Breast Tuberculosis: A Diagnosis Often Unknown: A Case Report
Received: 01-Nov-2017 / Accepted Date: 23-Nov-2017 / Published Date: 30-Nov-2017
Abstract
Breast tuberculosis is a rare condition. It poses a differential diagnosis problem with breast cancer because the clinic and imaging are not specific. Breast tuberculosis should be mentioned mainly in endemic countries or in immunocompromised individuals. We report a case of breast tuberculosis in a postmenopausal woman through this case, we describe the particularity clinical and evolving of this entity, and we discuss the diagnostic difficulties.
Keywords: Tuberculosis; Breast; Lymphadenopathy; Impregnation
Introduction
Tuberculosis has been gaining renewed interest for several years, mainly because of the resurgence of extrapulmonary forms in western and tropical countries, and in the Maghreb. This could be explained by the increasing of the prevalence of HIV infection, the emergence of strains of mycobacteria that are resistant to usual treatments, the immigration of populations from high rate of tuberculosis and the release of anti-tuberculosis campaigns [1].
The elective extrapulmonary localizations are, in order of decreasing frequency: the ganglia, the peritoneum, the pericardium, the kidneys, the skin, the joints, the meninges and the bone [1,2].
Breast localization is very rare, accounting for less than 0.1% of cases. Nearly 900 cases have been reported in the world literature [3,4]. This location can be primitive or secondary to locoregional tuberculosis or disseminated, and it often poses diagnostic difficulties both clinically and paraclinically [1-3].
The aim of our study is to make a clinical and therapeutic development on this rare pathology.
Case Presentation
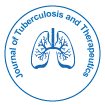
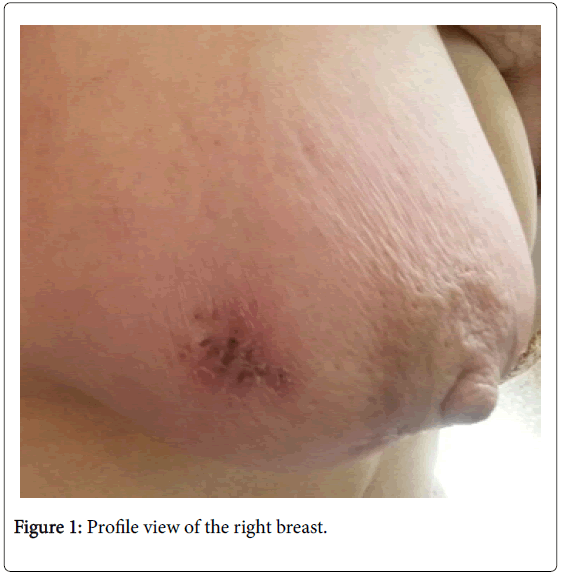
Mrs. G.N, 68 years old, multiparous, with no particular antecedents, in particular no concept of tuberculous contagion, who presented herself to our service for mastodynia appeared since two months. The clinical examination found a right inflammatory breast (Figures 1 and 2) with presence of homolateral axillary lymphadenopathies suggestive of breast cancer progressively advanced; the left breast was without abnormality the rest of the clinical examination also.
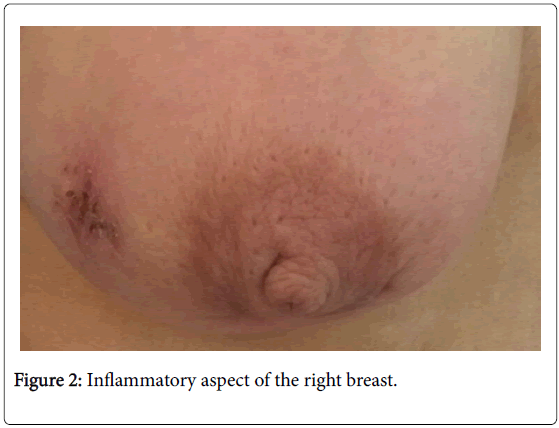
Mammography (Figure 3) showed an increase in right breast density with diffuse thickening of the soft tissues without nodular lesions or microcalcifications. Breast ultrasound revealed diffuse cutaneous thickening with an infiltrated aspect of the mammary tissues, especially in retro-areolar, associated with multiple hypoechogenic axillary lymphadenopathies, the largest of which was 32 mm × 16 mm. The lesion was classified as ACR 4. A cutaneous biopsy and a biopsy with the axillary lymphadenopathy were carried out; the anatomopathological examination objectified non-specific chronic fibro-inflammatory changes of the skin, and the presence of epitheliogiganto- cellular granuloma with caseous necrosis for the biopsy axillary lymphadenopathy. The diagnosis of tuberculous mastitis with associated ganglionic invasion was retained. The patient received antituberculous treatment with good clinical progression.
