Calcaneocuboid Joint Involvement in Calcaneal Fractures-CT Based Analysis and Classification
Received: 07-Oct-2018 / Accepted Date: 22-Oct-2018 / Published Date: 29-Oct-2018
Keywords: Calcaneal fracture; Calcaneocuboid joint involvement; Fracture morphology; CT scan; Fracture classification
Level of Evidence
Level III, retrospective cohort study
Introduction
Calcaneocuboid joint (CCJ) involvement has been shown to play an important role in calcaneal fractures [1-3]. Calcaneal fractures with CCJ involvement are associated with more severe trauma and worse outcome [3]. Hence, the calcaneocuboid should attract our interest during surgery. However, our understanding of CCJ involvement is still scarce. Only a handful of studies address this issue [3].
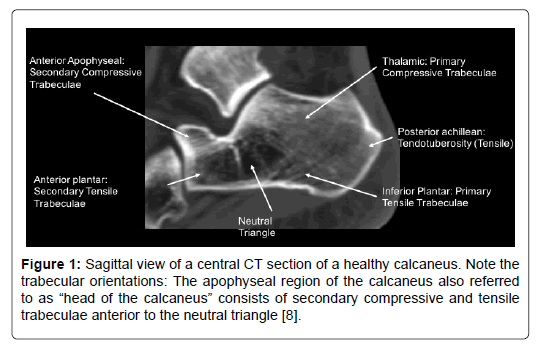
This does not only concern treatment and outcome, but also fracture pathology and classification [4-6]. Biomechanics and fracture pathology of the posterior facet have been described in detail [7,4]. But if it comes to the anterior apophyseal region even nomenclature becomes inconsistent. It is referred to as “anterior process” or “head of calcaneus”. The apophyseal region is separated from the tuberosity (thalamic region) by Wards’ neutral tringle, and consists of primary compressive and secondary tensile trabeculae (Figure 1) [8]. Extension of the primary fracture line into the CCJ has been described by Silhanek et al. [4]. They portrayed in their retrospective study that calcaneal fractures exhibiting a medial primary fracture line are associated with a more severe fracture pattern and an increased incidence of anterior articular extension. However, they lack to be more specific about CCJ involvement. A more precise analysis of CCJ involvement was presented by Ebraheim et al. [1,2]. They could show that CCJ involvement is more common with joint depression type fractures, and extension of the fracture line into the CCJ should be suspected in presence of significant lateral column comminution or lateral talar subluxation. However, their findings are based mainly on coronal CT scans.
Figure 1: Sagittal view of a central CT section of a healthy calcaneus. Note the trabecular orientations: The apophyseal region of the calcaneus also referred to as “head of the calcaneus” consists of secondary compressive and tensile trabeculae anterior to the neutral triangle [8].
Therefore, the aim of this study was to describe CCJ involvement and fracture pathology of the “calcaneal head” more precisely. A secondary research question was to evaluate the need of a separate classification of the CCJ injuries.
Methodology
After approval by the internal review board (IRB) 100 CT-data-sets of 87 consecutive patients were analyzed retrospectively.
Inclusion criteria
Displaced intraarticular calcaneal fractures (at least one articular surface of the calcaneus had to be involved), age equal or above 18 years. Bilateral fractures, concomitant injuries or multiple injuries were not considered as exclusion criteria.
Exclusion criteria
Insufficient CT-data-set, e.g. missing reformations.
Standard CT scans were obtained using spiral-CT (“Sensation 16”, Siemens, Germany) with table feed of 3 mm/s, slice collimation of 0.75 mm, pitch factor of 0.65 and slice thickness of 2 mm. Axial, sagittal and coronal reformations were obtained of each fracture. Axial views were reconstructed parallel to the sole of the foot, sagittal views orthograde to the ankle joint and the coro-nal views parallel to the calcaneocuboid joint (CCJ).
Demographic data of the patients were obtained from the clinical database (age, gender, injury mechanism, side of injury).
