive results. MRI is only indicated if rupture of SE tendon and calcification is suspected.
In our series, radiography was made in 100% of patients, ultrasound in 48% and MRI in 8%. Jimenez-Martín [13] in his study performed 100% X-ray, 81.5% ultrasound and 40.7% MRI, similar to our data. The apatite crystals deposit in periarticular tissues is more common in shoulder, but can occur in the hip, knee and carpal epicondyle, resulting in periarthritis and CT of the SE and bursitis (sub-deltoid, trochanteric) [18]. The reason for crystals, usually calcium phosphate, to be deposited in tendons and bursae is still not clear [6]. It seems that there must be a tendon fibrosis and necrosis with consequent degeneration to favor the crystal deposition [6,7]. However, other authors state that it is not a degenerative process [7]. CT can also be located in poorly vascularized areas, areas of chondral metaplasia or damaged tendons. It is suggesting that the alteration of the connective tissue promotes nucleation of apatite and calcification [13]. The attacks can be spontaneous or secondary to trauma. Most deposits are asymptomatic, but fragmentation, mobilization and deposited crystals produce an intense inflammatory reaction, which causes severe pain, loss of function, swelling, heat and redness. This process has a sudden onset, persists for 2-3 weeks, and is resolved spontaneously and slowly. If the inflammation is chronic, the tendon can calcify and cause CT, whose diagnosis is primarily radiologic [13].
Palma [22] classified calcifying tendonitis in two major groups: type I (resorptive) of hairy, shaggy, heterogeneous and poorly defined peripheral appearance, although clinically characterized by acute pain in the resorptive phase; and type II (Formative), whose density is homogeneous, as a circumscribed lesion, painless or with little pain and related to the formative or late phase [13,23].
In our series, the formative (type II) calcification was more frequent than the resorptive (type I) (74% vs 26%). Jimenez-Martín [13] found in his series 81.5% of formative (type II) calcifications and 18.5% of resorptive (type I), those data coincide with ours.
The CT treatment is controversial and varied, depending on the developmental stages. In the acute phase rest, ice, NSAIDs, colchicine, or infiltration of corticosteroids is postulated [2,6,13,18,23]; while in the chronic phase analgesics, electrotherapy (US, shockwaves, Iontophoresis [2] short wave [8], TENS and laser [18], pulsed electromagnetic therapy, radiation at low dosis [20], ozone, washing/aspiration by ultrasound-guided/arthroscopic could be prescribed [6,7,13,18,23]. In our series, 92% of patients had been previously treated, either by drugs, infiltration, shockwaves or rehabilitation. Martinez-Rodríguez [17] referred that their patients before being treated with ultrasonic shock wave therapy; had made kinesiotherapy (KT), thermotherapy and previous infiltration, which is consistent with our observations.
CT has a clinic that is insidious or sudden onset, acute or severe, with a limited movement in three spatial axes [13]. In our series, 96% had pain, chronic pain 66%, and 40% limited mobility, so they received electrotherapy treatment and KT.
The number of rehabilitation sessions in CT is also controversial. In our series, the average number was 28 sessions. Jimenez-García [8] with 15 sessions of KT+US+iontophoresis found the same results as 15 sessions of KT+US+SW. Rioja-Toro [2] found with 40 sessions of US+Iontophoresis better results than 20 sessions.
Conservative treatment fails to relieve pain and mobility in CT of the shoulder [1]. There is a high density of nociceptors close to the insertion on the shoulder rotator cuff, which explains that these tissues are more sensitive to painful stimuli [24]. Early diagnostic and appropriate therapeutics not only diminishes the pain but also improves functional capacity of the shoulder, reducing the risk of inability of the joint on the long term [15]. In our series, after the treatment, pain measured by VAS diminished 2.7 points, severe pain decreased significantly from 33% to 11% and 55% reported subjective improvement.
