Bismuth Toxicity as a Cause of Parkinsonism
Received: 28-Apr-2023 / Manuscript No. JADP-23-97513 / Editor assigned: 02-May-2023 / PreQC No. JADP-23-97513 (PQ) / Reviewed: 16-May-2023 / QC No. JADP-23-97513 / Revised: 23-May-2023 / Manuscript No. JADP-23-97513 (R) / Published Date: 30-May-2023 DOI: 10.4172/2161-0460.1000569.
Abstract
Parkinsonism” or a “Parkinsonian appearance” describes a cluster of neurologic signs and symptoms related to movement, such as rigidity, tremor, and abnormal gait. The list of causes is wide, the most common and memorable of which are neurodegenerative disorders (such as parkinson’s disease, corticobasal degeneration, multisystem atrophy, and lewy body dementia). There are however iatrogenic causes (such as the use of antipsychotic medication) and, more rarely, toxic encephalopathy. Here we discuss bismuth salicylate, as found in over-the-counter medications, as a cause of parkinsonism in a patient with chronic, unmanaged gastrointestinal symptoms.
Keywords: Parkinson’s disease; Neurotoxicity; Bismuth; Ataxia; Fibromyalgia; Bismuth; Irritable bowel syndrome
Introduction
Bismuth is a rare case of both chronic and acute toxic encephalopathy. Early symptoms can include mood and sleep changes, decline in working memory, and word-finding deficits. Untreated, the condition can progress to Parkinsonism, myoclonus, dysarthria, and seizures. Bismuth toxicity can occur even when used as directed, though it is more likely with supratherapeutic doses. Discontinuation of medication is typically enough to resolve symptoms, though permanent organ damage and death are possible.
Case Presentation
A 64-year-old woman presented to outpatient neurology office with new onset tremor and concerns of a neurodegenerative disorder. The patient described an intermittent resting tremor of both hands (left more than right) and a fine side-to-side tremor of the head. Tremor worsened with fatigue, stress, and anxiety. She describes a feeling of “vibrating or shimmering in chest” or feeling uneasiness when sitting still. She also described subjective mental slowing and difficulty with word finding. Her partner agreed with patient’s description of a slowly progressive tremor but did not feel there were any cognitive deficits. The patient’s past medical history included a distant history of a closed head injury and multiple left leg fractures from a motor vehicle accident more than 30 years prior, resulting in peripheral neuropathy and frequent migraine without aura. The patient also had a history of fibromyalgia, depression and anxiety, and untreated obstructive sleep apnea.
Review of systems revealed several chronic symptoms including neck and back pain, gastrointestinal upset with alternating diarrhea and constipation, and urinary frequency. Her medication list included only duloxetine (Cymbalta) with intermittent use of propranolol as a migraine controller medication. Upon further questioning the patient endorsed several Over-The-Counter (OTC) medications and supplements not listed in her chart, including ginseng, green tea extract, cranberry extract, and significant use of bismuth salicylate (Pepto Bismol), sometimes more than a bottle a day.
Physical exam revealed intention tremor, worse in right hand than left. Patient also showed poor balance in heel-to-toe walk and abnormal gait including stiffness, short stride, and reduced arm swing. Montreal Cognitive Assessment (MOCA) was 30/30. The patient’s handwriting was impeccable, and she easily reproduces complex shapes (such as stars, cubes, and swirls). The patient’s teeth had a slightly grey discoloration which she had not noticed. She was not sure if the discoloration was new. Various laboratory studies were ordered. The patient was asked to discontinue her OTC medication and supplements except for acetaminophen as needed for pain. The patient was advised to return in a few weeks for follow-up and the review the results of her lab work.
The patient returned for her appointment several weeks later and reported a dramatic improvement in symptoms. As her symptoms were improving, the patient had not completed the outpatient labs. On exam her tremor had resolved, and gait had normalized. The patient’s coordination was less than normal on heel-to-toe walk but had improved significantly. The patient was referred to Gastroenterology with instruction to avoid excessive intake of bismuth for her digestive symptoms. She was also advised to meet with her primary care physician to review all her medications as well as over-the-counter medications and supplements. It was recommended she complete outpatient labs, to include as assessment of her kidney function.
Results and Discussion
Bismuth toxicity is a rare cause of Parkinsonism and toxic encephalopathy. Bismuth subsalicylate may be prescribed (as in oral use for treatment for helicobacter pylori or topic use in the treatment of burns) but is most often used as a part of common over-the-counter medications, advertised as a safe option for all manner of gastrointestinal upset. Bismuth toxicity may be chronic or acute in nature, though the insidious nature of chronic toxicity makes it more likely to be seen in the outpatient setting. Bismuth is renally excreted, so risk of toxicity is higher patients with kidney dysfunction. Acute bismuth overdose can also cause acute kidney injury.
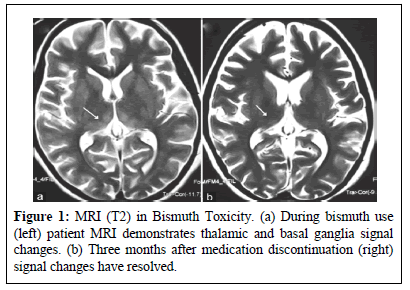
Bismuth toxicity is reversible. Most patients recover within days to weeks of medication discontinuation; however deaths from bismuth toxicity have been reported [1]. No imaging was obtained in this patient’s case, however existing literature demonstrates thalamic and basal ganglia signal changes in patients with bismuth toxicity (Figures 1a and 1b) [2].