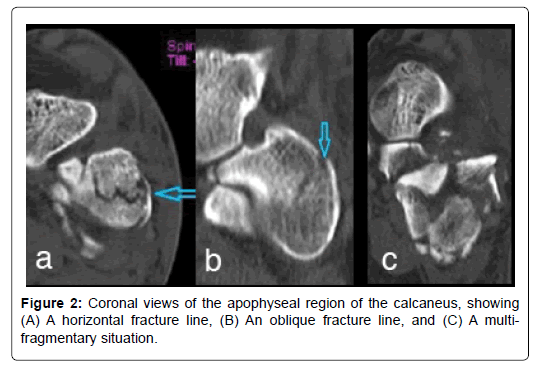
CT scans were analyzed systematically including the criteria displayed in Table 1 with a specific focus on CCJ involvement. These included: Analysis of number of fracture lines (using axial, sagittal and coronal views), localization of sagittal fracture line (on axial view), extension of primary fracture line into the CCJ, and orientation of fracture lines (vertical, horizontal oblique, multi-fragmentary; primarily on coronal views (Figure 2).
| Analysis of CT Scans |
| Bohler’s angle (on central sagittal view) |
| Estimated shortening of the calcaneus (on axial view) |
| no shortening |
| mild shortening, up to 10% |
| moderate shortening up to 30% |
| severe shortening >30% |
| Axial deformation (varus or valgus): longitudinal axis [°] |
| Size of central defect (axial views) |
| no defect |
| small defect ≤ 3 cm2 |
| medium size defect >3 cm2 ≤ 6 cm2 |
| large defect >6 cm2 |
| Fracture and displacement of the articular surfaces: posterior, medial and anterior facet of the subtalar joint and the calcaneocuboid joint |
| no displacement |
| <2 mm |
| >2 and ≤ 5 |
| ≥ 5 mm |
| Fracture classification |
| Essex-Lopresti |
| Sanders |
| Eastwood/Atkins |
| Zwipp |
| Evaluation of calcaneocuboid joint |
| No of fracture lines |
| Orientation and localization of fracture lines (axial, coronal and sagittal views) |
| Analysis of primary fracture line (axial view, in [%] from lateral to medial) |
| Classification of CCJ fracture (provisionally) |
| Type I: non-displaced fracture |
| Type II: displaced two-part fracture |
| Type IIA-C |
| Type III: displaced three-part fracture |
| Type IIIAB-BC |
| Type IV: multifragmentary |
Table 1: Analysis of CT scans (Axial, Coronal and Sagittal views).
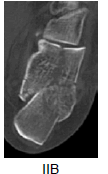
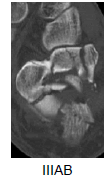
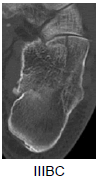
In addition, we tried to classify the CCJ injury (adapted from Sanders’ Classification of calcaneal fractures). Non-displaced fractures irrespective on the number of fracture lines were classified as type I. Two and three-part fracture as type II and III respectively, and multifragmentary fractures as type IV. The location of the fracture line was noted A=Lateral to C=Medial (Table 2).
| Type | Axial view | ||
|---|---|---|---|
| I |  |
||
| II |  |
 |
 |
 |
 |
 |
|
| IV |  |
||
Table 2: Proposed classification of CCJ involvement in calcaneal fractures, adapted from Sanders Classification system. Axial views of the spiral-CT scans were used to evaluate the CCJ.
Statistical analysis
Data are reported either as mean and standard deviation (SD) or median and range. Statistical analysis was performed using SPSS 25.0. Parametric and non-parametric statistical tests (Pearson and Spearman’s Rank Correlation Coefficient and Pearson’s Chi-square) were used to determine a meaningful association or difference between the parameters and groups where indicated. Statistical significance was assumed with p<0.05.
