Research Article Open Access
Black, Asian and Minority Ethnic Communities and Dementia - Where Are We Now?
David Truswell*
Central & North West London NHS Foundation Trust, London, UK
- Corresponding Author:
- David Truswell
Central & North West London NHS Foundation Trust
Stephenson House, 75 Hampstead Road
London, UK
Tel: 44 07969 693215
E-mail: davidtruswell@icloud.com
Received date: March 20, 2014; Accepted date: April 22, 2014; Published date: May 20, 2014
Citation: Truswell D (2014) Black, Asian and Minority Ethnic Communities and Dementia – Where Are We Now? J Alzheimers Dis Parkinsonism 4:152 doi: 10.4172/2161-0460.1000152
Copyright: © 2014 Truswell D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Alzheimers Disease & Parkinsonism
Abstract
Produced for the Race Equality Foundation’s Better Health briefing paper series. The Race Equality Foundation (www.raceequalityfoundation.org.uk) is a UK not-for-profit organization that seeks to influence national policy on support and services for black and minority ethnic communities by developing evidenced-based better practice to promote equality. This briefing looks at developments in the UK since the launch of the National Dementia Strategy in 2009. It uses census data to estimate the number of black and minority ethnic people living with dementia in the UK, and proposes innovative solutions for care, including the use of community dementia navigators. The briefing argues that: • Existing policy recommendations have not been taken into account when developing information and services to meet needs of black and minority ethnic communities. • The prevalence of dementia in some black and minority communities in the UK has been significantly underestimated. • Dementia is misunderstood and highly stigmatized in many UK black and minority ethnic communities. • There is an economic case for financing improvements in ‘living well’ with dementia for people in black and minority ethnic communities, • There should be a vision of a culturally appropriate approach to the dementia pathway that starts from raising awareness, leads to facilitating early diagnosis and lasts into appropriate end-of-life care.
Keywords
Dementia; Black and minority ethnic; Stigma
Introduction
The importance of dementia as an international issue was reinforced in 2012 when the World Health Organization produced a report [1] declaring dementia a ‘public health priority’. The number of people living with dementia worldwide currently stands at 35.6 million, and is expected to double by 2030, and triple by 2050.
The Alzheimer’s Society’s Dementia 2012 [2] reported that annual cost of dementia to the UK economy stood at £23 billion. A significant proportion (36%) of this cost is borne by informal careers.
This briefing is looks at developments in the UK since the launch of the National Dementia Strategy in 2009. It considers the extent to which the Strategy is addressing the information, support and care needs of those in black and minority ethnic communities and ensuring that they are supported in ‘living well’ with dementia. While issues have been raised with the connotations of the term ‘black and minority ethnic [3] this paper is focused on the term as used for self-description by those completing the 2011 Census.
What is Dementia?
‘Dementia’ is a term used to describe a range of illnesses associated with irreversible chemical and neurological changes in the brain that result in progressive functional and behavioural deterioration. Dementia is a terminal illness, usually with an onset in later life. About 60% of people with dementia suffer from Alzheimer’s disease. The life expectancy of those living with Alzheimer’s disease can vary between 5 and 12 years [4]. Vascular dementia makes up another 20% of cases, and most of the remainder is mixed dementias of various kinds.
Available treatments can produce some delay of onset of symptoms but the illness is incurable and there is limited understanding of its origins. However, there are lifestyle changes that can reduce the likelihood of developing some dementias. For example, vascular dementia can result as a sequel to stroke, and improved stroke care can reduce the risk of it developing. The risk of stroke itself can be reduced by a healthy diet and regular exercise which reduces the risk of hypertension.
