Research Article Open Access
Breaking Bad News: Preferences of Cancer Patients in Saudi Arabia
Syed Mustafa Karim1*, Jamal M Zekri1,5, Sawsan Bassi2, Baker bin Sadiq2, Ehab M Abdelghany3, Hossam Abdelrahman1 and Elshami Elamin41Consultant Medical Oncologists King Faisal Specialist Hospital and Research Center, MBC J-64, PO Box 40047, Jeddah 21499, Saudi Arabia
2Research Center King Faisal Specialist Hospital and Research Center, MBC J-64, PO Box 40047, Jeddah 21499, Saudi Arabia
3National Cancer Institute, Cairo University, Egypt
4Central Care Cancer Center, 730 Medical Center, Dr. Newton, KS 67114, USA
5Faculty of Medicine, Al-Faisal University, Saudi Arabia
- *Corresponding Author:
- Syed Mustafa Karim
Consultant Medical Oncology
King Faisal Specialist Hospital and Research Center
MBC-J64, PO Box 40047, Jeddah 21499, Saudi Arabia
Tel: +966-2-6677777
Fax: 64030
E-mail: skarim@kfshrc.edu.sa
Received date: December 30, 2014; Accepted date: February 16, 2015; Published date: February 28, 2015
Citation: Karim SM, Zekri JM, Bassi S, Sadiq B, Abdelghany EM, et al. (2015) Breaking Bad News: Preferences of Cancer Patients in Saudi Arabia. J Palliat Care Med 5:207. doi: 10.4172/2165-7386.1000207
Copyright: © 2015 Karim SM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: It is believed in some Middle Eastern (ME) cultures that disclosure of bad news to cancer patients may cause loss of hope. This is often used to justify withholding such news. In this study, we examine cancer patients ‘preference regarding breaking bad news and disease information disclosure to them. Patients and Methods: Nine close ended questions addressing patient’s disclosure preference and one question addressing timing of disclosure to the family were designed in a questionnaire format and were answered by cancer patients in an outpatient setting. Affirmative “Yes” answer indicates preference to be informed of bad news. Results: One hundred patients were recruited and answered the questions. 87% of patients preferred to be informed of their cancer diagnosis. There was no statistically significant effect of age, gender, education level, professional status, diagnosis and stage of disease on this preference. 98% wanted to know of serious news about their health. 60% of patients answered “Yes” to 8 or 9 questions. Age ≥ 50 compared to <50 years was the only factor significantly associated with likelihood of affirmative response to 8 or 9 questions (Chi2 P=0.027). Conclusions: Our study indicates that most cancer patients in Saudi Arabia prefer to know the diagnosis of cancer and any related poor outcomes, and to be involved in decision making throughout the course of their illness. This is in congruence with results of other studies from other parts of the world. Given this accumulating body of evidence, healthcare provider should, whenever possible, keep the patients involved in the decision making process throughout the cancer journey.
Keywords
Cancer-related bad news; End-of-life care; Middle Eastern; Saudi Arabia
Introduction
In the past few decades traditional paternalistic models of patient care have given way to emphasis on patient autonomy and empowerment. As a result in most parts of the world, information about health and disease is disclosed to the individual patient first. In some cultures it is believed that disclosure of bad news to patients may adversely affect them and cause patients to lose hope. In most of these cases, family members will act as bearers to the bad news. There is uncertainty if and how the news is then communicated between the family members and the patient. Physicians in these cultures may be more likely to follow family wishes [1,2].
Majority of cancer patients’ relatives in societies with eastern culture (including the Middle East) prefer and demand, and in most times impose a “do not tell approach” [1]. Most physicians treating these cancer patients feel that patients have the right to know about their health and that this knowledge will help them sail through the different stages of cancer journey.
There is evidence that most patients want to know more about their health and diseases [3]. The relatives’ wish on one hand and patient/physician wish on the other hand are totally opposed. Getting the balance without compromise is challenging.