Results
Epidemiological data
A total of 87 patients were included into the study. 13 patients (15%) had bilateral calcaneal fractures. The left side was involved in 51 cases and in 49 cases the right side. Only 13 of the 87 patients were female (15%). The mean age was 43.75 ± 13.36 years. The most common injury mechanism was a fall from height (n=70; 79%), 8% (n=7) occurred during a motor vehicle accident and 13% (n=11) of the fractures were caused by other mechanisms (e.g. Distortion of the foot and ankle, direct trauma due to a heavy load (crush injury).
Fracture morphology
Mean Bohler’s angle was 8.9° (± 19.4°). Fracture morphology is displayed in Table 3a. The most common fracture type involved 3 joints with a medium size central defect and a moderate shortening of the heel. The posterior facet was severely displaced in 55.7%, whereas displacement of the medial and anterior facet was generally only slight. The CCJ was involved in 84% with moderate (35.7%) or severe (38.1%) displacement.
| Bohler’s angle | >20° | 11°-20° | 0°-10° | <0° |
|---|---|---|---|---|
| (n=99) | 31 | 37 | 21 | 10 |
| Shortening | Non | Mild/small | Moderate/medium | Large |
| (n=100) | 2 | 31 | 49 | 18 |
| Central defect size | Non | Mild/small | Moderate/medium | Large |
| (n=100) | 8 | 21 | 37 | 34 |
| Facets involved | 1 | 2 | 3 | 4 |
| (n=100) | 8 | 32 | 42 | 18 |
| Facet involved [%] | No displacement | Displacement <2 mm | Displacement >2 mm <5 mm |
Displacement >5 mm |
| Posterior (97%) | 2.1 | 8.2 | 34 | 55.7 |
| Medial (61%) | 12.9 | 53.2 | 21 | 12.9 |
| Anterior (28%) | 17.9 | 46.4 | 17.9 | 17.9 |
| CCJ (84%) | 6 | 20.2 | 35.7 | 38.1 |
| No. of fracture lines CCJ | 1 | 2 | 3 | Multifragmentary |
| [%], n=84 | 51.2 | 40.5 | 1.2 | 7.1 |
| Extension of prim. fx line into CCJ | Lateral 1/3 | Middle 1/3 | Medial 1/3 | - |
| [%], n=53 | 28.2 | 50.9 | 20.8 | |
| Orientation of CCJ fracture line | Vertical | Oblique superiorlateral-inferiormedial | Oblique superiormedial-inferiorlateral | Horizontal |
| [%], n=98 | 69.5 | 19.5 | 1.2 | 2.4 |
Table 3a: Fracture morphology.
70% were joint depression type of injuries, whereas 30% were classified as tongue type according to the Essex-Lopresti classification system. Sanders and Zwipp Classifications are displayed in Table 3b. Mean Zwipp Scale was 9.5 points (range, 4-12 points). Using the Eastwood/Atkins Classification system 16.8% classified as type I, 47.4% as type II, and 35.8% as type III.
| Sanders Classification | |||||||||
| Fracture Type (n=95) | IIA | IIB | IIC | IIIAB | IIIAC | IIIBC | IV | ||
| [%] | 28.4 | 8.4 | 8.4 | 21.1 | 10.5 | 6.3 | 16.8 | ||
| Zwipp Classification | |||||||||
| Points (n=100) | 4 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | n |
| n | 1 | 4 | 3 | 13 | 30 | 26 | 13 | 10 | 100 |
Table 3b: Sanders and Zwipp classifications.
Calcaneocuboid joint involvement
51.2% of the 84 fractures with CCJ involvement showed one fracture line, 40.5% two, and 1.2% three. In 7.1% a multifragmentary situation was present. Displacement of the fragments was <2 mm in 20.2%, >2 and <5 mm in 35.7% and >5 mm in 38.1%.
