Short Communication Open Access
Blood Derived Induced Pluripotent Stem Cells (iPSCs): Benefits, Challenges and the Road Ahead
Jimmy El Hokayem1, Holly N Cukier1,2# and Derek M Dykxhoorn1,3*1John P. Hussman Institute for Human Genomics, University of Miami Miller School of Medicine, Miami, USA
2Department of Neurology, University of Miami Miller School of Medicine, Miami, USA
3John T. Macdonald Foundation Department of Human Genetics, University of Miami Miller School of Medicine, Miami, USA
- *Corresponding Author:
- Derek M. Dykxhoorn
John P. Hussman Institute for Human Genomics
University of Miami Miller School of Medicine
1501 NW 10th Ave, Biomedical Research Building
Room 509, Miami, USA
Tel: (305) 243-7596
E-mail: DDykxhoorn@med.miami.edu
Received date October 13, 2016; Accepted date October 18, 2016; Published date October 25, 2016
Citation: Hokayem JEl, Cukier HN, Dykxhoorn DM (2016) Blood Derived Induced Pluripotent Stem Cells (iPSCs): Benefits, Challenges and the Road Ahead. J Alzheimers Dis Parkinsonism 6:275. doi: 10.4172/2161-0460.1000275
Copyright: © 2016 Hokayem JEl, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Alzheimers Disease & Parkinsonism
Abstract
Since the creation of induced Pluripotent Stem Cells (iPSCs) ten years ago, hundreds of publications have demonstrated their considerable impact on disease modeling and therapy. In this commentary, we will summarize key milestones, benefits and challenges in the iPSC field. Furthermore, we will highlight blood as an effective and easily accessible source for patient-specific iPSCs derivation in the context of work done in our laboratory and others.
Abstract
Since the creation of induced Pluripotent Stem Cells (iPSCs) ten years ago, hundreds of publications have demonstrated their considerable impact on disease modeling and therapy. In this commentary, we will summarize key milestones, benefits and challenges in the iPSC field. Furthermore, we will highlight blood as an effective and easily accessible source for patient-specific iPSCs derivation in the context of work done in our laboratory and others.
Introduction
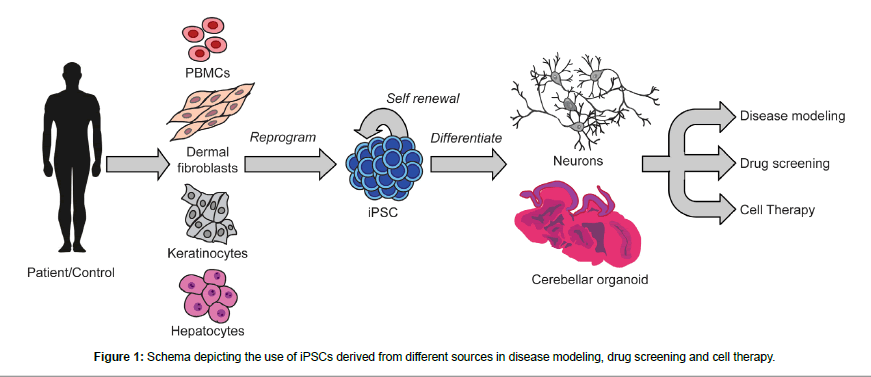
In 2006, Takahashi and Yamanaka were the first to reprogram adult cells into embryonic-like pluripotent stem cells, or induced Pluripotent Stem Cells (iPSCs), in mice [1]. One year later, the same laboratory, as well as an independent research team, both reported successfully reprogramming human adult cells into iPSCs [2,3]. This magnum opus stirred a whirlwind of scientific research activity in the stem cell field over the past 10 years, yielding vast advances in basic research and disease modelling and hinting at potential applications in the clinical and therapeutic arenas (Figure 1) [4].
iPSC reprogramming is typically initiated in somatic cells via the overexpression of four key genes (Oct3/4, Klf4, c-myc and Sox2), termed the “Yamanaka factors” [1-3]. Once generated, iPSCs have the same properties as embryonic stem cells (ESCs) in that they can indefinitely self-renew and can differentiate into all body cell types, with the possible exception of extra-embryonic tissue cells like placental cells. Although iPSC has shown morphological, karyotype and gene expression characterization, that mimic ESCs, there appears to be differences in epigenetic marks (e.g. DNA methylation) [3,5]. That is, the process of reprogramming appears to rejuvenate the somatic cells so that they adopt a stem cell-like state [6-8]. However, the process of resetting the epigenetic marks takes longer than the time required of establishing pluripotency [9]. However, as the iPSC are passaged for longer periods of time, these epigenetic marks are lost and the iPSC will more and more resemble ESCs [10].