The UK Dementia Policy Framework and its Implementation
The UK’s National Dementia Strategy [5] is an ambitious programme with 17 key objectives to support people diagnosed with dementia and their careers in ‘living well’ with dementia. The strategy anticipated that significant improvements would be achieved nationally within a 5 year time scale. An important emphasis for the strategy was raising awareness of dementia in the general public and through this reducing stigma and facilitating early diagnosis. The supporting joint commissioning guidance document [6] for the strategy identified black and minority ethnic communities as a group that commissioners should particularly consider ...........to ensure their specific needs are met (DH p.11). This was taken forward in 2010 in the London region with consultation work with black and minority ethnic communities developed by Commissioning Support for London, DH London, the Alzheimer’s Society and the Afiya Trust [7].
The current prime minister, David Cameron gave new impetus to the dementia strategy in 2012 with the Prime Minister’s challenge on dementia [8], which stated that ‘We must ensure that every person gets the treatment and support which meets their needs and their life’ (Older People & Dementia Team p.8). The key focuses of the Prime Minister’s challenge are:
• improved diagnosis;
• better support for careers;
• dementia friendly communities;
• improved research
The first progress report on the Prime Minister’s Challenge [9] highlights the inquiry of the All-Party Parliamentary Group on Dementia (2013) as a source of recommendations for work with dementia in black and minority ethnic communities. However, the progress report itself lacks any vision of these black and minority ethnic communities as integral partners in the implementation of the strategy when it outlines its approach to funding allocations and stakeholder building. In practice black and minority ethnic communities are likely to find themselves late arrivals to strategic discussions that are already dominated by clinical and academic institutional interests. Yet this is an opportunity to take forward previous work (for example, from The Royal College of Psychiatrists [10,11] or the Race Equality Foundation [12,13]) on relevant priorities for healthcare research in relation to black and minority ethnic mental health needs, including dementia, and developing a more active role for black and minority ethnic communities in the design of studies and as co-researchers [14,15].
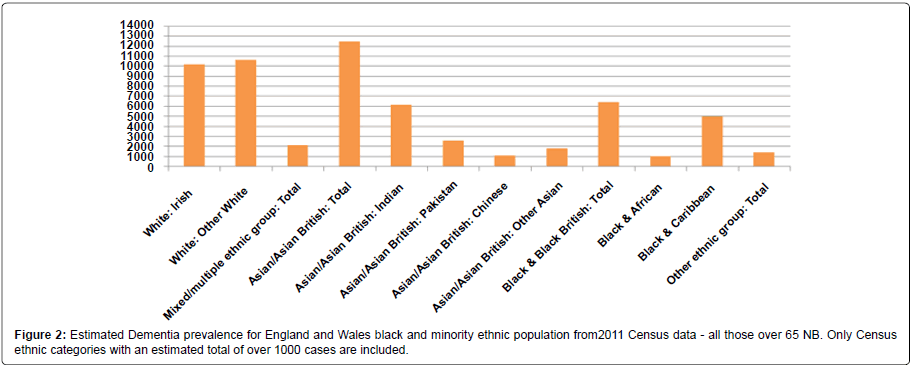
The All Party Parliamentary Group on Dementia’s inquiry report (2013) is significant in placing issues for black and minority ethnic communities and dementia at a national policy and political level not previously seen in the implementation of the National Dementia Strategy. It puts the figure for the number of people in England and Wales from black and minority ethnic groups living with dementia at 25,000, substantially revised from the previous estimate of 15,000 in the 2009 National Dementia Strategy.
While UK minority ethnic populations are generally widely dispersed, these communities are generally concentrated in urban areas [16], making shifts in prevalence estimates of this order challenging for commissioners and the new commissioning structures. Current Joint Strategic Needs Assessments (JSNAs), critical documents for understanding local commissioning priorities, are variable in the attention paid to dementia and few attempt to analyse their dementia information by ethnicity. New commissioning structures could make use of the extensive guidance readily available for working with and commissioning services for black and minority ethnic communities produced by the Race Equality Foundation and other sources [17,18].
Prevalence of Dementia and Black and Minority Ethnic Communities
In the UK there has been very little work done on the impact of dementia in black and minority ethnic communities. However, there are increasing indications that the prevalence of dementia in Black African-Caribbean and South Asian UK populations is greater than the white UK population [19] and that the age of onset is lower for Black African-Caribbean groups than the White UK population [20]. Since these groups are also more likely to experience high blood pressure, it is suggested that the increased risk of vascular dementia contributes to increased prevalence [21].