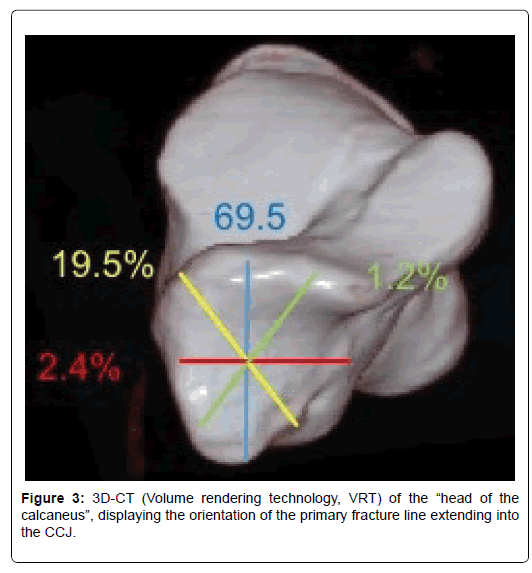
In the majority of the cases (69.5%) a vertical fracture line was present (based on the coronal view, followed by an oblique fracture line extending from superior-lateral to inferno-medial. Horizontal fracture lines were present in 2.4% and in 1.2% the fracture line extended from supe-rior-medial to inferno-lateral (Figure 3).
Based on the axial reformations the primary fracture line extended into lateral third of the CCJ in the in 28.2%, into the middle third in 50.9%, and in 20.8% into the medial third.
Evaluation of meaningful associations between the parameters
Table 4 displays a correlation matrix of the most important parameters analyzed. Significant corelations were found between CCJ involvement and general severity of the fracture, i.e. number of facets involved (rs=0.446, p<0.001), or size of central defect (rs=0.454, p<0.001).
| Bohler's angle | Shortening | No of facets involved | Displacement med. facet | Displacement ant. Facet | Classification (Zwipp) | Classification (Essex-Lopresti) | Classification (Sanders) | Classification (Eastwood/ Atkins) | Soft tissue | Fracture line CCJ | Central defect | Classification CCJ | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bohler's angle | Rs | 1 | -0.493** | -0.272** | -0.126 | -0.155 | -.355** | 0.155 | -0.272** | -0.433** | -0.182 | -0.204* | -0.206* | -0.224* |
| Sig. | 0 | 0.006 | 0.216 | 0.126 | 0 | 0.139 | 0.008 | 0 | 0.076 | 0.043 | 0.043 | 0.027 | ||
| N | 99 | 99 | 99 | 99 | 99 | 99 | 92 | 94 | 95 | 96 | 99 | 97 | 98 | |
| Shortening | Rs | -0.493** | 1 | 0.133 | 0.06 | -0.016 | 0.411** | 0.272** | 0.325** | 0.421** | 0.054 | 0.147 | 0.387** | 0.158 |
| Sig. | 0 | 0.188 | 0.551 | 0.873 | 0 | 0.008 | 0.001 | 0 | 0.6 | 0.143 | 0 | 0.119 | ||
| N | 99 | 100 | 100 | 100 | 100 | 100 | 93 | 95 | 95 | 97 | 100 | 98 | 99 | |
| No of facets involved | Rs | -0.272** | 0.133 | 1 | 0.613** | 0.656** | 0.733** | -0.072 | 0.281** | 0.099 | 0.035 | 0.446** | 0.318** | 0.500** |
| Sig. | 0.006 | 0.188 | 0 | 0 | 0 | 0.495 | 0.006 | 0.338 | 0.733 | 0 | 0.001 | 0 | ||
| N | 99 | 100 | 100 | 100 | 100 | 100 | 93 | 95 | 95 | 97 | 100 | 98 | 99 | |
| Displacement med. facet | Rs | -0.126 | 0.06 | 0.613** | 1 | 0.155 | 0.392** | -0.079 | 0.185 | 0.072 | 0.098 | 0.046 | 0.169 | 0.123 |
| Displacement med. facet | Rs | -0.126 | 0.06 | 0.613** | 1 | 0.155 | 0.392** | -0.079 | 0.185 | 0.072 | 0.098 | 0.046 | 0.169 | 0.123 |