This patient’s pain condition likely contributed to her diagnostic quandry. Fibromyalgia is a complex, poorly understood disorder that is often co-morbid with conditions such as anxiety, depression, tendinopathy, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), sleep disorders, irritable bowel syndrome, and interstitial cystitis [3]. In a 2012 study, 80% of physicians stated that they had seen a patient with fibromyalgia in the last 2 years but more than 50% of these physicians felt their knowledge of the disorder was insufficient [4]. Others still question the existence of fibromyalgia as a legitimate medical diagnosis. One study showed that fibromyalgia patients, most of whom are women, were more likely to be perceived as more difficult than patients with other rheumatologic disorders and physicians were more reluctant to accept these patients onto their panels [5]. Studies also show a significant patient-doctor discordance in the relationship between fibromyalgia suffers and rheumatologists [6], the physicians who, arguably, should be most attuned to their needs and concerns.
This patient felt her chronic health issues were not taken seriously by her doctors. As is often the case, patients who feel disrespected, disregarded, or misunderstood by the medical establishment may seek new explanations for their experiences (possibly from less reliable sources) and OTC, alternative, or unapproved treatments for their symptoms [7]. Without the guidance of a medical professional, patients may not be fully educated on the risks of such treatments.
Neither this patient’s record nor medication list included her over-the-counter medications or supplements. It was not discussed during the medication reconciliation at the beginning of her visit nor was her excessive use of bismuth known by her Primary Care Physician (PCP). This information was only discovered after deliberate, in-depth questioning.
Physician efforts towards both satisfaction and clinical thoroughness, however, are often hindered by time constraints. Though primary care physicians are expected to know a patient best and direct their care. Patient satisfaction and trust is largely correlated with appointment length [8], a commodity in short supply in many primary care offices. As such, it may be difficult for PCPs to build patient confidence or be as thorough as they hope to be.
The literature shows several cases of patients diagnosed with neurodegenerative disorders whose symptoms were later resolved after the removal of an offending medication or environmental exposure [2,9,10]. In cases of acute or sub-acute neurological decline a wide differential, including toxic causes, should be considered.
Conclusion
Bismuth toxicity is a rare cause of parkinsonism and sub-acute cognitive decline. Patients may not realize the significant impact over-the-counter medication, supplements, and complementary/alternative medications can have on their health. Health implications of such treatments are especially important in patients with a decreased ability to excrete these medications (such as in renal or liver dysfunction). Furthermore, patients who do not feel adequately helped or heard by their healthcare providers are more likely to seek information and treatment from non-traditional sources, the accuracy and safety of which varies widely. Many over the counter and complementary treatments are well-advertise and widely available, which may give patients the impression they are completely safe and without risk. More must be done to help patients understand risks and side effects.
References
- Borbinha C, Serrazina F, Salavisa M, Viana-Baptista M (2019). Bismuth encephalopathy-a rare complication of long-standing use of bismuth subsalicylate. BMC Neurol 19(1):1-5.
[Crossref] [Google Scholar] [PubMed]
- Siram R, Botta R, Kashikunte C, Pal PK, Yadav R (2017). Chronic encephalopathy with ataxia, myoclonus, and auditory neuropathy: a case of bismuth poisoning. Neurol India 65(1):186.
[Crossref] [Google Scholar] [PubMed]
- Goldenberg DL, Bradley LA, Arnold LM, Glass JM, Clauw DJ (2008) . Understanding fibromyalgia and its related disorders. Prim Care Companion J Clin Psychiatry 10(2):133-44.
[Crossref] [Google Scholar] [PubMed]
- Choy E, Perrot S, Leon T, Kaplan J, Petersel D, et al. (2010). A patient survey of the impact of fibromyalgia and the journey to diagnosis. BMC Health Serv Res 10(1):1-9.
[Crossref] [Google Scholar] [PubMed]
- Aloush V, Niv D, Ablin JN, Yaish I, Elkayam O, et al. (2021). Good pain, bad pain: illness perception and physician attitudes towards rheumatoid arthritis and fibromyalgia patients. Clin Exp Rheumatol 39 (Suppl 130):S54-60.
[Crossref] [Google Scholar] [PubMed]
- Dobkin PL, De Civita M, Abrahamowicz M, Bernatsky S, Schulz J, et al. (2003). Patient-physician discordance in fibromyalgia. J Rheumatol 30(6):1326-34.
[Google Scholar] [PubMed]
- Thorburn S, Faith J, Keon KL, Tippens KM (2013). Discrimination in health care and CAM use in a representative sample of US adults. J Altern Complement Med 19(6):577-81.
[Crossref] [Google Scholar] [PubMed]
- Geraghty EM, Franks P, Kravitz RL (2007). Primary care visit length, quality, and satisfaction for standardized patients with depression. J Gen Intern Med 22:1641-7.
[Crossref] [Google Scholar] [PubMed]
- Stockton-Brown M (2023) Rapidly Progressive Dementia (RPD) in the Setting of Therapeutic Lithium Levels. J Alzheimers Dis Parkinsonism. 13:566.
[Crossref]
- Mignarri A, Chini E, Rufa A, Rocchi R, Federico A, et al. (2013). Lithium neurotoxicity mimicking rapidly progressive dementia. J Neurol 260:1152-4.
[Crossref] [Google Scholar] [PubMed]
Citation: Stockton-Brown M (2023) Bismuth Toxicity as a Cause of Parkinsonism. J Alzheimers Dis Parkinsonism 13: 569. DOI: 10.4172/2161-0460.1000569.
Copyright: © 2023 Stockton-Brown M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1245
- [From(publication date): 0-2023 - Apr 01, 2025]
- Breakdown by view type
- HTML page views: 1035
- PDF downloads: 210