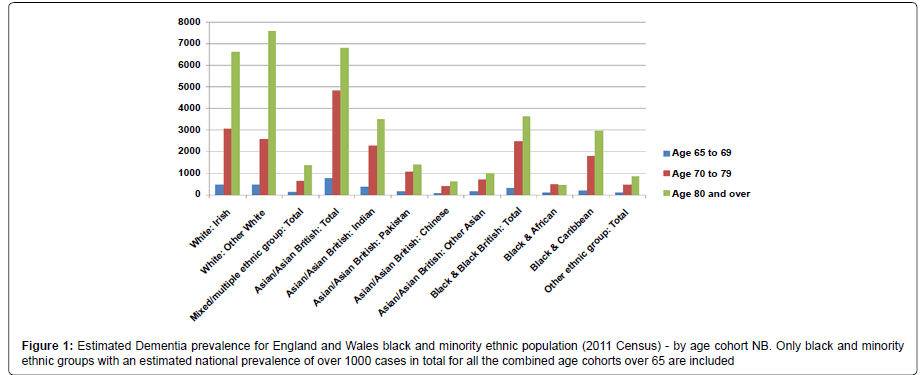
This briefing estimates the prevalence of late onset dementia (over 65) in black and minority ethnic communities using rates identified by the Alzheimer Society [22] and population figures from the 2011 Census.
| Age | % prevalence all dementias |
|---|---|
| 65-69 | 1 in 100 |
| 70-79 | 1 in 25 |
| 80+ | 1 in 6 |
Table 1: Estimated prevalence for all dementias by age cohort (adapted from Demography: Alzheimer’s Society Position Statement).
Differential Impact of Dementia in Black and Minority Ethnic Communities
It should be noted that the numbers of estimated cases in the ‘Other White’ category is substantial. In the UK very few studies exist on stigma, information needs and support issues in relation to these communities. Those UK studies that have been done [23,24] have been very small scale but indicate significant culturally specific values and expectations need to be taken into account. The dearth of research on the Irish population is a concern as it has the estimated highest prevalence of dementia of any ethnic group from the 2011 Census data. The Irish population in the UK is demographically ‘older’ than the native White population. The lack of research on the needs of the Jewish population in relation to dementia is also an area of concern. The 2011 Census indicates that 21% of those identifying themselves as Jewish are over 65.
Lievesley [25] in updating his previous work on the UK black and minority ethnic ageing population [26] has pointed out that the 2011 Census shows that 58% of the black ethnic groups (Black African- Caribbean, Black African and Black other) live in London and also that the Black African-Caribbean population is demographically the ‘oldest’ of the Black ethnic groups. From the 2011 Census data this would mean over 2,700 of those who identified as Black African- Caribbean in the capital over 65 are likely to be living with dementia. It is probable that this figure is considerably underestimated as it assumes that Black African-Caribbean population has the same prevalence of dementia as the indigenous white population, when there are studies to suggest that the prevalence rate is higher [27-29]; that early onset dementia is more prevalent [30] and that the Black African-Caribbean population has greater risk factors for vascular dementia, such as hypertension [31-33].
From the 2011 Census data there is estimated to be over 12,400 people in England and Wales of a South Asian ethnic background over the age of 65 living with dementia, over 5,200 of these living in London.
The small amount of research in the UK on dementia in South Asian communities [34-36] has illustrated the importance of understanding how expectations and obligations regarding care are likely be negotiated within South Asian communities and the challenge of developing effective awareness raising.
Good Practice Examples from a Variety of Black and Minority Ethnic Communities
Meri Yaadain is information and advice service for the South Asian communities in Bradford established in 2006 by the Council’s Adult Services Department. Its website http://www.meriyaadain.co.uk/ is a good example of accessibility to black and minority ethnic communities and they have developed a short DVD for explaining dementia to South Asian communities. Their Caring for Dementia guide is also a useful example an information leaflet setting out both the cultural issues as well as the care issues for South Asian communities.