This study investigates Saudi Arabian cancer patients’ perspective on the issue of communicating cancer bad news and their preference of wanting to know cancer related information.
Patients and Methods
Ten closed ended questions were designed to test patients’ perspectives regarding disclosure of bad news. The questions were handed to patients to attending the out-patient oncology clinic at a single tertiary care hospital which receives referrals from all provinces of Saudi Arabia. The questions reflect possible bad news communication from diagnosis to end of life (Table 1). The questions are designed to address the individual patient asking for his/her personal preference or will. For example “Do you prefer to be informed of the diagnosis of cancer?”. Differences in responses between cohorts of patients were compared using Chi-square test. To quantify the extent of desired disclosure of bad news, we chose a cut off of affirmative response to ≥8 questions. This reflects preference to be informed majority (89%) of information.
| Question: Do you… | “Yes” |
|---|---|
| 1- Prefer to be informed of the diagnosis of cancer | 87% |
| 2- Prefer to know of any possible poor outcome | 90% |
| 3- Prefer to hear the term chemotherapy if it is part of treatment | 71% |
| 4- Prefer to know if treatment is not effective, | 85% |
| 5- Prefer to know every significant change about the condition and outcome | 92% |
| 6- Agree that doctor should not hold information of you at the request of family member | 80% |
| 7- Want to know serious news about health | 98% |
| 8- Prefer to be informed if there are no specific anti-cancer treatment options | 90% |
| 9- Prefer involving the patient in end of life discussion | 56% |
| 10- Bad news should be disclosed first to: | |
| The patient | 43% |
| A family member | 16% |
| Both at the same time | 40% |
Table 1: Questionnaire and frequency of affirmative response.
Adult patients attending the oncology out-patient clinic with cancer diagnosed at least 3 months prior to recruitment, aware of their diagnosis, and with ability to read and write or verbally communicate were included in the study.
The patients were approached by the investigator (treating oncologist or the research nurse) to provide verbal explanation about the study and obtain verbal and written consent of participation. The patients were then given the questionnaire in native language to self-complete within the clinic setting. For those patients unable to read, the investigator read the questionnaire and documented the patient’s exact response. The investigator was available during completion of the questionnaire to explain any ambiguity. The organization’s research institutional review board reviewed the study and granted approval. All patients were recruited within one month.
Results
One hundred and three patients were approached. One hundred patients agreed to participate and answered the questions. Median age was 48 (18-80), 72% were females and 28% were males. Patients’ characteristics are shown in Table 2.
| Total number: 100 | |
|---|---|
| Males | 28 |
| Females | 72 |
| Median age | 48 (18-80) years |
| Education level: | |
| Pre university | 52 |
| University and higher | 48 |
| Stage of cancer | |
| Metastatic | 30 |
| Non metastatic | 65 |
| Missing | 5 |
| Professional status | |
| Professionally active | 39 |
| Not working | 48 |
| Retired | 10 |
| Students | 3 |
| Cancer diagnosis: | |
| Breast cancer | 48 |
| Lymphomas | 17 |
| Gastrointestinal | 15 |
| Genito-urinary | 14 |
| Sarcomas | 3 |
| Melanoma | 1 |
| Parotid | 1 |
| Thyroid | 1 |
| Current management: | |
| Hormonal therapy | 25 |
| Chemotherapy | 24 |
| Other cancer therapies | 11 |
| No active therapy | 40 |
Table 2: Patient characteristics.
