Case Report Open Access
Bladder Cancer
Babiano FMA1* and Rodriguez FA2
1Specialist in Family and Community Medicine, EAP Almaden, Guadalmez 's office , Ciudad Real, Spain
2Specialist in Family and Community Medicine, EAP Argamasilla de Calatrava, Ciudad Real, Spain
- *Corresponding Author:
- Miguel Angel Babiano Fernandez
Specialist in Family and Community Medicine, EAP Almaden
Guadalmez 's office , Ciudad Real, Spain
Tel: 673 073 651
E-mail: mababiano@sescam.jccm.es
Received date: June 29, 2016; Accepted date: July 26, 2016; Published date: July 29, 2016
Citation: Babiano FMA, Rodriguez FA (2016) Bladder Cancer. J Community Med Health Educ 6:456. doi:10.4172/2161-0711.1000456
Copyright: © 2016 Babiano FMA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Case Report
A 76 year old patient with a history of hypertension and osteoporosis treated currently with diuretics, calcium and ibandronic acid, no smoking and no other toxic habits, consulting for some months has intermittent episodes of painless hematuria without other associated symptoms. Physical examination revealed no relevant data. It is performed urine strip at that moment that reveals frank hematuria. It is including systematic analytical and urine culture and renal ultrasound is requested and interconsultation with Urologia.
The analytical data provides no relevance with blood count and normal biochemistry, including kidney function, urine confirmation of the presence of red blood cells and negative urine culture.
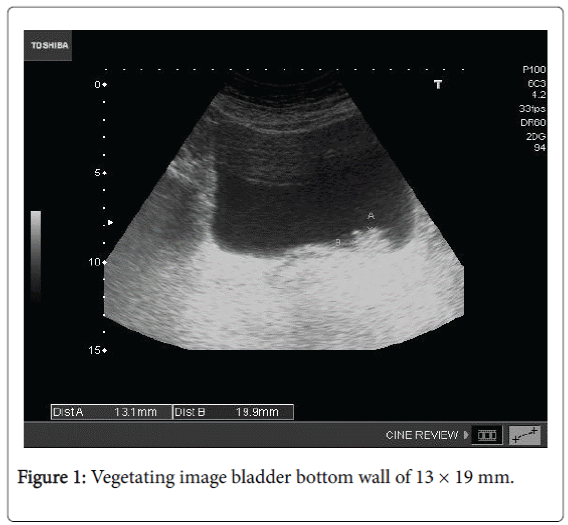
Given the delay in the query you performed abdominal ultrasound in the Health Center and found the following findings: liver echostructure homogeneous without visible LOES. Vesicle thin walls acalculous. pancreatic area without pathological findings. Kidneys of normal size with good cortico medullary differentiation, left kidney anechoic images with posterior reinforcement compatible with small sinus cyst. normal spleen. Vegetating image bladder bottom wall of 13 × 19 mm. Figures 1 and 2.
With the findings derived urgently to the urologist, who performed urography ureteropelvic confirming a normal morphology and cystogram with filling defect in the left bladder wall. At 2 weeks the patient was operated under spinal anesthesia and through RTU (TUR) 2 cm bladder tumors of the optic nerve at the level of left urethral orifice is removed. The histopathology of the lesion confirms the diagnosis of bladder papillary neoplasm of low malignant potential intraepithelial.
Comments
The prevalence of hematuria is between 0.18 and 16% of the general population, even in adults can reach 33%. Detection should lead to rule out the existence of a renal disease process or urinary tract.
The importance of hematuria does not depend on its intensity, but the cause that motiva [1,2] except hemodinánicos disorders that may endanger the patient's life. Hematuria may be associated with other disorders such as proteinuria, sometimes it appears as an isolated hematuria without the presence of other symptoms of urinary disturbance[3].
The macrohematuria sign has a positive predictive value (PPV) for malignancy of 22% in men over 60 years (in women of the same age is 8 %). For the population between 40 and 59 years, the VPP for cancer is 4% in men and 6% women [4].
Bladder cancer occurs mainly in the elderly. Around nine out of 10 people with this cancer are over 55 years old. Age average at the time of diagnosis is 73 years.