iPSCs have had a substantial impact on both the basic and clinical levels of biomedical research. To start, iPSCs offered a convenient alternative to ESCs which are ethically controversial due to the necessity of their creation from human embryos [11]. As such, it is impossible to know what medical ailments may occur over a lifetime if the embryo had developed into a person. In addition, there is so little source material when ESCs are collected that the genetic background cannot be determined prior to reprogramming. In contrast, iPSCs allow patient-specific lines to be generated for which a full clinical and genetic assessment can be made in advance of reprogramming. This allows research efforts to be focused on creating the most relevant models for studying disease. There is even the potential for patientspecific iPSCs, tissues and organs to be therapeutically used, free from the possibility of rejection by the host’s body [12]. Interestingly, studies have shown that patient-specific iPSC lines represent a plentiful and critical resource for drug screening and could aid in the discovery of new disease treatments and therapies [13].
Nonetheless, the success of these recent scientific endeavors vastly relies on the capability of iPSCs to model human diseases. Indeed, iPSCs have proven to be critical in supplying patient-specific cell types and organoids that were otherwise inaccessible for studying normal human developmental processes, as well as, detecting and deciphering aberrant processes as a result of disease [11,13-15]. Hence, iPSCs present a prime source for research of the mechanistic pathobiology behind many pressing diseases affecting the human population like autism spectrum disorders, Alzheimer disease, Huntington disease, Parkinson disease, glaucoma, and gut and liver diseases, among others [13-18].
Peripheral Blood Mononuclear Cells (PBMCs) as Source for iPSCs Derivation
Since the first iPSCs were generated from skin fibroblasts, many other sources of adult somatic cells have been probed for their suitability for iPSC reprogramming [2,3].These cell types include peripheral blood mononuclear cells (PBMCs), neuronal progenitor cells, keratinocytes, hepatocytes, kidneys, muscles, adrenal glands, and fibroblasts of mouse tail tips [13,19]. Indeed, these sources exhibit various levels of ease, efficacy, and cost in iPSC production. Differences in efficiency of iPSC derivation from distinct sources have been attributed to the original epigenetic state of the adult somatic cell type and its requirement to go through multiple steps of de-differentiation (e.g. mesenchymal to epithelial transition) to reach a pluripotent state [19]. Our laboratory was the first to use PBMCs to generate patient-specific iPSCs from individuals with autism spectrum disorder (ASD) and has extensively studied the adequacy of this iPSC source and reprogramming methods for the purpose of modeling ASD [18]. Indeed, we have been able to efficaciously generate iPSCs from patient-specific PBMCs. These iPSCs were, in turn, successfully differentiated to GABAergic neurons [18]. Moreover, recent studies demonstrate the successful derivation of iPSCs from PBMCs collected from Alzheimer disease (AD) and Parkinson disease (PD) patients [20-25]. Undeniably, blood is becoming a routinely used source for iPSC generation.
Benefits of PBMCs as a Source for iPSC Derivation
PBMCs isolated from whole blood present many benefits for the derivation of iPSCs. First of all, blood can be collected relatively easily from patients as compared to collecting dermal fibroblasts through a whole skin biopsy procedure. Moreover, drawing blood is routinely performed in clinical settings or even out in the field; all that is required is a trained phlebotomist without the need of either highly specialized staff or the use of expensive anesthetics and surgical tools. Therefore, acquiring blood samples from patients is a routine, relatively cheap, and much less intrusive procedure as compared to skin biopsies, which can help patients overcome the psychological barrier of participating in research and clinical trials. In our experience, this latter point is crucial for successful ascertainment of patients because it allows access to a larger number of willing participants. Moreover, time is needed for the expansion of dermal fibroblasts in vitro before reaching adequate numbers needed for reprogramming while PBMCs collected from blood can be reprogrammed immediately after extraction [1,2,18]. Furthermore, in our experience, reprogramming success is not adversely affected when performed on PBMCs extracted from aged patients, in clear contrast with dermal fibroblasts extracted from elderly patients. In support of this convenient source of iPSCs we, as well as other laboratories, have successfully demonstrated the feasibility of using this accessible resource for cell reprogramming and modeling diseases like ASD, AD and PD [3,20-25].