Culture Dementia UK is an energetic 3rd organization that has been working in Brent for the past 15 years with the African-Caribbean community providing information, a crisis line, a monthly support group and respite. The organization exemplifies the rich network of informal contacts, particularly with the Black African-Caribbean faith communities that are a common feature of voluntary organizations in Black African-Caribbean communities that could be more effectively directly supported by the health and social care mainstream. More information and contact details can be found at http://www. culturedementiauk.org.
Dementia UK http://www.dementiauk.org/ is a national charity which promotes and develops Admiral Nursing - a specialist nursing intervention focused on meeting the needs of families and people with dementia. It is committed to the delivery of person centered, culturally competent care. There are a number of examples of positive practice by Admiral Nurses, in working with black and minority ethnic careers. For example one Admiral Nurse has recently led the development of awareness rising about dementia in the Tamil-speaking community in the Royal Borough of Kingston on Thames with South West London and St. George’s NHS Trust [37]. Central and North West London NHS Trust (CNWL) is currently working with an Admiral Nurse covering Brent and Harrow in developing dementia service information for black and minority ethnic communities. In Haringey, North London, Admiral Nurses have led on the establishment of a culturally inclusive social and therapeutic club (Tom’s Club) [38]. Dementia UK Admiral Nurses in London have extensive experience and knowledge in support black and minority ethnic careers.
An initiative started in Wolver hampton [39] informed by Dementia UK’s work is the development of the post of Asian link worker, where a community nurse fluent in Punjabi and English provides an outreach role to local South Asian communities in raising awareness of dementia as well as advising across the professional spectrum on cultural issues. As well as facilitating greater direct engagement and understanding between the local community and health services, the role ranges flexibly across the primary care and acute hospital interfaces of the dementia pathway.
Jewish Care http://www.jewishcare.org/home have a dementia care and support service based at their Maurice and Vivienne Wohl Campus in North London which supports those living with dementia and their careers across the whole dementia pathway from awareness raising activities to residential care. An important feature is their commitment to being involved with the family throughout the pathway from diagnosis onwards. Their challenges in reaching the Orthodox Jewish community illustrates the limitations inherent in assuming ethnic or religious communities are homogenous.
The Alzheimer’s Society’s Connecting Communities initiative provides dementia community development workers for black and minority ethnic communities in the London Boroughs of Hillingdon, Lambeth, Merton, Enfield, Newham, Red bridge, Hounslow and Croydon. This initiative is committed to working closely with local community groups to develop raising awareness events. The Alzheimer Society also has a nationwide project underway focusing developing awareness raising materials for South Asian communities. The Alzheimer Society’s Dementia Knowledge Centre online at http://www. alzheimers.org.uk is a very good information resource for research and reports on dementia in black and minority ethnic communities.
The Policy Institute for Research on Ageing and Ethnicity (PRIAE) http://www.priae.org/ has been around since 1998 and produced a number of significant documents aimed at the national policy level. They have produced work on people from black and minority ethnic elders in long term care [40] and extra care housing [41] and their website has an extensive collection of reports on dementia care needs across Europe.
The Pepper Pot day centre in London is a 3rd sector day service that has been around since 1981 working with the Black African–Caribbean community providing variety activities including aromatherapy and yoga and respite that has recently taken to using social media https:// www.facebook.com/thepepperpotcentre to enhance its reach.
