Research Article Open Access
C-Reactive Protein-The Most Useful Marker in Rheumatoid Arthritis
Spasovski D1* and Sotirova T21Department of Rheumatology, University Clinical Centre, Skopje, Republic of Macedonia, Roman, Italy
2Department of Hematology, University Clinical Centre, Skopje, Republic of Macedonia, Roman, Italy
- *Corresponding Author:
- Dejan Spasovski
Department of Rheumatology, University Clinical Centre
Skopje, Republic of Macedonia, Rome, Italy
Tel: +389023147147
E-mail:drspasovski@yahoo.co.uk
Received date: November 04, 2014; Accepted date: December 06, 2014; Published date: December 10, 2014
Citation: Spasovski D and Sotirova T (2014) C-Reactive Protein-The Most Useful Marker in Rheumatoid Arthritis. Interdiscip J Microinflammation 1:120. doi: 10.4172/2381-8727.1000120
Copyright: © 2014 Spasovski D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at International Journal of Inflammation, Cancer and Integrative Therapy
Abstract
Aim: The aim of the study was to determine the most useful biochemical marker of the acute phase reactants for evaluation of disease activity in rheumatoid arthritis (RA).
Material and methods: 60 patients with RA were included, 27 of them treated with non-steroid anti-inflammatory drugs (NSAIDs) and Methotrexate (MTH). The control group consisted of 33 patients treated only with NSAIDs due to irregular control. In the first group disease activity was evaluated in four time intervals and in the control group in three time intervals, following the scores of the articular indices, complete blood count (CBC), elevated sedimentation rate (ESR) and C-reactive protein (CRP) in every patient.
Results: In the first group of patients decreased activity of RA was found in every subsequent control, with consecutive decrease in the mean values of the scores of the articular indices with statistically significant differences in the four time intervals. Considering laboratory parameters there were statistically significant differences in the mean values of hemoglobin (Hb), erythrocytes (Er), platelets (Plt), ESR (p=0.0462, p=0.0076, p= 0.0058, p= 0.0003). Mean values of CRP did not show statistically significant differences, but the number of patients who were CRP negative increased (standard deviation increased, also). In the group of patients treated only with NSAIDs, there were statistically significant differences in the mean values of the scores of the articular indices with increase in every subsequent control (in favour of disease progression). There were not statistically significant differences considering CBC, ESR and CRP (in favour of permanently active disease).
Conclusion: CRP is the most useful marker in the prospective evaluation of patients with rheumatoid arthritis.
Keywords
Rheumatoid arthritis; Articular indices; Reactants of the acute phase
Introduction
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease with peripheral synovitis and progressive and unpredictable evolution resulting in joint failure. Beside the joints, disease affects multiple organs and systems. The quantification of the joint inflammation is very important in disease evaluation. Several articular indices were developed in order to standardize the clinical measurement of the joint inflammation [1,2]. Systemic involvement is accompanied by laboratory abnormalities such as increased ESR, anemia, thrombocytosis and elevated values of the liver function tests. The cause for anemia in RA is multifactorial. It is related to the degree of disease activity and not with its duration, and is one of the indicators of the RA activity. The degree of anemia in RA correlates with the disease activity, especially with degree of the joint inflammation. Usually anemia is normocytic and normochromic, except when it is accompanied by other disorders such as bleeding, wrong diet, concomitant infection or hemolytic anemia (in some patients due to antibodies), and most commonly induced by drugs which suppress bone marrow. Iron deficiency could be a reason for anemia in RA. Iron replacement therapy could be disappointing with inadequate therapeutic effect, because anemia in RA is caused by the inhibition of the hemoglobin synthesis due to inflammation. Thrombocytosis is the common finding in active RA. The degree of thrombocytosis correlates with the number of the involved joints with active synovitis as well as with the extra-articular disease manifestations. The mechanism of thrombocytosis is unknown. It is supposed that increased intravascular coagulation with compensatory increased production of platelets could be a possible reason. Thrombocytosis in RA do not correlate with the neoplastic changes in bone marrow. Thrombocytopenia in RA is a rear finding and could be caused by drug therapy or is found in Felty’s syndrome. The cause for thrombocytopenia in RA could be inhibitors of coagulation or more rarely hyperviscosity. Other indicators often used are the reactants of the acute phase such as ESR, increased according to the disease activity, as well as CRP as better indicator of the disease activity and progression in relation with ESR [3-5].