Treatment of CT remains controversial [6]. That is why in daily practice combination of treatments is used [8]. In our Department there is not a treatment protocol. Patients with restricted mobility receive KT, and those with pain get electrotherapy techniques without any special preference. However, statistical association was seen in the combination treatment of KT+MW. Different Electrotherapy techniques and KT reduce pain, although no statistically significant difference was seen in our study. The technique that most decreases pain was the MW, followed by IF, SW and KT. These findings agree with those of Jimenez-García [8], who demonstrated that the combination CT+US+iontophoresis is no better than the combination of CT+US+OC. On the other hand, Martinez-Rodríguez [17] reported that 50% of patients receiving shockwaves previously failed the combination of thermotherapy+infiltration+KT.
Rioja-Toro [2] argues that CT is a disease entity with its own characteristics, with a dark pathophysiology, and the required rehabilitation treatment focuses on improving mobility and decreasing pain, but the calcification is neglected. Even so, in our series, patients with limited mobility regain ROM significantly.
There is no clear consensus, when we review the state of the art, of the possible factors that influence the outcome of the treatment of this disease by arthroscopic surgery [1]. However, the resorptive calcification (type I) has a favorable prognosis [8]. In our series, the resorptive calcifications had more chronic pain while formative calcifications had acute/subacute pain, but without statistical difference.
Conclusions
The significant risk factors for developing CT are female, Caucasian, middle-age/working-life, with repetitive manual movements or forced positions. The most clinical features of CT are: right SE, formative calcification, painful, acute/subacute evolution, mild to moderate intensity and prior treatment. Diagnostic is made by a proper physical exploration and confirmation is done with radiography, being sometimes necessary an ultrasound scan. The 28 days treatment has demonstrated effectiveness in diminishing pain and recovering functional mobility in the experimental group. However, no one specific treatment (KT, US, TENS, MW, SW, IF) has shown significant difference in reducing the pain, compared to another. The control group did not improve pain spontaneously. There is no association between time of evolution and type of calcification in this study.
Study Limitations
This is a small size sample study (n=50). Fourteen months (from October 2011 to February 2013) were needed to collect such a number of patients, since this was a prospective study. Then, the treatment was prescribed and afterwards the follow up period, to evaluate the results in both the control and experimental groups. Even so, the results are very similar to those found by different researchers, as previously exposed in this article.
Acknowledgment
To Saturnino Diaz Trujillo, librarian of Santa Cristina’s University Hospital, for his article research. Without his help, this work could not be done.
References
- Barrera-Cadenas JL,Campa-RodríguezAY, García-Prendes V, Resultados V (2010) del tratamientoartroscópico de las tendinitis calcificantes del manguito de los rotadores del hombro. RevEspCirOrtopTraumatol54: 100-105.
- Rioja-Toro J, Romo-Monje M, Cantalapiedra-Puentes E, González-Rebollo AY,Blázquez-Sánchez E (2001)Tratamiento de la tendinitis calcificante del hombro mediante iontoforesis con ácido acético y ultrasonidos Rehabilitación (Madr) 35:66-170.
- Porcellini G, Paladini P, Campi F, Paganelli M (2004) Arthroscopic treatment of calcifying tendinitis of the shoulder: Clinical and ultrasonographic follow-up findings at two to five years. J ShoulderElbowSurg13:503-8.
- UthoffHK,Dervin GF, Loehr JF (2006) Calcifying tendonitis. En: Rockwood Jr CA, Matsenerd FA, Wirth MA, Lippitt SB. Hombro. Tomo II. Madrid: Marban1033-1057.
- Mc Laughlin HL (1946) Lesions of the músculostendinous cuff of the shoulder. III. Observations on the pathology, course and treatment of calcific deposits. Ann Surg124:354-362.
- Juan-García FJ, González-Movilla C, yCordal-López AB (2004)Efectividad del tratamiento mediante ondas de choque extracorpóreas en tendinitis calcificadas del hombro. RevEspReumatol31:116-121.
- UhthoffHK (1975) Calcifying tendinitis: an active cell-mediated calcification. VirchowsArch [A] 366:51-68.
- Jiménez-García D, López-Dolado E, López-Zarzuela MC (2008)Tratamiento de la tendinopatíacalcificante de hombro:¿iontoforesis con ácido acético u onda corta? Rehabilitación (Madr) 42:239-245.