The London Dementia Strategy Implementation Team explored the use of social media as a peer-led information source such https://www. facebook.com/pages/Resources-for-Dementia-and-Black-Minority- Ethnic-and-Refugee-Communities/ but this approach remains underdeveloped. The same team’s legacy document on information for commissioners on working with black and minority ethnic communities [42] continues to be a useful source for online resources. Successful online initiatives in the wider mental health field such as The Big White Wall http://www.bigwhitewall.com could provide the template for similar developments in the dementia field. There are many 3rd sector organizations that do invaluable work locally supporting people from black and minority ethnic communities that simply lack the time and resources to promote themselves beyond their locality and the growth of on-line resources modelled on the information sharing and informal support of social networking has considerable potential for such organizations. Emerging careers peer support sites such as Yecco http:// www.yecco.com have the potential to be of significant value to black and minority ethnic careers.
The Economic Case
The economic case for investment in raising awareness and developing information dissemination and support services via the BAME 3rd sector has been largely unexplored. There is poor understanding of demand and JSNAs often fail to provide detailed differentiation of black and minority ethnic communities at higher risk, such as the Irish and Black African-Caribbean. The number of older people from these communities in nursing homes is unknown.
Health information about dementia could be more effectively disseminated into black and minority ethnic communities by investing in these communities as a resource for conveying health messages.
The arguments on cost savings from early diagnosis of dementia used in 2009 by Banerjee and Wittenberg [43] can be applied to the economic case for targeting information and resources to support early diagnosis and intervention in dementia for black and minority ethnic communities. This example (Table 2) uses the Personal Social Services Research Unit (PSSRU) costs for 2012 [44] for health and social care to illustrate an invest-to-save case. It is assumed that delaying transfers still incurs some costs for ongoing care provision, and uses PSSRU costs for critical care for social care as an estimate for these costs. It compares the cost per week of different kinds of residential care with the cost saving per week if 100 cases were delayed in transferring to residential care by one week. If there are 2,700 Black African Caribbean people over 65 living with dementia in London, then for every 100 who spend one week longer in the community as a result of targeted early information, the cost saving could be as illustrated.
| PSSRU Provider category |
Cost per resident per week |
Cost per resident per day |
Cost saving per week for 100 cases by 1week delay in transfer |
Less cost of 1 week of Social Care Package Critical care package costs £363 per person per week |
| Private sector nursing homes for older people |
£736 | £105.14 | £73,600 | Less cost of Critical care - saves £37,300 per 100 cases per week |
| Private sector residential care for older people |
£522 | £74.57 | £52,200 | Less cost of Critical care - saves £15,900 per 100 cases per week |
| Local authority residential care for older people |
£1,007 | £143.86 | £100,700 | Less cost of Critical care - saves £64,400 per 100 cases per week |
| Extra care housing for older people |
£428 | £61.14 | £42,800 | Less cost of Critical care - saves £6,500 per 100 cases per week |
| Costing for early interventions | ||||
| Voluntary adult befriending |
£87 for 12 hrs per week |
This could support development of 'black and minority ethnic dementia navigator' | ||
| Targeted black and minority ethnic health promotion campaign |
Unknown as depends on the scale of health promotion campaign |
This could be partly directly invested in black and minority ethnic community groups. It is anticipated that economic benefits would be comparable with those found by Knapp et al in reviewing the benefits of mental health promotion |
||
Table 2: An ‘invest to save’ illustration for using cost saving benefits of delayed transfer to residential home to fund community support services.
The cost saving could be invested in the early interventions outlined and this investment could also provide a useful stimulus for the black and minority ethnic 3rd sector. Commissioners should review existing system dynamic models for modelling dementia costs to input the new Census data and factor in the emerging information on higher prevalence rates for dementia in some black and minority ethnic communities. The cost of rising rates of unscheduled hospital admissions or transfers to residential care that are funded as urgent spot purchases of care packages for complex, late presenting black and minority ethnic patients who have been living in the community with undiagnosed dementia needs to be acted on.
A New Role – A Black And Minority Ethnic Community Dementia Navigator?
Dementia navigators as be frienders who provide support to people living with dementia and help them to find their way around the health and social care system have been identified as good practice in Barnsley (National Dementia Strategy Good Practice Compendium) [46]. Models for community health service navigators for minority ethnic communities are well developed in the US [47] for navigating health systems, and may have a casework focus, as in the case of bilingual patient navigators at the Seattle Children’s Hospital [48]. Navigators are usually fluent in the community language of the person they are supporting and have lived knowledge of their cultural background.