| Sig. | 0.216 | 0.551 | 0 | 0.123 | 0 | 0.449 | 0.072 | 0.488 | 0.337 | 0.651 | 0.096 | 0.225 | ||
| N | 99 | 100 | 100 | 100 | 100 | 100 | 93 | 95 | 95 | 97 | 100 | 98 | 99 | |
| Displacement ant. facet | Rs | -0.155 | -0.016 | 0.656** | 0.155 | 1 | 0.571** | 0.029 | 0.285** | 0.069 | 0.1 | 0.316** | 0.207* | 0.253* |
| Sig. | 0.126 | 0.873 | 0 | 0.123 | 0 | 0.786 | 0.005 | 0.507 | 0.329 | 0.001 | 0.041 | 0.011 | ||
| N | 99 | 100 | 100 | 100 | 100 | 100 | 93 | 95 | 95 | 97 | 100 | 98 | 99 | |
| Classification (Zwipp) | Rs | -0.355** | 0.411** | 0.733** | 0.392** | 0.571** | 1 | 0.02 | 0.596** | 0.257* | 0.19 | 0.440** | 0.284** | 0.497** |
| Sig. | 0 | 0 | 0 | 0 | 0 | 0.851 | 0 | 0.012 | 0.063 | 0 | 0.005 | 0 | ||
| N | 99 | 100 | 100 | 100 | 100 | 100 | 93 | 95 | 95 | 97 | 100 | 98 | 99 | |
| Classification (Essex-Lopresti) | Rs | 0.155 | 0.272** | -0.072 | -0.079 | 0.029 | 0.02 | 1 | 0.039 | 0.089 | 0.088 | 0.122 | 0.14 | 0.05 |
| Sig. | 0.139 | 0.008 | 0.495 | 0.449 | 0.786 | 0.851 | 0.714 | 0.399 | 0.411 | 0.244 | 0.186 | 0.633 | ||
| N | 92 | 93 | 93 | 93 | 93 | 93 | 93 | 91 | 91 | 90 | 93 | 91 | 92 | |
| Classification (Sanders) | Rs | -0.272** | 0.325** | 0.281** | 0.185 | 0.285** | 0.596** | 0.039 | 1 | 0.352** | 0.314** | 0.274** | 0.132 | 0.309** |
| Sig. | 0.008 | 0.001 | 0.006 | 0.072 | 0.005 | 0 | 0.714 | 0 | 0.002 | 0.007 | 0.206 | 0.002 | ||
| N | 94 | 95 | 95 | 95 | 95 | 95 | 91 | 95 | 94 | 92 | 95 | 93 | 94 | |
| Classification (Eastwood/ Atkins) | Rs | -0.433** | 0.421** | 0.099 | 0.072 | 0.069 | 0.257* | 0.089 | 0.352** | 1 | 0.340** | 0.144 | 0.055 | 0.222* |
| Sig. | 0 | 0 | 0.338 | 0.488 | 0.507 | 0.012 | 0.399 | 0 | 0.001 | 0.165 | 0.602 | 0.032 | ||
| N | 95 | 95 | 95 | 95 | 95 | 95 | 91 | 94 | 95 | 92 | 95 | 93 | 94 | |
| Soft tissue | Rs | -0.182 | 0.054 | 0.035 | 0.098 | 0.1 | 0.19 | 0.088 | 0.314** | 0.340** | 1 | 0.298** | 0.162 | 0.317 |
| Sig. | 0.076 | 0.6 | 0.733 | 0.337 | 0.329 | 0.063 | 0.411 | 0.002 | 0.001 | 0.003 | 0.117 | 0.002 | ||
| N | 96 | 97 | 97 | 97 | 97 | 97 | 90 | 92 | 92 | 97 | 97 | 95 | 96 | |
| Fracture line CCJ | Rs | -0.204* | 0.147 | 0.446** | 0.046 | 0.316** | 0.440** | 0.122 | 0.274** | 0.144 | 0.298** | 1 | 0.454** | 0.939** |
| Sig. | 0.043 | 0.143 | 0 | 0.651 | 0.001 | 0 | 0.244 | 0.007 | 0.165 | 0.003 | 0 | 0 | ||
| N | 99 | 100 | 100 | 100 | 100 | 100 | 93 | 95 | 95 | 97 | 100 | 98 | 99 | |