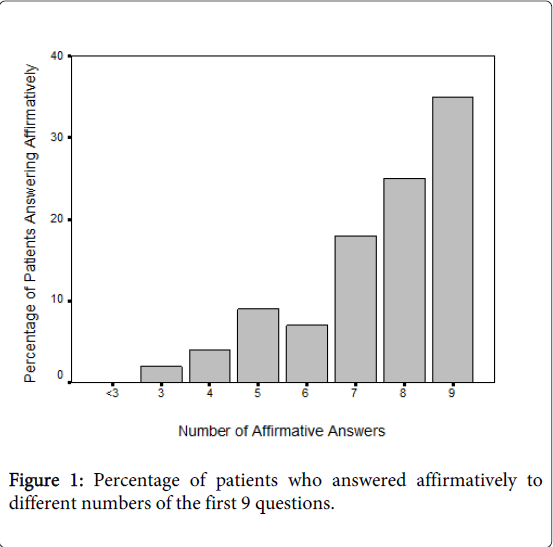
87% of patients preferred to be informed of their cancer diagnosis. 98% wanted to know of serious news about their health. Responses to other individual questions are also depicted in the Table 1 and they show that majority of patients preferred to be informed of other aspects of cancer treatment and possible unfavourable outcome. Relatively small majority (56%) preferred to be involved in end of life discussion. 83% of patients wanted to be the first to know of any bad news (either alone; 43% or with accompanied family member; 40%). 60% of patients answered “Yes” to 8 or 9 questions. No patients (0%) answered “Yes” to <3 questions (Figure 1).
Table 3 shows effects of patients’ and disease related factors on rate of affirmative answer to question 1. There was no statistically significant effect of age, gender, education level, professional status, diagnosis and stage of disease. Among these factors, older age (≥50 vs. <50 years) was the only factor significantly associated with likelihood of affirmative response to 8 or 9 questions (72% vs.50% respectively, Chi2 P=0.027).
| Affirmative Response to question 1 | Chi2 P value | Affirmative Response to >7 questions | Chi2 P value | |
|---|---|---|---|---|
| Gender | ||||
| Male | 24/28 (86%) | 0.812 | 16/28 (57%) | 0.716 |
| Female | 63/72 (88%) | 44/72 (61%) | ||
| Age | ||||
| <50 years | 45/54 (83%) | 0.237 | 27/54 (50%) | 0.027 |
| ≥50 years | 42/46 (91%) | 33/46 (72%) | ||
| Professiona | ||||
| Unemployed | 47/51 (92%) | 0.118 | 29/51 (57%) | 0.514 |
| Employed | 40/49 (82%) | 31/49 (63%) | ||
| Education | ||||
| Pre-university | 46/52 (89%) | 0.651 | 31/52 (60%) | 0.935 |
| University or higher | 41/48 (85%) | 29/48 (60%) | ||
| Diagnosis | ||||
| Breast cancer | 41/48 (85%) | 0.960 | 28/48 (53%) | 0.26 |
| Lymphoma | 15/17 (88%) | 11/17 (65%) | ||
| Gastrointestinal cancer | 13/15 (87%) | 8/15 (53%) | ||
| Genitourinary cancer | 13/14 (93%) | 10/14 (71%) | ||
| Othersb | 5/6 (83%) | 3/6 (50% | ||
| Stage of cancerc | ||||
| Metastatic (Stage IV) | 25/30 (83%) | 0.568 | 16/30 (53%) | 0.484 |
| Non-metastatic (Stage I-III) | 57/65 (87%) | 40/65 (62%) |
Table 3: Cross-tabulation between patients’ factors and affirmative answer to question 1 and to ≥7 questions; a‘Unemployed’ includes not working and students; ‘Employed’ includes professionally active and retired; bIncluding sarcoma, melanoma, parotid and thyroid cancers; cData on stage of cancer missing on 5 patients.
Discussion
Personal observations and research evidence show that health related information and in particular cancer related bad news are not shared with significant proportion of patients [2]. This is more prevalent in non-Western countries [2]. For many decades, evidence also showed that majority of cancer patients in western societies need to know the nature of diagnosis and they want as much information as possible about their condition [3-6].