Is it time for a new role focusing on dementia navigators focusing specifically on the information and support issues for black and minority ethnic communities? Such navigators need not be clinical experts but would ideally stay with the person until the end of their life, supporting other professionals, such as the Admiral Nurses. Community dementia navigators could be of particular value in supporting those living alone in black and minority ethnic communities or who have very limited sources of informal help. However such provision of a culturally informed service needs to move beyond the limitations of simple ‘ethnic matching’ which risks importing the negative stereotyping of dementia from the culture of origin into the care relationship. Further work needs to be done on defining cultural competency that achieves a nuanced understanding of the complexity of lives lived out geographically displaced from the culture of origin and involving mixed generational experience of migration and discrimination. This complexity has been highlighted by Jutlla [49] and others [50]. Experience across the NHS following from even such focused national policy initiatives in mental health such as Delivering Race Equality is that cultural competency in service delivery remains a sharp challenge [51].
Although the role would be very challenging, the appointment of black and minority specific dementia navigators could align with the culturally congruent narratives of resilience and spiritual succor which are finding increasingly prominence in end of life care, but remain neglected in the dementia field [52].
As suggested above there is scope for considering this as an ‘invest to save’ opportunity when considered on a local authority or regional scale and could be an economic stimulus to hard pressed minority ethnic community organizations.
Conclusion
There is a worldwide recognition that dementia is the key public health issues for the 21st century, yet there is very little research on the illness despite the fact that it absorbs a significant and rapidly growing amount of expenditure on health and social care. For carers it presents a profound psychological as well as financial burden. Very little is known about the prevalence of dementia in the UK black and minority populations despite some of these communities being at higher levels of risk than the indigenous white population. Policy guidance on understanding the issues for black and minority ethnic communities has not yet found its way into practice in implementing the UK National Dementia Strategy. Information from the 2011 Census indicates that there are substantial increases in the number of people from black and minority communities likely to be living with dementia, but understanding of dementia in such communities is limited and the illness highly stigmatised. A more targeted approach to information and support for people in black and minority ethnic communities living with dementia and their carers must be taken and could be financed through its impact on reducing the rate of transfers to residential care. A whole pathway approach to ‘living well’ with dementia should be developed using a community dementia navigator or some similar role and improved training in cultural competency amongst professionals throughout the pathway for people from black and minority ethnic communities.
Originally published online November 2013 by the Race Equality Foundation www.raceequalityfoundation.org.uk
References
- World Health Organization and Alzheimer’s Disease International (2012) Dementia: a public health priority World Health Organization
- Louise Lakey L., Chandaria K., Quince C., Kane M., and Saunders, T. (2012) Dementia 2012: A national challenge (2012) Alzheimer’s Society
- Jutlla K. (2013) Ethnicity and cultural diversity in dementia care: a review of the research Journal of Dementia Care 21:2 April/June 33-39
- Banerjee S. and Lawrence V (2010) Managing dementia in a multicultural society John Wiley & Sons
- Department of Health (2009) Living well with dementia: A National Dementia Strategy
- Department of Health (2009 Joint Commissioning Framework: National Dementia Strategy
- Truswell D. (2011) Black, minority ethnic and refugee (BMER) communities and the National Dementia Strategy: the London experience Diversity in Health and Care 8:2 , Number 2, June 2011 , 113-119
- Older People and Dementia Team (2012) Prime Minister’s challenge on dementia Delivering major improvements in dementia care and research by 2015 Department of Health
- Department of Health (2013). The Prime Minister's Challenge on Dementia Delivering major improvements in dementia care and research by 2015: Annual report of progress Department of Health
- Royal College of Psychiatrists (2009) Psychiatric services for Black and minority ethnic older people Royal College of Psychiatrists College report CR156
- Oomen G., Bashford J. and Shah A. (2009) Ageing, ethnicity and psychiatric services Psychiatric Bulletin 33 pp30-34.
