Brief Notes on Pure Obturator Dislocation of the Hip
Received: 15-Oct-2022 / Manuscript No. jhcpn-22-80952 / Editor assigned: 17-Oct-2022 / PreQC No. jhcpn-22-80952 / Reviewed: 31-Oct-2022 / QC No. jhcpn-22-80952 / Revised: 04-Nov-2022 / Manuscript No. jhcpn-22-80952 / Accepted Date: 10-Nov-2022 / Published Date: 11-Nov-2022 QI No. / jhcpn-22-80952
Abstract
Hip post-traumatic dislocation is a surgical emergency that is typically brought on by a high-energy trauma in a polytraumatized setting. Pure obturator hip dislocations are quite uncommon. It is regarded as an emergency, and a trained surgeon must address it within six hours in order to lower the danger of iatrogenic fractures and femoral head osteonecrosis. Here, we describe a case of a hip dislocation caused solely by the obturator muscle after a high-energy trauma. Under general anaesthesia, the patient received urgent closure reduction treatment. After two years, the functional and radiological findings were satisfactory and free of any avascular necrosis symptoms.
Keywords
Obturator; Dislocation; Hip post-traumatic
Introduction
One of the least common dislocations in traumatology is hip obturator dislocation, with only a few occurrences documented in the literature. The very specific architecture of the hip joint, one of the most congruent joints in the human body, can be used to explain this uniqueness. Numerous stabilisers, including muscles, capsulo-labral structures, and ligamentous structures, surround it. To dislocate the hip, high-energy trauma is required due to the congruency's high level of stability for this joint. Hip [1-5] dislocations is a rare occurrence in athletic training. The most frequent type of hip dislocation is posterior; obturator dislocations are rare, accounting for just 6% to 10% of all occurrences. Due to the significant risk of avascular necrosis, which might impact the prognosis and long-term functional outcomes, reduction must be completed within 6 hours. 6 Here, we provide the results of a case of a solitary obturator dislocation treated with a modality and a follow-up of two years.
Case Report
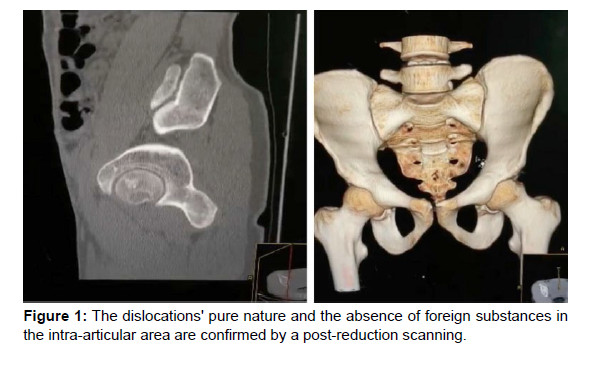
We discuss the case of a 23-year-old smoker who was the passenger in a car accident and who presented with no prior medical history. His left hip was in flexion, abduction, and external rotation upon evaluation (Figure 1), with no cutaneous opening present. The neurovascular examinations were normal, and a dermabrasion was found on the homolateral leg's inner side. A routine radiograph of the frontal pelvis revealed a right hip pure obturator dislocation without a fracture (Figure 1), a fractured femoral neck, or any other bone lesions. The patient was brought to the operating room at hospital H3 of the accident when it was determined that she had a pure obturator dislocation of the hip. A reduction via external manipulation was carried out while the patient was unconscious. The reduction was accomplished by pulling on the limb's axis, then bending the hip internally and abducting it and it was successful on the first try. Fluoroscopy and post-operative radiography proved the reduction (Figure 1). The hip was determined to be stable and in a concentric posture following assessment of post-reduction hip stability and neurovascular health. To rule out an intra-articular osteochondral fragment and to further evaluate the femoral head, a CT scan of the pelvis was performed. For two weeks, the limb was kept in traction to encourage capsulo-labral healing and lower intra-articular pressure. There was a non-weight-bearing post-operative procedure. Traction was withdrawn after two weeks, and light weight bearing was permitted. At six weeks, full weight bearing was accomplished. Three months after the reduction, sports activities were permitted. Serial radiographs were taken every three months for the first two years, then monthly, to monitor the patient's condition. The hip was stable and radiographs revealed no evidence of osteonecrosis after two years of follow-up.
