Short Communication Open Access
Building a Comprehensive Tobacco Control Program at a Community Health System
Joanne H Ebner*, Catherine Brady-Copertino and Barry MeisenbergCancer Prevention, Anne Arundel Medical Center, Cancer Prevention, DeCesaris Cancer Institute, USA
- *Corresponding Author:
- Joanne H Ebner
Supervisor, Cancer Prevention
Anne Arundel Medical Center
Cancer Prevention
DeCesaris Cancer Institute, USA
Tel: 336-285-2247
Fax: 443-481-5808
E-mail: Jebner@AAHS.org
Received date: Mar 15, 2016; Accepted date: Mar 31, 2016; Published date: Apr 07, 2016
Citation: Ebner JH, Copertino CB, Meisenberg B (2016) Building a Comprehensive Tobacco Control Program at a Community Health System. J Comm Pub Health Nurs 2:117. doi:10.4172/2471-9846.1000117
Copyright: © 2016 Ebner JH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community & Public Health Nursing
Abstract
Strategies to discourage tobacco use on many fronts from taxation to hard-hitting awareness campaigns have made an impact on reducing tobacco use and promoting tobacco avoidance. In order to further advance tobacco control efforts, future efforts require expanded awareness campaigns; additional training for health professions in tobacco treatment; continued policy shifts; and further integration of tobacco treatment at all health care visits. Anne Arundel Health System’s Cancer Prevention/Nicotine Dependence Program is using several evidence-based tobacco control strategies to eliminate one of the most potent causes of death and disease. These broad efforts have been designed to engage wherever the health system can interact with the public: inpatients, outpatients, community health clinics, public housing, public schools, health system employee policy and public health policy at the state level. Community Cancer Centers can and should play a leading role in anti-tobacco efforts. Incorporating several elements of tobacco control within our organization and in the community allows us to further advance tobacco control efforts and enhance the health of the people we serve.
Introduction
Although adult smoking rates in the U.S. are at their lowest level since 1965 [1], cigarette smoking continues to plague the lives of millions of Americans accounting for 480,000 tobacco-related deaths per year and 14 million major medical conditions [2]. The estimated economic costs attributable to smoking and exposure to tobacco smoke are estimated to be $300 billion annually (direct medical costs of at least $130 billion and productivity losses of at least $150 billion) [2]. While the progress in tobacco control is encouraging, there are still pockets of populations where cigarette smoking remains high, notably, individuals with lower educational attainment; those who live below poverty level; African and Native Americans; the Lesbian Gay Bisexual and Transgendered (LGBT) communities and those who suffer from mental illness and substance abuse [3]. Tobacco related morbidity and mortality is a global concern as well. According to the World Health Organization, tobacco kills an estimated 6 million people. 80% of the estimated one billion smokers live in low- and middle-income countries where tobacco control efforts are not as well developed [4].
As new tobacco and nicotine products arise, efforts to drive down tobacco use must remain robust. Providing tobacco cessation counselling and treatment throughout the continuum of health care is an important strategy in the tobacco control effort. The process should begin at any place that a person enters the health care system. This article describes the multi-level tobacco-prevention and cessation efforts of a major regional community health care provider.
Setting. Anne Arundel Health System (AAHS) serves a population of over a million people across five Maryland counties. It consists of a 383 bed, acute care hospital with over 30,000 admissions and 90,000 emergency department visits yearly and a medical group with over 250 employed medical providers. Over 100,000 visits are performed annually.
The DeCesaris Cancer Institute provides the central planning and management for the health system’s public education, provider education, prevention, screening, treatment, and post-treatment programs. The Cancer Prevention Department is a component of the DeCesaris Cancer Institute and represents the prevention arm of the cancer care program.
The Cancer Prevention/Nicotine Dependence Team is comprised of a full-time Cancer Prevention Supervisor; two part-time registered nurses and one part-time health educator. All staff are certified Tobacco Treatment Specialists (TTS) through the Mayo Clinic Nicotine Dependence Program. Mayo Clinic’s TTS program is based on the tenets of the Association of the Treatment of Tobacco Use and Dependence (ATTUD) [5]. AAHS shares the goal of several professional organizations that guide quality and practice in cancer care including the National Comprehensive Cancer Network [6], American College of Surgeons. Committee on Cancer [7] and the American Society for Clinical Oncology [8] all of which call for integration of tobacco use assessment and treatment of tobacco dependence into the routine part of cancer care.