| Central defect | Rs | -0.206* | 0.387** | 0.318** | 0.169 | 0.207* | 0.284** | 0.14 | 0.132 | 0.055 | 0.162 | 0.454** | 1 | 0.386** |
| Sig. | 0.043 | 0 | 0.001 | 0.096 | 0.041 | 0.005 | 0.186 | 0.206 | 0.602 | 0.117 | 0 | 0 | ||
| N | 97 | 98 | 98 | 98 | 98 | 98 | 91 | 93 | 93 | 95 | 98 | 98 | 97 | |
| Classification (CCJ) | Rs | -0.224* | 0.158 | 0.500** | 0.123 | 0.253* | 0.497** | 0.05 | 0.309** | 0.222* | 0.317** | 0.939** | 0.386** | 1 |
| Sig. | 0.027 | 0.119 | 0 | 0.225 | 0.011 | 0 | 0.633 | 0.002 | 0.032 | 0.002 | 0 | 0 | ||
| N | 98 | 99 | 99 | 99 | 99 | 99 | 92 | 94 | 94 | 96 | 99 | 97 | 99 | |
Table 4: Associations between the most important parameters analyzed, displayed in a correlation matrix. Showing spearman’s rank correlation coefficient Rs and level of significance.
Table 5 displays a contingency table showing the association between the extension of the primary fracture line into the CCJ and the number of facets involved, Zwipp and Sanders classifications. Overall fracture classification was found to be more severe (e.g. 9-12 points on the Zwipp scale) the more medial the primary fracture line extended into the CCJ (Spearman Rank Correla-tion Coefficient rs=0.386, p=0.004).
| Extension of primary fracture line into CCJ / No facets involved. Zwipp and Sanders’ Classifications | Lateral Third | Middle Third | Medial Third | Spearman Correlation Coefficient [rs(p)] |
|---|---|---|---|---|
| Facets involved | 0.3 | |||
| (<0.05) | ||||
| 1 | 0 | 0 | 0 | |
| 2 | 6 | 10 | 1 | |
| 3 | 8 | 14 | 7 | |
| 4 | 1 | 3 | 3 | |
| Zwipp Classification | 0.426 | |||
| -0.01 | ||||
| 0-5 points | 0 | 0 | 0 | |
| 6-9 points | 10 | 13 | 2 | |
| 10-12 points | 5 | 14 | 9 | |
| Sanders’ Clacssification | 0.396 | |||
| -0.01 | ||||
| Typ I | 0 | 0 | 0 | |
| Typ II | 10 | 14 | 2 | |
| Typ III | 3 | 11 | 6 | |
| Typ IV | 2 | 1 | 2 | |
Table 5: Contingency table: association between the extension of the primary fracture line into the CCJ and the no. of facets involved, Zwipp and Sanders classifications
No clear association, however, was found between the orientation of the fracture line and fracture classification (Zwipp scale; Spearman Rank Correlation Coefficient rs=0.122, p=0.233)
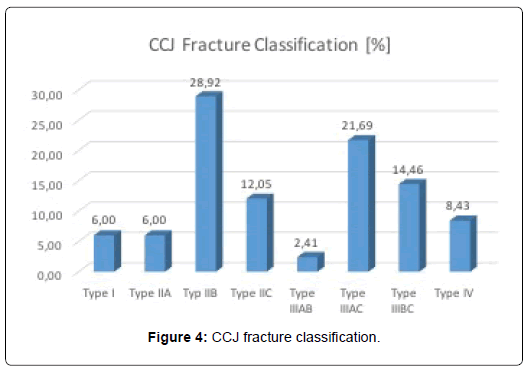
Finally, a classification of the CCJ involvement is proposed. Figure 4 shows the distribution of the fractures according to this system. We found a significant correlation of the CCJ fracture classification and Sanders, or Zwipp Classifications (Table 4).