Aim
The aim of this study is quantify RA activity in time intervals, following the scores of two different articular indices (set of 28 sensitive and set of 28 swollen joints), laboratory parameters (Hb, Hct, Er, WBC, Plt ) and the reactants of the acute phase (ESR and CRP) in patients treated with Methotrexate (MTX) versus control group (without immunomodulatory drugs), and to determine which of the reactants of the acute phase is the most useful biochemical marker for the evaluation of disease activity in RA.
Material and Methods
In this prospective control study were included 60 patients with RA. These patients fulfilled criteria of disease classification according to the American College of Rheumatology from 1987 [6]. 27 patients were treated with NSAIDs and MTH, mean dose 7.5 mg once weekly. Patients mean age was 50.3 ± 8.9 years (range 33-72 years), mean disease duration was 3.1 ± 1.3 years (range 1-5 years). The control group consisted of 33 patients who were incidentally treated with NSAID due to irregular control, with mean age 55.4 ± 8.3 (range 37-73 years) and mean disease duration 4.3 ± 2.4 years (range 1-9 years ).
Inclusion criteria: patients with RA, age 18-73 years, newly diagnosed and not treated.
Exclusion criteria:
1. Patients with RA age<18 years.
2. Patients with SLE, Sy Sjögren, uric arthritis, mixed conjunction tissue disease, vasculitis.
3. Patients treated with antibiotics and salicylates in period less than six months from the beginning of the study.
4. Patients who take drugs from basic line.
5. Patients with previous medical history for diseases of the spleen and thyroid gland, hepatic, renal, hematologic, cardiovascular, neurologic and lung failure, autoimmune disease, AIDS, diabetes mellitus, malignant disease, febrile conditions, arterial hypertension.
6. Patients treated with antihypertensive, antidiabetic and cardiac therapy.
7. Hypersensitive to some drugs or their components.
8. Patients with previous history of blood transfusion and overweight.
9. Patients whose results show glycemia in 0 spot or increased level of degraded products: serum urea and creatinine, urine creatinine and hematologic and enzymatic disturbance.
All patients voluntarily took part in the study, so the ethical criteria were fulfilled.
Clinical Evaluation of Disease Activity
RA was quantitatively evaluated in every patient according to the changes of the articular indices score, laboratory measurements - CBC and reactants of the acute phase–ESR, RF, CRP in certain time intervals. In the first group of patients RA was quantitatively evaluated in 4 time intervals: 0-time, after 1, 2, and 3 years. In the control group of patients disease was quantitatively evaluated in 3 intervals of time: 0-time, after 1 and 2 years.
For the quantitative evaluation of the joint inflammation two different articular indices were used: set of 28 palpation painful, sensitive and set of 28 edematous, swollen joints. These artucular indices evaluate set of 28 joints with score from 0 to 1 separately for the joint sensitivity and the joint edema. Their sum gives the cumulative index of the joint inflammation range 0–28 [7-10].
Laboratory Assessment
Every patient was evaluated in determined time intervals for complete blood analysis-CBC with differential, reactants of the acute phase-ESR (mm/1 hour) according to the Westergreen method with reference values 4/10; CRP determined with immunonephelometric method, with reference values 0.0-0.6 mg/l. Values>6 mg/l signify positive CRP. Rheumatoid factor (RF) was detected with Latex RF test, reference values>8 mg/l in serum. Liver function tests: AST, ALT, AP, LDH, CPK and creatinine in serum and urine.
Statistical Analysis
Data analysis were performed using: analysis of the structure of the numerical data with measures of the central tendency (mean values) and measures of dispersion (standard deviation), analysis of correlation between attributive series is made with χ² test, determination of the significance among three or more arithmetical means in the groups (dependant samples) was done with Freedman’s two-directional analysis of variance.
Results
Quantitative evaluation of RA activity in patients treated with MTX is shown in Table 1. Freedman’s two-directional analysis of variance showed statistically significant differences among mean values of the score on the set of 28 tender joints (DAS28 sensitivity) in four time intervals (Fr χ²=12.205 p=0.000001), as well as among mean values of the articular index on the set of 28 tender and swollen joints (Fr χ²=10.262 p=0.00006) in favor of decrease of articular indices score in every subsequent control, due to the decreased joint inflammation. There were statistically significant differences among mean values of ESR in all four time intervals (Fr χ²=15.161 p=0.0003) in favor of decreased mean values of ESR in the subsequent controls. Among mean values of CRP in the four time intervals there were not statistically significant differences (Fr χ²=2.094 p=0.1056); standard deviations showed great variations. Analysis of the χ² test showed that patients in whom the values of CRP were negative in the course of time increased, and the differences were statistically significant (χ²=17.35 df=3 p=0.00059).