Discussion
Breast tuberculosis is a very rare form of tuberculosis. Its frequency varies from 0.06% to 0.1% of tuberculosis [5,6]. The rarity of this clinical form could be explained by the fact that breast tissue does not seem to be very conducive to the survival and multiplication of tubercle bacilli [7].
It essentially affects the young woman [8]. Pregnancy, lactation and multiparity are risk factors [9], which is explained by the effect of galactophoric ectasia during lactation.
Routes of infection are diverse [6] the lymphatic route or axillary lymphadenopathy is often found; hematogenous pathway, in the context of a miliary tuberculosis; propagation by contiguity from a neighborhood focus; The ductal: dilation of the galactophoric ducts in women during pregnancy or lactation increases the sensitivity of these ducts to infection with bacilli; The direct way: exceptional, it is the penetration of the bacillus of Koch in the breast following a cutaneous abrasion or galactophoric.
Classically, there are two types of breast tuberculosis: secondary with involvement of other organs and primary or tuberculosis appears strictly localized in the breast, the latter is the most common [7,10]. Concerning our patient the attack was primitive.
The attack is often unilateral and sits mainly at the level of the upper quadrant of the breast bilateral would be observed in only 3% of cases.
Clinically, mammary tuberculosis is characterized by the absence of specific clinical signs [9], whether in the form of a nodular mass or an inflammatory mass mimicking breast cancer. General signs of tuberculous impregnation (asthenia, anorexia, weight loss and vesperal fever) are classically present, but may be absent or incomplete.
However, there are clinical criteria that can lead to tuberculosis [6] the existence of recurrent abscess rebelling to antibiotics; the existence of fistulized axillary lymphadenopathy, mammary fistula with nipple discharge and the existence of a breast fistula with intermittent flow rhythmized by the menstrual cycle.
On the radiological level, there are no specific mammographic signs of mammary tuberculosis [11,12], mammography may show irregular heterogeneous opacities, poorly limited sometimes with calcifications rather orienting towards a malignant etiology. On ultrasound, mammary tuberculosis often appears as a hypoechoic, heterogeneous image well or poorly limited with minimal posterior reinforcement [12]. On MRI, the aspects are not specific because they are found in carcinomas and abscesses. However the MRI makes it possible to make the assessment of locoregional extension.
The intra dermal reaction to tuberculin is usually positive in the endemic area. This test is insensitive, and may give false negatives, not excluding the diagnosis of tuberculosis [13].
The diagnosis of certainty is histological examination [14] with the detection of epitheloid and giant cell granuloma with caseous necrosis.
The diagnosis of certainty can be as bacteriological and is based on the identification of Mycobacterium tuberculosis in the biopsy or in the secretions of breast fistula. However, the tubercle bacillus is found only in 25% of cases [15]; In addition, culture it takes four to six weeks.
The main differential diagnosis to be feared in breast tuberculosis is breast cancer, other pathologies are to be discussed, such as breast abscess, fibroadenoma, sarcoidosis and granulomatous mastitis.
In our observation, in front of an inflammatory breast in an elderly and menopausal woman, the first diagnosis to evoke is essentially breast cancer and only the histological examination which allowed to make the diagnosis of mammary tuberculosis.
Therapeutic management of breast tuberculosis is usually based on conventional quadruple therapy with isoniazid, rifampicin, ethambutol and pyrazinamide for two months, followed by isoniazid and rifampicin for a total duration of nine to twelve months.
The surgical act is primarily a means of diagnosis by performing biopsies, excisions or lumpectomies to obtain histological certainty [1,2,4]. In the case of resistance to treatment antituberculosis or locally advanced diseases, a mastectomy can be offered for therapeutic purposes [1,2,4]. Currently, some authors advocate percutaneous drainage of abscess under tomographic or ultrasound control.