The Diagnosis
Tests conducted two years before her cancer showed that my wife had stones in her gull bladder. In 2013, in a business trip to Canada, after a meal with her colleagues, she felt severe pain in her abdomen which upon examination by x-ray turned out to be due to gull stones. The incident though painful did not repeat and no treatments were performed. A year later, in a visit to her primary doctor at the advice of her brother who had experienced rupture of the gull bladder, my wife asked that her gull stones be removed. The doctor ordered an x-ray that showed the stones but also, a shadow which was visible in her liver. The doctor who did not take the shadowy object seriously referred my wife to surgeon to remove the stones. At the same time, our neighbour, a radiologist when saw the x-ray, expressed concern and emphasized that we examine the liver further by CT-SCAN and MRI. The scans confirmed the presence of a diffuse tumor like tissue in the liver which prompted a biopsy examination. The diffuse tissue in question was not well defined which posed challenge in taking the biopsy sample. The result of the biopsy showed aggressive bile duct cancer. Our lives from the moment of this diagnosis was turned upside down. Next step was to remove the tumor as soon as possible before it invades the other organs. I assured my wife that” We’ll do whatever can be done and we’ll take you wherever there is the best treatment. I promised her that I believed a new tool “immunotherapy” was going to cure her.”
Inpatient Program
All hospitalized patients are screened for tobacco use upon admission with a tool embedded in the electronic medical record (EMR) (Epic, Verona, WI, USA). If the individual has a positive tobacco use history a “NO SMOKE” consult from either the physician or nurse is generated within the EMR. A daily report of currently hospitalized patients who have used tobacco within the previous year is also gleaned from the EMR based on the tobacco use assessment. Daily rounds are conducted by TTS to visit each patient identified as a tobacco user and provide bedside counselling, information and referral for tobacco cessation services. Depending on the individual’s readiness to quit, counselling may entail simply providing information and resources or include a 20 minute first counselling session. TTS visit over 250 patients per month. Patients are also encouraged to continue cessation efforts post discharge. Another priority of the nicotine dependence counselling visit is to ensure the comfort of the nicotine dependent patient’s abrupt cessation of tobacco while hospitalized by utilizing nicotine replacement therapies (NRT) and other available comfort strategies (deep breathing, cinnamon sticks, hard candy, etc.).
The AAHS is currently implementing a new initiative that would bridge tobacco cessation efforts that occur during hospitalization and tobacco abstinence post discharge. In addition to bedside counselling by the TTS, four weeks of the nicotine transdermal will be provided upon discharge. Patients will then receive follow up phone calls post discharge at 72 hours, one month, three months and six months. Outcomes such as quit rates, cigarette consumption, and readmission will be measured against the current standard of care which ends as bedside counselling and referral to a community based program. If successful, as measured by quit rates, cigarette consumption, and readmission rates, it would establish a new standard of care for hospitalized patients. The hope is that by extending tobacco treatment and cessation received as an inpatient to beyond discharge will streamline and improve tobacco cessation efforts, having a positive impact on community health.
Outpatient Services
Clients who are motivated to continue cessation efforts have a number of resources available to support them. Group tobacco cessation classes, and well as individual counselling are offered by AAHS. Group classes are evidence-based and pull from a variety of sources including the Mayo Clinic Nicotine Dependence Program, Legacy’s “Become An Ex” and the Maryland state sponsored MD Tobacco Quit Program [9]. Additional community resources such as the Tobacco Quit Line (1-800-Quit-Now) are also utilized as an adjunct or other programs or to accommodate specific individual needs. Five to six classes are held throughout the year with an average of 15 participants per class. Classes meet weekly in the evening for approximately 90 minutes for seven consecutive weeks. Each of the seven sessions addresses a unique topic associated with quitting tobacco (Table 1).
| Understanding nicotine addiction/habit |
| Building motivation: Formulating a plan to quit |
| Approaches to quitting, including tobacco cessation pharmaceuticals |
| “Quit day” preparation; Managing triggers and withdrawal symptoms |
| Panel discussion from recent “graduates” of the program |
| Stress Management, Weight Management and Physical activity |
| Planning ahead to avoid relapse; Overall recovery and support |
Table 1: Tobacco Cessation Class Elements.