| Time interval | M±SD) set of 28 painfull joints |
M±SD) set of 28 swolen joints |
(M±SD) ESR | (M±SD) CRP |
(M±SD) PLT |
|
|---|---|---|---|---|---|---|
| MTX group |
0-spot | 12.8 ± 5.7 | 6.5 ± 3.1 | 78.4 ± 30.6 | 30.8 ± 47.1 | 311.4±105.4 |
| 1 year | 8.1 ± 5.4 | 3.6 ± 3.1 | 47.2 ± 28.2 | 14.3 ± 21.8 | 272.8 ± 84.5 | |
| 2 year | 5.6 ± 5.2 | 2.6 ± 2.5 | 37.3 ±19.2 | 8.3 ± 9.1 | 236.1 ± 77.1 | |
| 3 year | 6.7 ± 5.4 | 3.5 ± 2.1 | 36.6±24.2 | 26.4 ± 51.3 | 238.3±61.7 | |
| MTX+ NSAIDsgroup |
0-spot | 4.1 ± 5.2 | 8.3 ± 3.1 | 58.7 ± 16.8 | 32.2 ± 15.3 | |
| 1 year | 15.7 ± 5.3 | 8.7 ± 3.7 | 69.1± 14.3 | 41.4 ± 16.7 | ||
| 2 year | 17.5 ± 4.1 | 8.8 ± 2.7 | 65.5 ± 21.6 | 49.8 ± 16.2 |
Table 1: Quantitative evaluation of RA activity in patients treated with Metotrexate and in control patients (without Metotrexate).
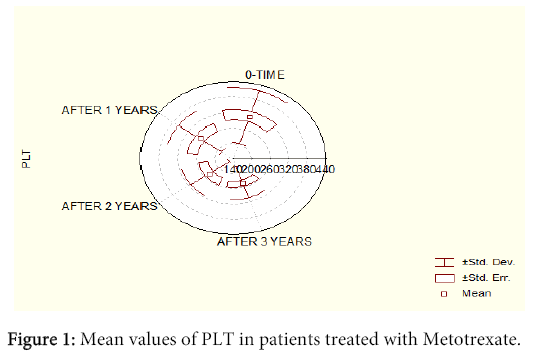
Freedman’s two-directional analysis of variance showed statistically significant differences among mean values of Hb (Fr χ²=2.756 p=0.0462), mean values of Er (Fr χ²=4.199 p=0.0076), with increase in the mean values of Hb and Er in the subsequent controls. Among mean values of Hct in this group there was not statistical increase in the four time intervals (Fr χ²=4.353 p=0.0063) in favour of correction of anemia. Differences in the mean values of WBC were not significant (Fr χ²=0.6807 p=0.5658). Considering platelets Freedman’s two-directional analysis of variance showed that there were statistically significant differences among mean values (Fr χ²=4.418 p=0.0058), in favor of correction of thrombocytosis (Figure 1). Quantitative evaluation of RA activity in the control group (without MTX) is shown in Table 1. Freedman’s two-directional analysis showed that there were statistically significant differences among mean values of the score in the set of 28 painful, tender joints (Fr χ²=4.214 p=0.0176), in favor of elevated values in every subsequent control. Considering the mean values of the score in the set of 28 swollen joints statistical analysis did not show statistically significant differences (Fr χ²=0.242 p=0.7851), they were in all time intervals almost identical, which spoke in favor of constant disease activity.
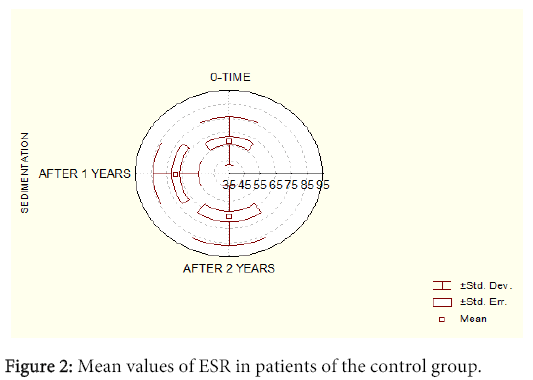
There were not statistically significant differences neither in ESR in all three time intervals (Fr χ²=2.807 p=0.0625), in favor of constantly increased high values and disease activity (Figure 2). There were not statistically significant differences nor in the mean values of CRP in the three time intervals (standard deviations showed great variations). χ² test analysis showed that patients in whom the values of CRP were negative did not change in the course of time, so the differences were not statistically significant (χ²=0.57 df²=p=0.752). There were not statistically significant differences among mean values of Hb (Fr χ²=1.82 p=0.165), mean values of Er (Fr χ²=0.020 p=0.997), mean values of WBC (Fr χ²=0.319 p=0.727), mean values of Hct (Fr χ²=1.085 p=0.341) and mean values of Plt (Fr χ²=0.257 p=0.773) in the three time intervals. All parameters in this group of patients showed increased activity of RA and disease progression.