It is clear from available evidence that in the ME, serious health related information (including cancer bad news) is not disclosed to most patients. Experts from this region have documented their experience and views about this issue. In his review, Bou Khalil [7] reports that in the Greater ME region, a diagnosis of cancer is still mixed with social stigma and misperceptions. Family members and caregivers' attitudes, perceptions and beliefs about telling the truth to the patient seem to be in favour of concealment. Aljubran described the position in Saudi Arabia that family members find themselves forced by their genuine cultural and mainly religious values to extend their help and support to the patient. They find themselves obliged, and frequently, allowed by the patient to do so by stepping forward and taking over some or all of the patient's responsibilities. This supportive attitude, unfortunately, at the end may evolve into a dominating attitude that hijacks the patient's basic right of knowledge and decision-making [8]. In a survey of 249 physicians from Saudi Arabia, only 47% of physicians indicated they provided information on diagnosis and prognosis of serious illnesses to patients [9]. As discussed above, most of the available literature have either documented personal experience and views or approached physicians and asked for their practice and attitude. We identified only 2 published reports in the ME region describing patients’ perspective to cancer bad news [10,11]. Both studies had some differences compared to our study.
Encouraged by the above and by personal experience, we conducted this study to shed light on the perspective of cancer patients in Saudi Arabia on breaking cancer bad news. Our results confirm that majority of cancer patients from this region (71-98%) prefer to know most of the information about their condition’s diagnosis, outcome, treatment, results of treatment and progress (Table 2). In addition, 90% prefer to be informed of the more serious information if there are no specific anti-cancer treatment options available for their condition. Al-Ahwal [10] recruited 136 individuals (33 cancer patients, 63 doctors, and 40 public) to a questionnaire based survey in Saudi Arabia. In the cancer patients’ group, 27/33 (81.7%) wanted to be informed of the diagnosis of cancer. 20 out of 33 (60.6%) wanted to be informed of the prognosis. This work is probably the first of its kind to investigate cancer patients’ perspective in this geographic region but the interpretation of its results may be limited by the small sample size (n=33) and it may not represent current views as it was conducted more than 15 years ago. Nevertheless, it showed that significant majority of cancer patients wished to be informed. Our results show that 87% prefer to be informed of the diagnosis of cancer. This is slightly higher than 81.7% reported by Al-Ahwal [10]. In addition, our results show that 90% of patients prefer to know of any possible poor outcome. This is higher than 60.6% reported as wanting to be informed of the prognosis in Al-Ahwal’s study. This difference may represent a shift of patients’ attitude over 15 years or may simply represent expected cross-study differences.
Also in Saudi Arabia, Al-Amri recruited 114 cancer patients between 2002 and 2005 to a questionnaire based study before they knew their diagnosis [11]. All patients except 1 (99%) wished to know all the information about their disease and 100% rejected withholding information. In our study population, all patients were already aware of their cancer diagnosis. To avoid selection bias, we approached all eligible patients attending the oncology out-patient setting and recruited patients within one month. Nevertheless, findings in all these studies indicate that majority of patients wish to be kept informed.
It is believed that older patients may less likely wish to know a lot of details about their medical condition. In UK based study involving 2331 patients [6], only 13.2% patients stated that in general they preferred to leave disclosure of details up to the doctor. These patients tended to be older patients more than 70 years of age (P<0.0001), although paradoxically they still wanted to know certain specific details. Looking at one specific question: “Want to know if the condition is cancer or not?” 98.4% and 96.9% of patients <70 and >70 years answered “Yes”. The median age of patients in our study is 48 years and accordingly 50 years was taken as cut off to study association between age and outcome. Only 10% of our study patients were ≥70 years of age and this is representative of cancer patients’ age distribution in Saudi Arabia. The cancer incidence report of Saudi Arabia (2009) showed that only 8.8% and 5.3% of all male and female cancer patients were over 74 years of age respectively [12].
We found that 91% of older patients compared to 83% of younger patients preferred to know the diagnosis if it is cancer (P=0.237). This means that older patients want to know the cancer diagnosis as much as younger patients. A study of 250 cancer patients in Scotland also showed that 96% patients wanted to know if the diagnosis was cancer, and similar to our findings there was no difference between patients’ responses and age [3].