Discussion
Epidemiological data on calcaneocuboid joint involvement in intraarticular calcaneal fractures is scarce. This retrospective radiographic evaluation sought to describe calcaneocuboid joint involvement in more detail than previous studies, including our own [3]. CCJ involvement was 84 % in this study. In a prior study, we reported 68% [3]. Other studies reported a lower incidence ranging from 33% to 76% [1,9-14,4]. The higher incidence in comparison to other studies might be explained by the fact, that only intraarticular calcaneal fractures were included into this study. In contrast to other studies we included all fractures involving the CCJ, even if non-displaced (also in contrast to own our previous study [3]). Furthermore, the reported incidences are based on different diagnostic algorithms. Not all studies included routinely CT-scans with multiplanar reformations to evaluate calcaneal fractures. Most studies lack to define CCJ involvement exactly. Last but not least, there were more Sanders type III and IV fractures in our cohort compared to other studies [4,15].
Up to now fracture anatomy of the anterior apophyseal region of the calcaneus and the calcaneocuboid joint is only partially understood and most classification systems disregard CCJ involvement. Therefore, we provided a detailed analysis of fracture morphology.
As we could show CCJ involvement was associated to more severe trauma, resulting in a significant higher Zwipp or Sanders classification. This has partially been shown previously [3,16].
Ebraheim et al. described the correlation between joint depression type fracture and calcaneocuboid involvement [1]. Our data confirmed also this finding.
These (more severe) fractures were also more likely to be displaced (Spearman rank correlation coefficient, rs=0.512, p<0.001) and presented either with a vertical fracture line, an oblique fracture line extending from super-lateral to inferior-medial, or a multifragmentary situations. These typical extension of fracture lines into the CCJ may be explained by the proposed typical patho mechanisms with the talus acting as an “axe” during the vertical impact and producing a more or less vertical fracture line, that runs more medially with more varus position of the foot during impact [17,18]. We could also show that a more severe fracture, defined by a higher Sanders of Zwipp classification, was associated with a more medial extension of the primary fracture line into the CCJ. This compares to the findings of Silhanec et al. [4].
Sanders classification itself, however, is inapplicable to classify CCJ involvement, since only subtalar joint involvement is assessed [19].
We therefore proposed a classification system for CCJ involvement, based on our descriptive data. During analysis, we could show a reasonable correlation between our own CCJ classification and Sander’s Classification for calcaneal fractures. Significant correlations were also seen for Bohler’s angel, number of facet involved, degree of displacement, Zwipp classification and size of the central defect (Table 3).
Future studies must show, if the proposed classification system has any impact on the treatment and outcome of calcaneal fractures. Moreover, intra and interobserver reliability have to be tested. Last but not least, this additional classification system has to show, if it is applicable in daily routine.
In the light of outcome measurements, we concluded in a prior study, that CCJ involvement should be given more credit during surgery and in our research efforts [3]. Therefore, an accurate radiological analysis is indispensable.
Limitations of this study include a not always optimal imaging, which is especially true for the coronal reformations, resulting in images that could not be included for analysis. Even if trained on a regular basis, secondary reformations of the original data-set were not always satisfactory.
Moreover, we have to take into account a low inter- and intraobserver reliability. Roll et al. could show that the extension into the CCJ was evaluated correctly only in 49% [20].
Conclusion
Our results suggest that calcaneocuboid joint involvement is more common than previously published and associated with more severe calcaneal fractures, as shown by Sanders and Zwipp classifications. Typical fracture patters can be expected, facilitating planning for surgical reduction and fixation. A classification of CCJ involvement may support our efforts towards a better understanding of fracture pathology.
Conflicts of Interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of the article “Calcaneocuboid Joint Involvement in Calcaneal fractures–CT Based Analysis and Classification”.
References
- Ebraheim NA, Biyani A, Padanilam T, Christiensen G (1996) Calcaneocuboid joint involvement in calcaneal fractures. Foot Ankle Int 17: 563-565.