Is second in order of frequency and cause of death in urological tumors [5]. It ischaracterized usually (in 75% of cases) diagnosed in incipient stages, which would explain its good prognosis and therefore, its high survival.
Men are about three to four times more likely to develop cancer bladder during life than women. In general, the probability that men suffering from this cancer during their lifetime is about 1 in 26 and in the case of women, the odds are about 1 in 90.
Rates of new cancer cases and deaths from the disease have been fairly stable in men and have been declining slightly in women during the last years.
In the European Union more than 75,000 new cases are diagnosed each year, representing a crude incidence of 31 cases per 100,000 men and 9 cases per 100,000 women. In Spain we have more than 10,000 new diagnoses a year, with 47 cases per 100,000 men and almost 8 cases per 100,000 women.
To understand how cancer grows bladder is essential to know the anatomy of the bladder. The bladder wall is made up of four main layers. The inner line is composed of cells called transition or urothelial, and therefore this layer is called urothelium or transitional epithelium. Beneath the urothelium, there is a thin layer of connective tissue, blood vessels and nerves called lamina propria. The next layer is thick and muscle called the muscularis propria. Outside this muscle, a layer of connective tissue separate bladder fatty of other adjacent organs.
About half of all cases, patients initially diagnosed are bladder cancer while it is confined in the innermost layer of the bladder (or non-invasive cancer in situ). About 35% of patients have bladder that has invaded deeper layers cancer, but the cancer is still confined to the bladder. In most of the remaining cases, the cancer has spread to nearby tissues outside the bladder. In a few cases (about 4% of cases), spread to distant areas. As for histologic types of tumors of the bladder [6], are divided into 3 depending cells that comprise: urothelial transitional cell by (90-95%), Squamous (8%) and adenocarcinoma (2%). At diagnosis, 75-85% is superficial, 20% invades the muscle layer of the wall and 5% begins with metastasis. They are multifocal (anytime, anywhere) and 5-10% is located in the upper urinary tract or prostatic urethra.
Transitional cell carcinoma (urothelial). This type of cancer is by far the most common bladder cancer. Cells of transitional cell carcinomas (TCCs) resemble urothelial cells lining the inside of the bladder. Urothelial cells also cover other parts of the urinary tract, such as renal pelvis, ureter and urethra. Therefore, the transitional cell carcinomas may also occur in these places. In fact, patients with bladder cancer sometimes have other tumors in the kidneys, ureters or urethra. If someone has a cancer in a part of the urinary system, you need to examine the entire urinary tract for determine if tumors.
Often bladder cancers are described based on how far they have invaded bladder wall: Cancers noninvasive bladder remain in the inner layer of cells (Transitional epithelium), and they have not grown into deeper layers.Invasive cancers grow into the lamina propria or even deeper into the muscle layer. Invasive cancers are more likely to spread and they are more difficult to treat.
Bladder cancer can also be described as superficial or invasive than not compromises the muscle layer. These terms include noninvasive tumors and any invasive tumor has not grown into the main muscle layer of the bladder.The transitional cell carcinomas are also divided into two subtypes, papillary and plane, based on how they grow.
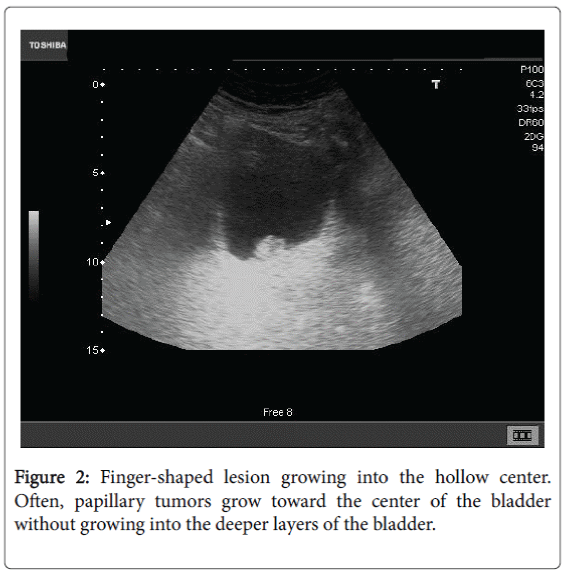
Papillary carcinomas, as the patient of our case, are thin projections of the inner surface of the bladder by way of fingers grow into the hollow center. Often, papillary tumors grow toward the center of the bladder without growing into the deeper layers of the bladder.