Challenges of PBMCs as a Source for iPSC Derivation
Despite the benefits that PBMCs provide, they still pose a few challenges for iPSC derivation. Indeed, once blood is collected, temperature fluctuations and an extended timeframe to the isolation of the PBMCs can adversely affect the quality of the sample. Another challenge to using blood as a source material is that it can be difficult to study patients who have clotting disorders [26,27]. These later disorders could hinder successful extraction of needed PBMC numbers from blood, and subsequently negatively affects reprogramming success and iPSC derivation.
Another challenge is the carryover of epigenetic marks from PBMCs to the reprogrammed iPSCs. This could affect the pluripotency potential of the derived iPSCs because of “epigenetic memory”, making it difficult to differentiate to certain types of cells. Evidence in the literature has shown that this issue can be circumvented by extending the number of passages the iPSC undergo to reach a basal state of epigenetic marks needed for full differentiation potential [9].
Finally, iPSCs derived from all sources pose a critical challenge regarding quality control. Since the different derived lines may have a varied differentiation potential, they must indeed be fully tested as such for quality control. In line with this train of thought, a battery of tests have been recently proposed to ensure cell line identity, genomic stability, pluripotency potential and check for residual reprogramming factors [28].
The Future of PBMC Derived iPSCs
Despite the challenges described above, PBMC-derived iPSC lines are a valuable resource for the advancement of research and therapies for many critical diseases. Indeed, the scientific community has rightfully invested huge resources to successfully tackle these challenges. Remaining to see is how government agencies are going to streamline funding and law-making in order to cope with fast approaching clinical applications of PBMC-derived iPSCs. To date, only one human trial using iPSCs has been reported; this key study used the cells to treat macular degeneration. This same trial has was halted because of the presence of two non-tumorigenic genetic changes found in the patient specific iPSCs and the differentiated Retinal Pigment Epithelium sheets generated [4]. Nonetheless, one can imagine the plethora of clinical trials that will emerge in the near future and their vast potential to impact how we ameliorate human disease.
Acknowledgement
This work was supported by the NIH grant 5P50NS071674 (DMD).
References
- Takahashi K, Yamanaka S (2006) Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126: 663-676.
- Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, et al. (2007) Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131: 861-872.
- Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, et al. (2007) Induced pluripotent stem cell lines derived from human somatic cells. Science 318:1917-1920.
- Scudellari M (2016) How iPS cells changed the world. Nature 534: 310-312.
- Wernig M, Meissner A, Foreman R, Brambrink T, Ku M, et al. (2007) In vitro reprogramming of fibroblasts into a pluripotent ES-cell-like state. Nature 448: 318-324.
- Vera E, Studer L (2015) When rejuvenation is a problem: challenges of modeling late-onset neurodegenerative disease. Development 142: 3085-3099.
- Miller JD, Ganat YM, Kishinevsky S, Bowman RL, Liu B, et al. (2013) Human iPSC-based modeling of late-onset disease via progerin-induced aging. Cell Stem Cell 13: 691-705.
- Soria-Valles C, Lopez-Otin C (2016) iPSCs: On the Road to Reprogramming Aging. Trends Mol Med 22: 713-724.
- Polo JM, Liu S, Figueroa ME, Kulalert W, Eminli S, et al. (2010) Cell type of origin influences the molecular and functional properties of mouse induced pluripotent stem cells. Nat Biotechnol 28: 848-855.
- Kim K, Doi A, Wen B, Ng K, Zhao R, et al. (2010) Epigenetic memory in induced pluripotent stem cells. Nature 467: 285-290.
- Yamanaka S (2010) Patient-specific pluripotent stem cells become even more accessible. Cell Stem Cell 7: 1-2.
- Kaneko S, Yamanaka S (2013)To be immunogenic, or not to be: that's the iPSCquestion. Cell Stem Cell 12: 385-386.
- Colman A, Dreesen O (2009) Pluripotent stem cells and disease modeling. Cell Stem Cell 5: 244-247.