- Ebraheim NA, Haman SP, Lu J, Padanilam TG (1999) Radiographic evaluation of the calcaneocuboid joint: a cadaver study. Foot Ankle Int 20: 178-181.
- Kinner B, Schieder S, Muller F, Pannek A, Roll C (2010) Calcaneocuboid joint involvement in calcaneal fractures. J Trauma 68: 1192-1199.
- Silhanek AD, Ramdass R, Lombardi CM (2006) The effect of primary fracture line location on the pattern and severity of intraarticular calcaneal fractures: A retrospective radiographic study. J Foot Ankle Surg 45: 211-219.
- Zwipp H, Baumgart F, Cronier P, Jorda E, Klaue K, et al. (2004) Integral classification of injuries (ICI) to the bones, joints, and ligaments: Application to injuries of the foot. Injury 35: 3-9.
- Kinner BJ, Best R, Falk K, Thon KP (2002) Is there a reliable outcome measurement for displaced intra-articular calcaneal fractures? J Trauma 53: 1094-1101.
- Andermahr J, Jesch AB, Helling HJ, Jubel A, Fischbach R, et al. (2002) CT morphometry for calcaneal fractures and comparison of the Zwipp and Sanders classifications. Z Orthop Ihre Grenzgeb 140: 339-346.
- Bajraliu M, Walley KC, Kwon JY (2016) Rationale for the hypodense calcaneal region of ward’s neutral triangle. Orthop J Harv Med Sch 17: 63-67.
- Gupta A, Ghalambor N, Nihal A, Trepman E (2003) The modified Palmer lateral approach for calcaneal fractures: wound healing and postoperative computed tomographic evaluation of fracture reduction. Foot Ankle Int 24: 744-753.
- Linsenmaier U, Brunner U, Schoning A, Rieger J, Krotz M, et al. (2003) Classification of calcaneal fractures by spiral computed tomography: Implications for surgical treatment. Eur Radiol 13: 2315-2322.
- Hutchinson F, Huebner MK (1994) Treatment of os calcis fractures by open reduction and internal fixation. Foot Ankle Int 15: 225-232.
- Kurozumi T, Jinno Y, Sato T, Inoue H, Aitani T, et al. (2003) Open reduction for intra-articular calcaneal fractures: Evaluation using computed tomography. Foot Ankle Int 24: 942-948.
- Stephanson JR (1987) Treatment of displaced intra-articular fractures of the calcaneus using medial and lateral approaches, internal fixation, and early motion. J Bone Joint Surg Am 69: 115-130.
- Zwipp H, Rammelt S, Barthel S (2004) Calcaneal fractures: Open reduction and internal fixation (ORIF). Injury 35: 46-54.
- Cao L, Peng Y, Yan R, Wang H (2013) Surgical treatment of calcaneal fracture involving talocalcaneal and calcaneocuboid joints. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 27: 169-172.
- Miric A, Patterson BM (1998) Pathoanatomy of intra-articular fractures of the calcaneus. J Bone Joint Surg Am 80: 207-212.
- Burdeaux BD (1983) Reduction of calcaneal fractures by the McReynolds medial approach technique and its experimental basis. Clin Orthop Relat Res 177: 87-103.
- Carr JB (1993) Mechanism and pathoanatomy of the intraarticular calcaneal fracture. Clin Orthop Relat Res 290: 36-40.
- Sanders R, Fortin P, DiPasquale T, Walling A (1993) Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res 290: 87-95.
- Roll C, Schirmbeck J, Schreyer A, Muller F, Neumann C, et al. (2011) How reliable are CT scans for the evaluation of calcaneal fractures? Arch Orthop Trauma Surg 131: 1397-1403.
Citation: Roll C, Zwicker K, Kinner B (2018) Calcaneocuboid Joint Involvement in Calcaneal Fractures-CT Based Analysis and Classification. Clin Res Foot Ankle 6: 278. DOI:
Copyright: © 2018 Roll C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 5667
- [From(publication date): 0-2018 - Apr 06, 2025]
- Breakdown by view type
- HTML page views: 4903
- PDF downloads: 764