These tumors are called non-invasive papillary cancers. Sometimes the non-invasive papillary cancer of low grade is called papillary neoplasm of low malignant potential. This cancer usually has a very favorable prognosis [7].
Carcinomas planes never grow into the hollow part of the bladder. If a flat tumor is found only in the inner layer of cells of the bladder, it known as non-invasive carcinoma plane or a flat carcinoma in-situ.
If a papillary or flat tumor grows into the deeper layers of the bladder, it is called invasive carcinoma cell transition (or urothelial).
Squamous cell carcinoma: About 8% of bladder cancers are squamous cell carcinomas. Almost all squamous cell carcinomas are invasive.
Adenocarcinoma: Only about 2% of bladder cancers are adenocarcinomas. The cells of this cancer have much in common with forming cells glands colon cancers. Nearly all adenocarcinomas of the bladder are invasive.
Other less frequent are small cell carcinoma and sarcoma; the first originates in cells resembling nerve cells, called neuroendocrine cells and often these cancers grow rapidly and sarcoma cells originate in the bladder muscle, but rarely occur.
As for the known risk factors for the development of bladder cancer are:
• Snuff: is the most important etiologic agent (2 to 4 times).
• Occupational exposure to aromatic amines or benzenes (rubber, rubber, leather, aluminum, stains, paints, varnishes). The average latency of 18 years.
• Schistosoma haematobium infections.
• Drugs: cyclophosphamide (4 times), phenacetin (2.3 to 12 times) and pelvic radiation therapy.
• Are unclear: hereditary factor and consumption of coffee, tea, alcohol or sweeteners. Most are asymptomatic or may present as painless hematuria (franca or microscopic), as the initial manifestation in 75-80%, pain in advanced stages, irritative symptoms (dysuria, urinary frequency, urinary urgency) in 20% and sometimes obstructive symptoms of upper urinary tract.
In short, the importance of early diagnosis if the patient has any known risk factors or the patient in our case consultation hematuria as an initial manifestation without presenting known risk factors, supported by the use of abdominal ultrasound eliminates uncertainty diagnosis and improve the quality and effectiveness of our interventions. The importance of this case lies in the incorporation of ultrasound as a tool that accompanies the usual physical examination in primary care consultation , which is to increase our response capacity.
References
- Malsmstrom PU (2003) Time to abonbontestinfor microscopic haematuria in adults? BMJ 326: 813-815.
- Haematuria (2008) Evidence-Based diagnosis in primary care. Practical solutions to common problems. Elsevier Butterworth Heineman, Philadelphia, pp: 122-129.
- Hidalgo IM, Garcia Sanchez Lopez MC (2012) My patient consultation ... hematuria. semFYC editions, Barcelona, pp. 302-307.
- Bruyninckx R, Buntinx F, Aertgeerts B, Van CV (2003) The diagnostic value of macroscopic haematuria for the diagnosis of urological cancer in the general practice. Br J Gen Pract 53: 31-35.
- Ferlay J, Autier P, Boniol M, Heanue M, Colombet M, et al. (2007) Estimates of the cancer incidence and mortality in Europe in 2006. Ann Oncol 18: 581-592.
- Sanz M, García L, School T, Castillo MJ, Michael I, et al. (2006) Cancer from other locations, vejiga. AMF Cancer 2: 217-231.
- Palou J, Rodriguez-Rubio F, J HuguetSegarra J, MJ Ribal, Alcaraz A, et al. (2005) Multivariate analysis of clinical parameters of synchronous surface primary bladder cancer and upper urinary tract tumor. J Urol 174: 859-861.
--
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 11768
- [From(publication date):
August-2016 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 10884
- PDF downloads : 884