Once the treatment is done, the prognosis is excellent, subject to appropriate care of others tuberculous localizations. However, rigorous monitoring of adherence to treatment is necessary to prevent recurrence and the development of resistance to anti-tuberclosis drugs. Finally, the risk of contamination of the breastfeeding child deserves special attention, and can be discussed weaning.
Conclusion
Breast tuberculosis is a very rare localization of the tuberculosis. In tuberculosis endemic countries, this diagnosis should not be ignored and should be mentioned in the light of certain clinical and radiological data.
Breast cancer remains the main differential diagnosis to be eliminated. The medical and surgical management allows a favorable evolution in the majority of the cases.
Acknowledgment
We thank the anatomopathology Department of Ibn El Jazzar Hospital, Kairouan.
References
- Ben Hassouna J, Gamoudi A, Bouzaiene H, Dhiab T, Khomsi F, et al. (2005) Mammary tuberculosis: A retrospective study of 65 cases. Gynecol Obstet Fertil 33: 870-876.
- Elmrabet F, Ferhati D, Amenssag L, Kharbach A, Chaoui A (2001) Breast tuberculosis. Med Trop (Mars) 62: 77-80.
- Fadaei-Araghi M, Geranpayeh L, Irani S, Matloob R, Kuraki S (2008) Breast tuberculosis: Report of eight cases. Arch Iran Med 11: 463-465.
- Luh SP, Hsu JD, Lai YS, Chen SW (2007) Primary tuberculous infection of breast: experiences of surgical resection for aged patients and review of literature. J Zhejiang Univ Sci B 8: 580-583.
- Agoda-Koussema LK, Djibril AM, Adjenou KV (2014) Tuberculose mammaire: à propos d'un cas (Breast tuberculosis: a case report). J Afr Imag Méd 6: 73-77.
- Khanna R, Prasanna GV, Gupta P, Kumar M, Khanna S, et al. (2002) Mammary tuberculosis: report on 52 cases. Postgrad Med J 78: 422-424.
- Spyridon M, Dionysia L, Thomas G, Dimitrakakis C, Papaspyrou I, et al. (2002) Breast tuberculosis: Diagnosis, management and treatment. Int J Surg Case Rep 3: 548-550.
- Nassim B, Hichem KC, Fatiha Y, Kheloufi F (2012) Tuberculous mastitis: a diagnosis not to be ignored. Imaging of the Woman 22: 221-223.
- Hawilo A, Abdelmalek R, Mebazaa A, Addouni O, Kanoun F, et al. (2012) Breast tuberculosis: a rare diagnosis, often unrecognized. Médecine et Santé Tropicales 22: 292-296.
- Kamil G, Erpulat OS, Suleyman O, Korkmaz A (2013) Primary breast tuberculosis: Report of a case. Surgical Science 4: 68-71.
- Morsad F, Ghazli M, Boumzgou K, Abbassi H, El Kerroumi M, et al. (2000) Breast tuberculosis. J Gynecol Obstet Biol Reprod 30: 331-33.
- Filippou DC, Rizos S, Nissiotis A (2003) Primary breast tuberculosis: A case report. Radiology and Oncology 37: 1-3.
- Daali M, Hssaida R, Hda A (2001) La tuberculose primitive du sein. Presse Med 30: 431-433.
- Mirsaeidi SM, Masjedi MR, Mansouri SD, Velayati AA (2007) Tuberculosis of the breast: Report of 4 clinical cases and literature review. Eas Mediter Health J 13: 670-676.
- Makanjuola D, Murshid K, Al Sulaimani S, Al Saleh M (1996) Mammographic features of breast tuberculosis: the skin bulge and sinus tract sign. Clin Radiol 51: 354-358.
Citation: Houssem R, Abir A, Abdrahmen D, Najeh B (2017) Breast Tuberculosis: A Diagnosis Often Unknown: A Case Report. J Tuberc Ther 2: 109.
Copyright: © 2017 Houssem R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 5495
- [From(publication date): 0-2017 - Apr 01, 2025]
- Breakdown by view type
- HTML page views: 4649
- PDF downloads: 846