Discussion
RA disease activity evaluation is very importance in everyday practice, as well is for the clinical investigations. The disease presentation varies significantly among patients, as well as in the same patient. Considering the heterogeneous presentation of disease and variable course among different individuals, it is impossible to evaluate the disease activity on the base of one variable/measure.
In the previous decades numerous measurements were used in the clinical investigations for quantification of different aspects of disease and for more complete evaluation of the disease activity such as clinical evaluation of the inflammation with articular indices [11], laboratory measurements for detection of anemia and thrombocytosis as parameters which show increased disease activity, as well as biochemical parameters that indirectly reflect synovitis, such as reactants of the acute phase. ESR and CRP are sensitive indicators for measurement of the immune-mediated inflammatory response. All these measurement are standardized and have potential for disease quantification. Considering the variability of all of these measurements for the reliable evaluation of the RA activity, it is important an individual monitoring of each one in certain time intervals [12,13].
A lot of rheumatologists think that MTX is a drug of choice, most convenient for long-term treatment of RA. A lot of clinicians think that MTX is superior in comparison with other DMARDs. Inhibition of the DNA synthesis and the inhibitory effect on cell proliferation, on the activity of lymphocytes and neutrophils, as well as suppressive activity of cytokines are the most important mechanisms of action of MTX in the treatment of RA. It has an impact on the modification of the course of disease, improves the signs and symptoms of the inflammatory synovitis, prevents and decreases the rate of the joint erosion progression, all that contributing for function maintenance. Early treatment of RA with MTX is of great importance for reaching maximal treatment efficacy, disease remission and better treatment response.
The results of this study are similar to other studies for early RA, considering the mean values of the set of 28 painful, tender joints and set of 28 swollen joints and laboratory parameters. Differences are caused by variations in the number of patients and disease activity in the beginning of the study [14]. Following all the previously exposed measurements in patients of the control group who were incidentally treated with NSAIDs it was possible to evaluate the natural course of disease, which is unpredictable, progressive and individual. On the contrary, the group of patients treated with MTX, in whom disease suppression was achieved, clinically presented with decrease in the mean values of the scores in the two articular indices, with laboratory parameters (correction of anemia and thromocytosis), as well as reactants of the acute phase (with decrease in the values of ESR in the subsequent controls and increase in the number of patients who were CRP negative).
There are other studies which confirm the association of these two parameters, but they are cut-off studies with smaller number of patients [15,16]. They also emphasize the benefit of CRP as the most useful biochemical marker in the evaluation of the disease activity.
Nowadays the most of the rheumatologists strongly recommend early introduction of MTX in the treatment of RA. But, even early MTX treatment can not stop complete disease progression in certain patients, and what is more important the term early is under discussion [17,18].
Quantitative evaluation of disease activity by those measurements enables assessment of the actual patient’s condition and also helps clinicians to be more effective in treatment modification.
Conclusion
CRP is the most useful marker in the prospective follow-up of RA patients.
References
- Pincus T Strand V, Koch G, Amara I, Crawford B, et al. (2003) An index of the three core data set patient questionnaire measures distinguishes efficacy of active treatment from that of placebo as effectively as the American College of Rheumatology 20% response criteria (ACR20) or the Disease Activity Score (DAS) in a rheumatoid arthritis clinical trial. Arthritis Rheum 48: 625-630.
- Pincus T, Amara I, Koch GG. (2005) Continuous indices of core data set measures in rheumatoid arthritis clinical trials: lower responses to placebo than seen with categorical responses with the American College of Rheumatology 20% criteria. Arthritis Rheum 52: 1031-6.
- Buchbinder R, Bombardier C, Yeung M, Tugwell P. (1995) Which outcome measures should be used in rheumatoid arthritis clinical trials? Clinical and quality-of-life measures' responsiveness to treatment in a randomized controlled trial. Arthritis Rheum 38: 1568-80.