- Smith F. And Islam-Barrett F. (2011) 'Being Heard: Effective Involvement in local Health and Social Care Decisions for the voluntary sector’ Faith Action and the Race Equality Foundation
- Salway S., Turner D., Ghazala M. , Carter L. Skinner., Bushara B., GerrishK. and Ellison G. (2013) High Quality Healthcare Commissioning: Obstacles and opportunities for progress on race equality Better Health Briefing 28 Race Equality Foundation
- Jolley D., Moreland N., Read K. and Kaur H. (2009) The ‘Twice a Child’ projects: learning about dementia and related disorders within the black and minority ethnic population of an English city and improving relevant services Ethnicity and Inequalities in Health and Social Care 2:4 pp4-8
- Vickers T., Craig G. and Atkin K. (2012) Research with black and minority ethnic people using social care services NIHR School for Social Care Research
- Crosby (2004) G. Developing Policy And Practice For Older People In London Report for Centre for Policy on Ageing
- Imogen Blood I. and Bamford S.-M. (2010) Equality and diversity and older people with high support needs The International Longevity Centre – UK
- Turner D., Salway S., Punita Chowbey P. and Mir G. (2012) Mini Case Study Book Real world examples of using evidence to improve health services for minority ethnic people Evidence and Ethnicity in Commissioning
- Ibid
- Bhattacharyya S., Benbow S. M. and Kar N. (2012) Unmet Service Needs of Ethnic Elders with Dementia in United Kingdom Indian Journal of Gerontology 26:1. 242-258
- Alzheimer's Society Demography: Alzheimer's Society Position Statement (Webpage) http://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=412 Accessed 17/07/13
- Botsford J., Clarke C.L. and Gibb C.E. (2012) Dementia and relationships: experiences of partners in minority ethnic communities Journal of Advanced Nursing 68(10) 2207-2217
- Mukadam N. Cooper C., Basit B. and Livingston G. (2011) Why do ethnic elders present later to UK dementia services? A qualitative study) International Psychogeriatrics 23:7 1070-1077
- The ageing of the ethnic minority populations of England and Wales: findings from the 2011 census (2013) Lievesley N., Centre for Policy on Ageing,
- Lievesley N. (2010 The Future Ageing of the Ethnic Minority Population of England and Wales CPA / Runnymede, 2010
- Adelman S., Blanchard M. and Livingston G. (2009) A systematic review of the prevalence and covariates of dementia or relative cognitive impairment in the older African-Caribbean population in Britain Int J Geriatr Psychiatry 24 657–665.
- Livingston G, Leavey G., Kitchen G. Manela M., Sembhi S. and Katona C. (2001) Mental health of migrant elders- the Islington Study British Journal of Psychiatry 179 361-366
- Managing dementia in a multicultural society (2010)
- Healthcare for London (2009) Dementia Services Guide Appendix 9: Equality Impact Assessment (EqIA) http://www.londonhp.nhs.uk/wp-content/uploads/2011/03/09-Dementia-EqIA.pdf Accessed 11/10/2013
- Adelman S., Blanchard M., Greta Rai G., Leavey G. and Livingston G. (2011) Prevalence of dementia in African–Caribbean compared with UK-born White older people: two-stage cross-sectional study The British Journal of Psychiatry 199, 119–125.