- García-Llorente JF, Galíndez-Aguirregoikoa E, García-Vivar ML,Aranburu-Albizuri JM (2009) Protocolo diagnóstico del hombro doloroso crónico. Medicine10:2222-2225.
- Re LP, Karzel RP (1993) Management of rotator cuff calcifications. OrthopClin North Am 24:125-132.
- Hamada J, Ono W, Tamai K,Saotome K, Hoshino T (2001) Analysis of calcium deposits in calcific periarthritis. J Rheumatol28:809-813.
- Loew M,Jurgowski W, Mau HC, Thomsen M (1995) Treatment of calcifying tendonitis of rotator cuff by extracorporeal shock waves: A preliminary report. J Shoulder Elbow Surg4:101-105.
- Jiménez-Martín A, Santos-Yubero FJ, Zurera-Carmona M, Najarro-Cid FJ, Chaqués-Asensi, et al. (2012) Tratamiento de la tendinitis calcificante de hombro mediante artroscopia. Trauma Fund MAPFRE 23:32-37.
- Neer IICS (1990) Shoulder reconstruction. Philadelphia: Saunders 427-433.
- Vicente-Herrero MT,Capdevila García L, López González ÁA, Ramírez Iñiguez de la Torre MV (2009) El hombro y sus patologías en medicina del trabajo. SEMERGEN. 35:197-202.
- Esparza-Ferrera C,y Ricard F (2009)Estudio comparativo de pruebas ortopédicaspara la valoración y confirmación diagnóstica de tendinopatía del músculo supraespinoso. Osteopatía Científica 4:86-92.
- Martínez-RodríguezME, y Peña-Arrebola A (2005)Tratamiento de tendinitis y bursitis calcificadas subacromiodeltoideas con ondas de choque. Rehabilitación (Madr) 39:2-7.
- Hernández-Díaz A, González-Méndez BM, Orellana-MolinaA, Martín-Gil JL, y Berty-Tejeda J (2009) Láser de baja potencia en el tratamiento de las calcificaciones de hombro. RevSocEsp Dolor 16: 230-238.
- Uhthoff HK, Loehr JF (1997)Calcifictendinopathy of the rotator cuff: pathogenesis, diagnosis and management. J Am AcadOrthopSurg 5:183-191.
- Adamietz B, Schulz-Wendtland R, Alibek S, Uder M, Sauer R (2010)Calcifying Tendonitis of the Shoul Oder Joint. Predictive Value of Pretreatment Sonography for the Response to Low-Dose Radiotherapy. StrahlentherOnkol 1:18-23.
- Muñoz S (2001) Síndrome del hombro doloroso: estudio radiológico. Revista Médica. Área académica Clínica12: 12-25.
- De Palma AF, Kruper JS (1961)Long term study of shoulder joints afflicted with and treated for calcific tendinitis. ClinOrthopRel Res20:61-72.
- Tillander BM,Norlin RO (1998) Change of calcifications after arthroscopic subacromial decompression. J Shoulder Elbow Surg May/June 7:213-217.
- Minaki Y, Yamashita T, Takebayashi T, Ishii S (1999)Mechanosensitive afferent units in the shoulder and adjacent tissues. ClinOrthop Related Res 369:349-356.
Relevant Topics
- Child Health Education
- Construction Safety
- Dental Health Education
- Holistic Health Education
- Industrial Hygiene
- Nursing Health Education
- Occupational and Environmental Medicine
- Occupational Dermatitis
- Occupational Disorders
- Occupational Exposures
- Occupational Medicine
- Occupational Physical Therapy
- Occupational Rehabilitation
- Occupational Standards
- Occupational Therapist Practice
- Occupational Therapy
- Occupational Therapy Devices & Market Analysis
- Occupational Toxicology
- Oral Health Education
- Paediatric Occupational Therapy
- Perinatal Mental Health
- Pleural Mesothelioma
- Recreation Therapy
- Sensory Integration Therapy
- Workplace Safety & Stress
- Workplace Safety Culture
Recommended Journals
Article Tools
Article Usage
- Total views: 15191
- [From(publication date):
December-2015 - Apr 01, 2025] - Breakdown by view type
- HTML page views : 14212
- PDF downloads : 979