We also attempted to investigate the amount of bad news patients want to know. We performed this by calculating the percentage of patients who answered “Yes” to different proportions of the first 9 questions. This is shown in detail in Figure 1. To differentiate between preferences to know more or less, it is ideal to select a cut off of about 50%. This can be achieved by selecting a cut off of answering “Yes” to ≤5 questions indicating preference to want to know ≤56% of the bad news. However, only 9% of patients fell in this category rendering such analysis impractical. Answering “Yes” to 8 or more questions indicate preference to want to know ≥89% of the bad news. Even with this high cut off, we found that 60% of patients prefer to know ≥89% of possible bad news. To our knowledge, this is the only published report that addresses the amount of possible bad news cancer patients want to know.
Our results show that cancer patients prefer to be informed of the diagnosis regardless of demographics and disease characteristics. Gender, professional status, diagnosis and stage of disease were not associated with preference to know majority of cancer related bad news. These results are similar to the findings in the UK study mentioned above, where majority of patients of both gender and different stage of disease wanted similar details of information [6]. In our study, education level did not influence the willingness to obtain cancer information. We are not aware of any studies investigating this relation. However, the study from Scotland of 250 cancer patients reported patients from more affluent areas to want more information and those from deprived areas to want less [3].
In a culture where there is pressure from family members to disclose information to them and not to patients, we felt that it is vital to take the opinion of patients [7,8]. Question 10 was designed differently from other questions to address this matter (Table 1). It gave the patient 3 options. Majority of patients (83%) wanted to be the first to know about any bad news disclosed (either alone; 43% or with accompanied family member; 40%). This indicates that patients consider these specifics as their own and that they have the right (and want) to have first ownership of information about their health. It also indicates that 40% of patients see the role of family as supportive rather than dominating. This first ownership right has to be respected by treating physicians and patient’s consent should be sought prior to disclosure of information to others.
It seems that majority of patients with diagnosis of cancer irrespective of geographic origin prefer to be informed of serious health related news. This is well established in western countries. Similar attitude is confirmed in the Far East, for example in Japan where in a study more than 90% of cancer patients strongly preferred to discuss their current medical condition and treatment options with their physician [13].
For practical reasons, we recruited patients from one hospital. This may be considered as a limitation. However, our hospital is a tertiary referral centre serving all provinces of the country. Therefore, we believe our results can be generalized to the whole Saudi population who share common cultural and traditional values with the rest of the ME.
It seems obvious that majority of patients desire disclosure of cancer related news. At the same time, this report shows that small proportion of cancer patients want to know less information than others (Figure 1 and Table 1). Here empathic and careful communication is the key. Baile et al. [14] organised recommendations into the mnemonic SPIKES (Setting up, Perception, Invitation, Knowledge, Emotions, Strategy and Summary) which is a rather simple and useful approach. The “invitation” step in SPIKES can identify patients who want less information. In a previous review, we addressed the general aspects of breaking bad news to patients detailing the SPIKE approach including the need to get the patient's permission to share bad news quoting “Getting permission may be especially important for patients from non-Western cultures in which autonomy of the individual may not be paramount and healthcare decision-making is shared with others”. For example, the physician may say, “I'd like to share with you the results of your tests. Is that okay?” [15].
Before ordering tests or procedures, physicians need to inform patients about possible results, which prepare patients for potential bad news. Physicians also should ask patients if they want only basic information or a detailed disclosure” [15].
Governing bodies and specialist medical guidelines highly recommend respecting patients’ right of information about their medical condition. The good medical practice guidance of the UK General Medical Council (GMC) recommends responding to patients’ concerns and preferences. It also recommends sharing with patients the information they want or need to know about their condition, it’s likely progression, and the treatment options available to them, including associated risks and uncertainties [16]. In Japan, similarly guidelines clearly state that diagnosis must be first discussed with cancer patients themselves whenever possible and from the initial interview, physicians should try to tell the truth consistently [17,18].