The class also includes a medication clinic run by a Nurse Practitioner who is able to prescribe and advise individuals regarding tobacco cessation pharmaceuticals. The program is partially funded through the Cigarette Restitution Funds (CRF) grant available through the Anne Arundel County Department of Health in the state of Maryland [10]. After completion of the seven week course, individuals are followed at one month, three months, six months and 12 months to monitor progress, collect data on quit rates and provide additional guidance as needed. Quit rates vary depending on the individual’s commitment to attend all sessions and adherence to recommended tobacco cessation pharmaceuticals. 51% of all attendees competed all 7 classes for whom the overall quit rate is 38.5%. Ongoing individual counselling which utilize motivational interviewing techniques to help people overcome the ambivalence that comes with a major lifestyle change are offered The frequency and duration of the individual sessions is flexible based on the client’s needs. Quit rates at 12months for individual counselling is 28%.
Community Outreach
Disproportionate suffering from tobacco is seen in minority populations, particularly African Americans; the uninsured or underinsured; individuals who suffer from behavioural health or substance abuse issues (or both) [3]. In an effort to reach these populations, the Cancer Prevention Team has moved tobacco control programs into the community in a variety of settings.
Two Community Outreach Clinics serving as primary care medical homes for the underserved now host tobacco cessation efforts. One of these clinics located within a city owned senior housing building is home to elderly and disabled citizens. Many of the residents have several comorbidities often compounded by tobacco use and utilize emergency medical services at high rates. In 2012 the Housing Authority for the City of Annapolis began the process of implementing tobacco-free housing throughout city owned housing increasing the need for these programs.
Recognizing that residents who smoke need resources and support to quit, classes were held onsite in small groups and included the same components of the program held at the medical center. Clients were followed up in person and by phone. All participants in this voluntary program made a quit attempt, reducing overall consumption by half but quit success was not durable. Accordingly, a different approach was instituted. A certified TTS is now available in the clinic weekly for three hours to provide individual tobacco cessation counseling and medications to clinic clients.
In May of 2015 AAHS was host for “Clearing the Air: A Healthy Smoke-free HUD Housing Summit,” a consortium of public housing authorities, multifamily housing owners, management agents, and residents to learn about creating a healthier and safer environment by sharing expertise, experience and resources for reducing healthcare and property costs associated with smoking and environmental tobacco smoke. Nearly 300 participants attended the program. The Cancer Prevention Program is currently working with the City Housing Authority to expand programs to all city-owned multi-family housing facilities.
Programs in Behavioral Health
Tobacco use in individuals with co-occurring behavioral health or substance abuse issues results in disproportionately high tobaccorelated illness and premature death. Alcohol-dependent smokers are more likely to die from tobacco-related causes than from diseases associated with drug or alcohol consumption [11]. As a consequence, tobacco treatment is encouraged as part of the overall approach to treatment and wellness in mental health and substance abuse facilities. Randomized controlled studies evaluating tobacco treatment interventions for individuals with substance abuse problems found that smoking cessation interventions were associated with a 25% increased likelihood of long-term abstinence from alcohol and illicit drugs [12].
AAHS operates a substance abuse/behavioral health facility for adults and adolescents in which tobacco treatment is being incorporated into the standard of care for these individuals. The Cancer Prevention/Nicotine Dependence department developed an inpatient tobacco education program that has been integrated into the curriculum of the adult and adolescent inpatient program. Every other week, clients receive education regarding nicotine dependence and information about how tobacco cessation can be incorporated into their overall recovery treatment plan with practical information on how to initiate a quit plan and identify resources for “recovering” from nicotine dependence as well other substances.