- Ranganath VK, Elashoff DA, Khanna D, Park G, Peter JB, et al. (2005) Age adjustment corrects for apparent differences in erythrocyte sedimentation rate and C-reactive protein values at the onset of seropositive rheumatoid arthritis in younger and older patients. J Rheumatol 32: 1040-2.
- Wolfe F1 (1997) Comparative usefulness of C-reactive protein and erythrocyte sedimentation rate in patients with rheumatoid arthritis. J Rheumatol 24: 1477-1485.
- Arnett FC, EdworthySm, Bloch Da, McShane DJ, Fries JF, et al. (19987) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis.Arthritis Rheum 31:315-24.
- van Gestel AM Prevoo ML, van 't Hof MA, van Rijswijk MH, van de Putte LB, et al. (1996) Development and validation of the European League Against Rheumatism response criteria for rheumatoid arthritis. Comparison with the preliminary American College of Rheumatology and the World Health Organization/International League Against Rheumatism Criteria. Arthritis Rheum 39: 34-40.
- Prevoo ML, van't Hof MA, Kuper NH, van Leeuwen MA, et al. (1995) Modified disease activity scores that include 28-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44-8.
- Balsa A Carmona L, González-Alvaro I, Belmonte MA, Tena X, et al. (2004) Value of Disease Activity Score 28 (DAS28) and DAS28-3 compared to American College of Rheumatology-defined remission in rheumatoid arthritis. J Rheumatol 31: 40-46.
- Prevoo MLL, van Gestel AM, van't Hof MA, van Rijswijk MH, et al. (1996) Remission in a prospective study of patients with rheumatoid arthritis. American Rheumatology Association preliminary remission criteria in relation to the disease activity score. Br J Rheumatol 35:1101-5.
- Smolen JS Breedveld FC, Eberl G, Jones I, Leeming M, et al. (1995) Validity and reliability of the twenty-eight-joint count for the assessment of rheumatoid arthritis activity. Arthritis Rheum 38: 38-43.
- Hassell AB Davis MJ, Fowler PD, Clarke S, Fisher J, et al. (1993) The relationship between serial measures of disease activity and outcome in rheumatoid arthritis. Q J Med 86: 601-607.
- Anderson JJ Chernoff MC (1993) Sensitivity to change of rheumatoid arthritis clinical trial outcome measures. J Rheumatol 20: 535-537.
- Nell VP Machold KP, Eberl G, Stamm TA, Uffmann M, et al. (2004) Benefit of very early referral and very early therapy with disease-modifying anti-rheumatic drugs in patients with early rheumatoid arthritis. Rheumatology (Oxford) 43: 906-914.
- Kadir Y, Saliha K, Meltem AM, Gurhan G, Mahir U, et al. (2004) Associations between Acute Phase Reactant Levels and Disease Activity Score (DAS28) in Patients with Rheumatoid Arthritis. Annals of Clinical & Laboratory Science 34: 423-26.
- Matsui T, Kuga Y, Kaneko A, Nishino J, Eto Y, et al. (2006) Disease Activity Score 28 (DAS28) using C-reactive protein underestimates disease activity and overestimates EULAR response criteria compared with DAS28 using erythrocyte sedimentation rate in a large observational cohort of rheumatoid arthritis patients in Japan. Ann Rheum Dis 66: 1221-6.
- van der Heide A Jacobs JW, Bijlsma JW, Heurkens AH, van Booma-Frankfort C, et al. (1996) The effectiveness of early treatment with "second-line" antirheumatic drugs. A randomized, controlled trial. Ann Intern Med 124: 699-707.
- Hider SL, Buckley C, Silman AJ, Symmons DP, Bruce IN, et al. (2005) Factors influencing response to disease modifying antirheumatic drugs in patients with rheumatoid arthritis. J Rheumatol32: 11-16.
Relevant Topics
Recommended Journals
- Journal of Lung Cancer Diagnosis & Treatment
- Advances in Cancer Prevention
- Breast Cancer: Current Research
- Cancer Surgery
- Immunology: Current Research
- Current Trend in Gynecologic Oncology
- Journal of Cancer Diagnosis
- Journal of Gastrointestinal Cancer and Stromal Tumors
- Cervical Cancer: Open Access
- Journal of Mucosal Immunology Research
- Journal of Oncology Research and Treatment
- Journal of Orthopedic Oncology
- Journal of Prostate Cancer
- Research and Reviews on Pathogens
Article Tools
Article Usage
- Total views: 19918
- [From(publication date):
December-2014 - Jul 04, 2025] - Breakdown by view type
- HTML page views : 15301
- PDF downloads : 4617