- Moriarty J., Sharif N. and Robinson J. (2011) Black and minority ethnic people with dementia and their access to support and services SCIE Research Briefing 35
- Adelman S. (2009) Prevalence and Recognition of Dementia in Primary care: A Comparison of Older African-Caribbean and White British Residents of Haringey. PhD thesis submission University College London
- Seabrooke V. and Milne M. (2004) Culture and care in dementia. A study of the Asian Community in North West Kent Alzheimer’s and Dementia Support Services
- Seabrooke V. and Milne M. (2009) Early intervention in dementia care in an Asian community Lessons from a dementia collaborative project Quality in Ageing 10:4 18-28
- Jutlla K. and Moreland N. (2009) The personalisation of dementia services and existential realities: understanding Sikh carers caring for an older person with dementia in Wolverhampton Ethnicity and Inequalities in Health and Social Care, 2:4, 10 – 21
- Jackson C. (2008) Spreading the word Mental Health Today Mar 2008
- Orr, K.,Botsford, J., and Efstathiou, K. (2013) Tom’s Clubs: time together Journal of Dementia Care 21: 4 18-19.
- http://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=412
- Patel N. (1999) Black and Minority Ethnic Elderly: Perspectives on Long-Term Care in with With respect to old age : long term care - rights and responsibilities : a report by the Royal Commission on Long Term Care pp257-303 The Stationery Office
- Patel N. and Traynor P. (2006) Developing Extra Care Housing for Black and Minority Ethnic Elders: an overview of the issues, examples and challenges Housing Learning & Improvement Network
- Healthcare for London (2011) Dementia Services Guide Appendix 15 Scoping Report Availability and accessibility of materials and research evidence on Dementia in Black and Minority Ethnic and Refugee (BMER) Communities to support achievement of the dementia services guide objectives in London http://www.londonhp.nhs.uk/wp-content/uploads/2011/03/15-Scoping-Report-and-Resources-Handbook.pdf Accessed 11/10/2013
- http://www.londonhp.nhs.uk/wp-content/uploads/2011/03/09-Dementia-EqIA.pdf
- Curtis L. (2012) Unit Costs for Health and Social Care http://www.pssru.ac.uk/project-pages/unit-costs/2012/ Accessed 11/10/2013
- Knapp M., McDaid and D. and Parsonage M. (eds.) (2011) Mental health promotion and mental illness prevention: The economic case Personal Social Services Research Unit, London School of Economics and Political Science
- Department of Health (South East) (2011) Living well with dementia: A National Dementia Strategy Good Practice Compendium – an assets approach Department of Health (South East)
- http://www.nursingtimes.net/how-a-link-nurse-ensured-equal-treatment-for-people-of-asian-origin-with-dementia/5016160.article Accessed 11/10/2013
- Jackson D (2013) Patient Navigation in a Tertiary Pediatric Healthcare Setting: A Promising Practice for Eliminating Healthcare Disparities 2013 doug jackson diversity rx FINAL.pdf Workshop presentation at Eighth National Conference on Quality Health Care for Culturally Diverse Populations, Oakland, California (March 11-14, 2013) Accessed 11/10/2013
- http://www.londonhp.nhs.uk/wp-content/uploads/2011/03/15-Scoping-Report-and-Resources-Handbook.pdf
- Banerjee S1, Wittenberg R (2009) Clinical and cost effectiveness of services for early diagnosis and intervention in dementia. Int J Geriatr Psychiatry 24: 748-754.
- http://www.pssru.ac.uk/project-pages/unit-costs/2012/
- Regan J, Bhattacharyya S, Kevern P, Rana T (2013) A systematic review of religion and spiritual care pathways in black and minority ethnic populations Mental Health, Religion and Culture 16:1 1-15
- Rush CH (2012) Return on investment from employment of community health workers. J Ambul Care Manage 35: 133-137.
Relevant Topics
- Advanced Parkinson Treatment
- Advances in Alzheimers Therapy
- Alzheimers Medicine
- Alzheimers Products & Market Analysis
- Alzheimers Symptoms
- Degenerative Disorders
- Diagnostic Alzheimer
- Parkinson
- Parkinsonism Diagnosis
- Parkinsonism Gene Therapy
- Parkinsonism Stages and Treatment
- Stem cell Treatment Parkinson
Recommended Journals
Article Tools
Article Usage
- Total views: 17510
- [From(publication date):
August-2014 - Jun 30, 2025] - Breakdown by view type
- HTML page views : 12815
- PDF downloads : 4695