School-based Prevention Programs
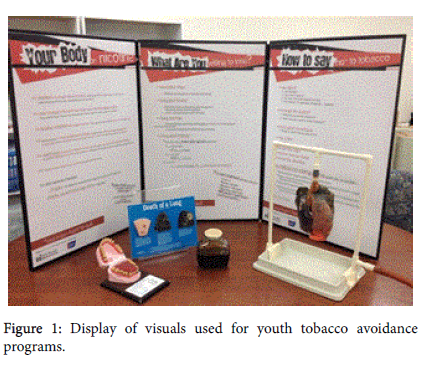
Avoiding the initiation of tobacco use is the ultimate goal of any tobacco control program. The importance of bringing that message to school-aged children in our community remains a priority. The “Teen Tobacco Road Show” was established in 2008 after receiving a Targeted Community Investment Grant through the American Cancer Society. The program is comprised of several components. A three-sided display (Figure 1) was developed, with input from the marketing department. It was designed to be visually appealing and educational to adolescents highlighting areas of nicotine addiction; the toll (physically and financially) of tobacco use; and techniques to resist tobacco initiation. Presentations are conducted during health or science classes to dovetail with current curriculum and are interactive and fast paced. They include compelling visuals such as “pig’s lungs” representing a healthy versus a “smoker’s” lung and a “tar jar” to show the amount of tar the lungs must process from smoking tobacco. The centerpiece of the presentation is the “age progression” software that allows the presenter to take photos of a handful of students, load them into the software then project two images of the student’s face onto the screen. One photo shows normal aging. The opposing photo illustrates aging as it occurs when one is smoking. The comparison is dramatic and appeals to the adolescent audience who relates more to the adverse cosmetic effects of smoking as opposed to the long term health consequences of smoking.
The nurse leader of the Tobacco Cessation Program also serves on the Youth Tobacco Access Task Force along with the County Department of Health; Police Department; School leaders and other stakeholders to help curb underage access to nicotine and tobacco products.
Engagement of the Larger Medical Community
Engaging other health professionals in the tobacco control effort is paramount in successfully reducing tobacco use. Several years ago a “Fax-to-Quit” (F2Q) program was initiated to encourage direct referrals for tobacco treatment from physicians and other health care providers. The F2Q form includes referral source information; client contact information and request to contact the patient. This process has enhanced physician engagement and allows the physician to seriously address tobacco dependence within the time constraints physicians face during office visits. From 2012-2014, 562 F2Q physician referrals were received. The next phase of the F2Q program is to transition to an electronic referral system via the EMR. Table 2 summarizes the activities of the various tobacco cessation and prevention programs.
| January 2012 - June 2015 |
| Total No. of inpatients counseled âÂ?Â? 11,031 |
| Total No. of outpatients counseled |
| Individually - 934 (Quit rate at 6 months: 28%) |
| Classes âÂ?Â? 1,654 (over 163 sessions) |
| Quit rate 38% one year out |
| Special Populations (Substance abuse. and/or Behavioral Health) âÂ?Â? 368 |
| AAHS Employees Counseled âÂ?Â? 62 |
| Adolescents (Tobacco Avoidance Program) - 737 |
Table 2: “Fast Facts” about Tobacco Prevention Programs.
Policy
Policy can be a powerful tool in preventing and reducing tobacco dependence. Research has shown that work policies that prohibit the use of smoking “not only protect non-smokers from the dangers of passive smoking; they also encourage smokers to quit or to reduce consumption” [13]. Accordingly, in 2014, AAHS elevated its antitobacco/ nicotine policy, initiating a strict tobacco-free (and vapingfree) campus where the use of any nicotine product is prohibited anywhere on campus including city-owned streets that run through the medical campus (FDA- approved nicotine replacement therapies are excluded). Figure 2 shows campous signage. In addition, in July 2015, AAHS became the first health system in Maryland to become a tobacco-free employer, prohibiting hiring of prospective employees if the individual tests positive for cotinine (a nicotine metabolite) on a pre-employment screening test. Our policy includes tobacco products in any form including electronic nicotine delivery devices, which are not currently regulated by the FDA.