Clinical Implication
Cancer is a relatively common disease and most physicians will be faced with the task of breaking bad news to cancer patients. Unfortunately, most medical school do not include structured education and training in communication skills in their curriculum. For this reason physicians develop their own approach which may not cater to the needs of patients receiving serious health related news. In some cultures, the issue is compounded by possible misperception that patients may not want to receive worrisome health information. Our findings indicate that in our region, the vast majority of cancer patients prefer to be informed of cancer related bad information. Furthermore, more than half of patients want to be involved even in end of life discussion. A change of approach in the clinic towards asking each individual patient how much information he/she wants to be informed will guarantee the delivery of the right amount of information to the right patient.
Conclusion
Our data confirm that cancer patients in Saudi Arabia have strong preference to be informed of cancer related bad news. Physicians should not surrender to relatives’ demands to conceal information from patients. Practical steps and institutional and national guidelines should support this notion.
References
- Ozdogan M, Samur M, Artac M, Yildiz M, Savas B, et al. (2006) Factors related to truth-telling practice of physicians treating patients with cancer in Turkey.J Palliat Med 9: 1114-1119.
- Baile WF, Lenzi R, Parker PA, Buckman R, Cohen L (2002) Oncologists' attitudes toward and practices in giving bad news: an exploratory study.J ClinOncol 20: 2189-2196.
- Meredith C, Symonds P, Webster L, Lamont D, Pyper E, et al. (1996) Information needs of cancer patients in west Scotland: cross sectional survey of patients' views.BMJ 313: 724-726.
- Cassileth BR, Zupkis RV, Sutton-Smith K, March V (1980) Information and participation preferences among cancer patients.Ann Intern Med 92: 832-836.
- Sutherland HJ, Llewellyn-Thomas HA, Lockwood GA, Tritchler DL, Till JE (1989) Cancer patients: their desire for information and participation in treatment decisions.J R Soc Med 82: 260-263.
- Jenkins V, Fallowfield L, Saul J (2001) Information needs of patients with cancer: results from a large study in UK cancer centres.Br J Cancer 84: 48-51.
- Bou Khalil R (2013) Attitudes, beliefs and perceptions regarding truth disclosure of cancer-related information in the Middle East: a review.Palliat Support Care 11: 69-78.
- Aljubran AH (2010) The attitude towards disclosure of bad news to cancer patients in Saudi Arabia.Ann Saudi Med 30: 141-144.
- Mobeireek AF, al-Kassimi FA, al-Majid SA, al-Shimemry A (1996) Communication with the seriously ill: physicians' attitudes in Saudi Arabia.J Med Ethics 22: 282-285.
- Al-Ahwal M (1998) Cancer patients' awareness of their disease and prognosis.Ann Saudi Med 18: 187-189.
- Al-Amri AM (2009) Cancer patients' desire for information: a study in a teaching hospital in Saudi Arabia.East Mediterr Health J 15: 19-24.
- Saudi Cancer Registry (2009). Ministry of Health. Kingdom of Saudi Arabia.
- Fujimori M, Akechi T, Morita T, Inagaki M, Akizuki N, et al. (2007) Preferences of cancer patients regarding the disclosure of bad news.Psychooncology 16: 573-581.
- Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, et al. (2000) SPIKES-A six-step protocol for delivering bad news: application to the patient with cancer.Oncologist 5: 302-311.
- Kurer MA, Zekri JM (2008) Breaking bad news: can we get it right?Libyan J Med 3: 200-203.
- General Medical Council (2010) Treatment and care towards the end of life: good practice in decision making.
- http://www.gmc-uk.org/static/documents/content/End_of_life_9_May_2013.pdf
- Okamura H, Uchitomi Y, Sasako M, Eguchi K, Kakizoe T (1998) Guidelines for telling the truth to cancer patients. Japanese National Cancer Center.Jpn J ClinOncol 28: 1-4.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 15258
- [From(publication date):
March-2015 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10598
- PDF downloads : 4660