- Hohwieler M, Illing A, Hermann PC, Mayer T, Stockmann M, et al. (2016) Human pluripotent stem cell-derived acinar/ductal organoids generate human pancreas upon orthotopic transplantation and allow disease modelling. Gut 2016-312423.
- Takebe T, Zhang RR, Koike H, Kimura M, Yoshizawa E, et al. (2014) Generation of a vascularized and functional human liver from an iPSC-derived organ bud transplant. Nat Protoc 9: 396-409.
- Consortium HD IPSC (2012) Induced pluripotent stem cells from patients with Huntington's disease show CAG-repeat-expansion-associated phenotypes. Cell Stem Cell 11: 264-278.
- Tucker BA, Solivan-Timpe F, Roos BR, Anfinson KR, Robin AL, et al. (2014) Duplication of TBK1 Stimulates Autophagy in iPSC-derived Retinal Cells from a Patient with Normal Tension Glaucoma. J Stem Cell Res Ther 3: 161.
- 18. DeRosa BA, Van Baaren JM, Dubey GK, Lee JM, Cuccaro ML, et al. (2012) Derivation of autism spectrum disorder-specific induced pluripotent stem cells from peripheral blood mononuclear cells. NeurosciLett 516: 9-14.
- . DeRosa BA, Van Baaren JM, Dubey GK, Lee JM, Cuccaro ML, et al. (2012) Derivation of autism spectrum disorder-specific induced pluripotent stem cells from peripheral blood mononuclear cells. NeurosciLett 516: 9-14.
- Raab S, Klingenstein M, Liebau S, Linta LA (2014) Comparative View on Human Somatic Cell Sources for iPSC Generation. Stem Cells Int 2014: 768391.
- Táncos Z, Varga E, Kovács E, Dinnyés A, Kobolák J (2016) Establishment of induced pluripotent stem cell (iPSC) line from a 75-year old patient with late onset Alzheimer's disease (LOAD). Stem Cell Res 17: 81-83.
- Chandrasekaran A, Varga E, Nemes C, Táncos Z, Kobolák J, et al. (2016) Establishment of induced pluripotent stem cell (iPSC) line from a 63-year old patient with late onset Alzheimer's disease (LOAD). Stem Cell Res 17: 78-80.
- Táncos Z, Varga E, Kovács E, Dinnyés A, Kobolák J (2016) Establishment of induced pluripotent stem cell (iPSC) line from an 84-year old patient with late onset Alzheimer's disease (LOAD). Stem Cell Res 17: 75-77.
- Ochalek A, Nemes C, Varga E, Táncos Z, Kobolák J, et al. (2016) Establishment of induced pluripotent stem cell (iPSC) line from a 57-year old patient with sporadic Alzheimer's disease. Stem Cell Res 17: 72-74.
- Nemes C, Varga E, Táncos Z, Bock I, Francz B, et al. (2016) Establishment of PSEN1 mutant induced pluripotent stem cell (iPSC) line from an Alzheimer's disease (AD) female patient. Stem Cell Res 17: 69-71.
- Zhou H, Martinez H, Sun B, Li A, Zimmer M, et al. (2015) Rapid and Efficient Generation of Transgene-Free iPSC from a Small Volume of Cryopreserved Blood. Stem Cell Rev 11: 652-665.
- Kitchens CS, Erkan D, Brandão LR, Hahn S, James AH, et al. (2011) Thrombotic storm revisited: preliminary diagnostic criteria suggested by the thrombotic storm study group. AmJ Med 124: 290-296.
- Ortel TL, Kitchens CS, Erkan D, Brandão LR, Hahn S, et al. (2016) Clinical causes and treatment of the thrombotic storm. Expert Rev Hematol 5: 653-659.
Relevant Topics
- Advanced Parkinson Treatment
- Advances in Alzheimers Therapy
- Alzheimers Medicine
- Alzheimers Products & Market Analysis
- Alzheimers Symptoms
- Degenerative Disorders
- Diagnostic Alzheimer
- Parkinson
- Parkinsonism Diagnosis
- Parkinsonism Gene Therapy
- Parkinsonism Stages and Treatment
- Stem cell Treatment Parkinson
Recommended Journals
Article Tools
Article Usage
- Total views: 29880
- [From(publication date):
October-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 28800
- PDF downloads : 1080