While this policy generated controversy [14], the Health System felt it appropriate to join other health systems and businesses in other states without specific job protections for smokers in sending a clear message about the impact of tobacco and nicotine products on the public health. This type of policy also de-normalizes tobacco use, sending a clear message about the public health harms of tobacco use.
Advocacy
Cancer Prevention/Nicotine Dependence staff are involved in tobacco policy at the state and national level as well. They give input into the Maryland Comprehensive Cancer Control Plan developed by the Maryland Department of Health and Mental Hygiene with broad input from a partnership of public and private stakeholders. In summary, the Cancer Prevention/Nicotine Dependence program has been at the forefront of tobacco control efforts for health system patients, our community outside the hospital and clinics, the schools and for employees. The important role of partnerships and collaboration with physicians, government agencies and other public health partners cannot be overemphasized. Many of these programs would not be possible without the expertise, commitment, and resources that so many of the local, state and national organizations provide.
Despite this broad activity and partial success, there is still much work to do in eliminating the public health burden of tobacco. A critical factor in all tobacco treatment programs is the underlying understanding that tobacco abuse is a chronic, relapsing disease that requires on-going care and treatment adjustments. Our approach to all clients is that of non-judgmental and compassionate care in overcoming addiction. We urge community hospitals to forge similar coalitions to carry out this important work.
References
- Current Cigarette Smoking Among Adults in the United States (2014) Centers for Disease Control.
- Rostron BL, Chang CC and Pechacek TF (2014) Estimation of Cigarette Smoking–Attributable Morbidity in the United States. JAMA Intern Med 174:1922-1928.
- The Health Consequences of Smoking—50 Years of Progress (2016) A Report of the Surgeon General.
- World Health Organization (2015) Tobacco Fact Sheet.
- Association for the Treatment of Tobacco Use and Dependence (2016) ATTUD is an organization of providers dedicated to the promotion of and increased access to evidence-based tobacco treatment for the tobacco user.
- National Comprehensive Cancer Network (2015) NCCN Clinical Practice Guidelines: Smoking Cessation. Version 1.
- American College of Surgeons Commission on Cancer (2012) Cancer Program Standards: Ensuring Patient-Centered Care.
- American Society of Clinical Oncology. Guidelines for smoking/tobacco use.
- MDQUIT, Maryland’s Tobacco Resource Center (2016) MDQuit.org. Department of Health and Mental Hygiene.
- Cigarette Restitution Fund Program. Department of Health and Mental Hygiene.
- Hurt RD (1993) Treating nicotine addiction in patients with other addictive diseases. In CT Orleans, J Slade (eds.) Nicotine Addiction: Principles and Management. New York: Oxford University Press.
- Prochaska JJ (2010) Failure to treat tobacco use in mental health and addiction treatment settings: A form of harm reduction? Drug Alcohol Depend110: 177-182.
- Fichtenberg CM, Glantz SA (2002) Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ 325:188.
- Mirabella L (2014) In Maryland smoking could cost you your job: Controversial hiring policy is legal and growing in much of United States. The Baltimore Sun.
Relevant Topics
- Chronic Disease Management
- Community Based Nursing
- Community Health Assessment
- Community Health Nursing Care
- Community Nursing
- Community Nursing Care
- Community Nursing Diagnosis
- Community Nursing Intervention
- Core Functions Of Public Health Nursing
- Epidemiology
- Epidemiology in community nursing
- Health education
- Health Equity
- Health Promotion
- History Of Public Health Nursing
- Nursing Public Health
- Public Health Nursing
- Risk Factors And Burnout And Public Health Nursing
- Risk Factors and Burnout and Public Health Nursing
Recommended Journals
- Epidemiology journal
- Global Journal of Nursing & Forensic Studies
- Global Nursing & Forensic Studies Journal
- global journal of nursing & forensic studies
- journal of community medicine& health education
- journal of community medicine& health education
- Palliative Care & Medicine journal
- journal of pregnancy and child health
Article Tools
Article Usage
- Total views: 10464
- [From(publication date):
May-2016 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 9604
- PDF downloads : 860