Discussion
Hip flexion, abduction, and forceful external rotation are followed by obturator dislocation. 2 A similar instance was described in 2015 by Dellanh [6]. They noted that the most frequently reported mechanism is the shock wave's propagation from the medial side of a bent knee to the hip in flexed abducted and externally rotated position. The great trochanter's cam influence on the iliun in maximum abduction was emphasised by Toms et al. The orthopaedic reduction is crucial to the therapeutic therapy and is urgently needed. Like other writers, we insist on a reduction performed by an experienced surgeon under general anaesthesia with complete muscular relaxation. While Toms et al.7 recommend using an orthopaedic table and combining axial traction with lateral thigh traction, slowly releasing the traction while impregnating an addiction movement and internal rotation, Epstein and Wiss3 and Brav8 recommend traction in the axis of the femur followed by progressive flexion of the hip in internal rotation and abduction. Cases that are irreducible require open reduction using the ilioinguinal method. A case of an open reduction with rectus femoris muscle release was reported by Toms et al. In our situation, the procedure involved first applying traction to the limb's axis to enable decoaptation, then applying internal rotation to the limb's flexion to return it to extension adduction and internal rotation. We believe that this approach is more suitable in light of the femoral head's displacement in an obturator dislocation. Authors have opposed abduction because it can result in femoral neck fractures. The reduced challenges and large risk of problems that can result in a surgical approach for an open procedure are highlighted in these conversations. After reduction, it's important to [7-10] exclude out acetabulum anterior wall fractures; for this, a CT scan of the pelvis is particularly helpful. Additionally, it will enable the diagnosis of any femoral head osteochondrial lesions or an infra-radiological fracture that is usually linked to this kind of dislocation. These two factors will define the hip joint's functional prognosis, and the patient needs to be made aware of any issues. Theoretically, capsulo-labral healing could be aided by post-reduction traction for three to six weeks. A clinical benefit of its use on the long-term risk of avascular necrosis of the femoral head is not, however, supported by current studies. Catonné and co. In the case of anterior dislocations, it is advised to start off not bearing any weight and then add it back on completely on the fifteenth day. In 85% to 100% of cases, the course of an isolated hip dislocation is good. Necrosis of the femoral head and coxarthrosis are the two primary consequences. Delaying reduction raises the chance of femoral head avascular necrosis. When the reduction period was longer than 6 hours, Hougaard12 reported 47% necrosis. However, the majority of these statistics relate to lesions brought on by acetabulum or femoral head fractures. In isolated dislocations, this rate is unquestionably smaller.
Conclusion
The stability of the hip joint accounts for the rarity of obturator dislocation of the hip. Hip avascular necrosis can be avoided with early diagnosis and treatment within 6 hours. The patient must be given a detailed explanation of the post-reduction procedure and be made aware of any potential consequences.
Acknowledgements
The Department of Orthopedic Surgery and Traumatology at University Hospital Oujda in Morocco provided funding for this study. We thank the members of the Department of Orthopedic Surgery and Traumatology who contributed knowledge and insight that were extremely helpful to the study.
Declaration of conflicting interests
No potential conflicts of interest were disclosed by the author(s) with regard to the research, writing, or publication of this paper.
Ethical statement
I concur with the aforementioned claims and affirm that this submission complies with Solid State Ionics' policies as stated in the Ethical Statement and the Guide for Authors. There are no plans to publish the work elsewhere at the moment. The paper accurately and thoroughly reflects the authors' own research and analysis. The significant contributions of co-authors and co-researchers are duly acknowledged throughout the work. The findings are correctly positioned in relation to earlier and ongoing studies. All sources are duly acknowledged (correct citation). All authors have contributed significantly to the work that led to the paper, have been personally and actively involved in its production, and will accept public responsibility for its content. Literal copying of text must be identified as such by placing quotation marks around it and providing appropriate citation.
References
- Elouakili I, Ouchrif Y, Ouakrim R (2014) Luxation obturatrice de la hanche: un traumatismerare en pratique sportive. Pan African Med J 18: 138.
- Phillips AM, Konchwalla A (2000) The pathologic features and mechanism of traumatic dislocation of the hip. Clin Orthop Relat Res 7–10.
- Epstein HC, Wiss DA (1985) Traumatic anterior dislocation of the hip.Orthopedics8: 130–132.
- Hougaard K (1986) Traumatic posterior dislocation of the hip: prognostic factors influencing the incidence of avascular necrosis of femoral head. Arch Orthop Trauma Surg 106: 32–35.
- Wachtler B, Lampert T (2020) Digital divide-social inequalities in the utilisation of digital healthcare. Bundes gesundheitsblatt Gesundheitsforschung Gesundheitsschutz 63: 185-191.
- Bhavnani SP, Narula J, Sengupta PP (2016) Mobile technology and the digitization of healthcare. European heart journal 37: 1428-1438.
- Chen M, Decary M (2020) Artificial intelligence in healthcare: An essential guide for health leaders. In Healthcare management forum 33: 10-18.
- Kim HS, Yoon KH (2020) Lessons from use of continuous glucose monitoring systems in digital healthcare. Endocrinology and Metabolism 35:541.
- Belolipetskaya AE, Golovina TA, Polyanin AV (2020) Digital transformation of healthcare: a competency-based approach. Problems of Social Hygiene Public Health and History of Medicine 28: 694-700.
- Yang RS, Tsuang YH, Hang YS (1991) Traumatic dislocation of the hip. Clin Orthop 265: 218.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar , Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Agoumi O (2022) Brief Notes on Pure Obturator Dislocation of the Hip. J Health Care Prev, 5: 180.
Copyright: © 2022 Agoumi O. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1270
- [From(publication date): 0-2022 - Apr 28, 2025]
- Breakdown by view type
- HTML page views: 946
- PDF downloads: 324