Review Article Open Access
Biomatrices in Urethral Reconstruction
Long Zhang and Yajun Xiao*
Department of Urology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology , Wuhan, Hubei, China
- Corresponding Author:
- Yajun Xiao
Department of Urology, Union Hospital
Tongji Medical College, Huazhong University of Science and Technology
1277 Jiefang Road, Wuhan, Hubei 430022, China
Tel: +86 27 85351625
Fax: +86 27 85726970
E-mail: xiaoyjuh@163.com
Received Date: May 20, 2016; Accepted Date: May 31, 2016; Published Date: June 07, 2016
Citation: Zhang L, Xiao Y (2016) Biomatrices in Urethral Reconstruction. J Biotechnol Biomater 6:231. doi:10.4172/2155-952X.1000231
Copyright: © 2016 Zhang L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Biotechnology & Biomaterials
Abstract
Urethral reconstruction is still a big challenge in urology. Traditionally, the penile skin or buccal mucosa was used as graft for replacement. However, the morbidity of the donor site was reported previously. Furthermore, there is a lack of an adequate autologous donor graft in many cases. The tissue engineered urethra may provide an alternative to the reconstruction. Herein, we reviewed the biomatrices for urethral substitution either in animal model or in clinical cases.
Keywords
Urethral reconstruction; Biomaterials; Urethral stricture
Introduction
Various urethral disorders, such as hypospadias, stricture, require surgical reconstruction [1-3]. The most commonly used sources of graft were penile skin or buccal mucosa [4-7]. However, in many circumstances, an adequate amount of those tissues was not available. In addition, a number of surgical complications were described in previous studies, including prolapse and stricture recurrence [8-10]. Furthermore, bothersome donor site morbidity was associated with buccal mucosa, such as pain, numbness, ulceration and difficulty in opening mouth [11]. Penile skins also have the potential risk of subcutaneous bleeding, infection and the dorsal nerve injury [12].
Recently, the development of regenerative medicine provided novel biomaterials for urethral reconstruction, including natural decellularized matrix, protein derived scaffolds and synthetic polymers. The modification of those materials, such as oxidation with 5% peracetic acid (PAA) or stretch in 90% ethanol, further improves their microstructure and biocompatibility. Herein, we reviewed biomaterials for urethral replacement in brief.
Natural Collagen Based Matrices
The natural collagen based matrices were derived from decellularized heterogenic tissue, including small intestinal submucosa (SIS) [13-15], bladder accellular matrix (BAM) [16-18], accellular corpus spongiosum matrix (ACSM) [19] and accellular dermal matrix (ADM) [20]. Bhargava et al. [20] firstly used ADM and oral cells to fabricate tissue engineered buccal mucosa to repair long complex urethral stricture in 5 patients, the urethra successfully regenerated in 3 of them and maintained functional at mean follow-up of 8 years, however, 2 of them resulted in complete or partial graft removal. Such natural collagen based material for urethral reconstruction was far from ideal. Although the accellular matrix contains biological molecules beneficial for cell growth, there are two main disadvantages that limit further application. One of them is the high density of the material that prevents the transport of nutrient, air and metabolic substance. Another one is the retained heterogenic nuclear components which lead to chronic inflammation, fibrosis and calcification [21,22].
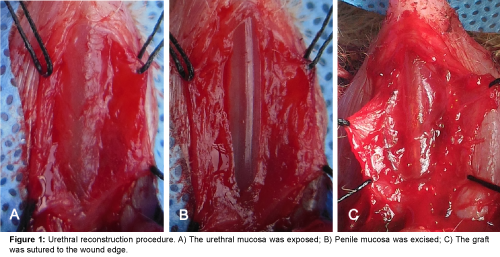
Liu et al. [21] and Wu et al. [22] reported that 5% paracetic acid (PAA) treated SIS and BAM increased the porosity of the fresh SIS, decreased the heterogenic cellular component, and prompted cell proliferation in vitro and in nude mice model. Initially, it was presumed that the maximum distance of the complete healing from the wound edge was 1 cm in a rabbit model [23]. However, Huang et al. [24] demonstrated that unseeded 5% PAA modified BAM could repair long urethral defect (1.5 × 0.8 cm2). In our previous study, we found that 5% PAA treated SIS increased porosity and prompted cell proliferation. In addition, such modified SIS seeded with cells can repair larger urethral defect (1.7 × 1 cm2, Figure 1), the urothelium, smooth muscle and vessel regenerated completely, however, fistula or stricture occurred in unseeded SIS or cell seeded non PAA treated SIS group [25]. Therefore, we considered that cell seeded scaffold and 3-dimension porous microstructure are two important factors to prompt tissue regeneration for large urethral defect.
Protein Derived Scaffolds and Cellulose
Silk fibroin (SF) is a novel protein obtained from Bombyx mori cocoons that have good biocompatibility and low immunogenicity [26,27]. The mechanical property and microstructure of was improved after it was stretched in 90% ethanol [28]. Both accellular and cell seeded SF showed good efficacy in urethral reconstruction in animal model [26,29,30]. Recently, Lv et al. [31] reported a novel oxygen-generating material composed of SF, keratin, calcium peroxide and gelatin. This study showed 3D porous structure, high mechanical property and steady release of oxygen, which improved the urethral tissue regeneration in dogs. There were two novel modified scaffolds using collagen-binding VEGF or collagen/poly (L-lactide-co-caprolactone)-binding Wnt signal inhibitor for urethral reconstruction, both of them showed good efficacy in urethral reconstruction in an animal model [32].
Bacterial cellulose (BC) is obtained from Acetobacter xylinum, it has satisfactory mechanical property, nanostructure and biocompatibility [33]. However, its compact density limits its further clinical application. Huang et al reported that 3D porous structure of BC was formed following the treatment of gelatin, but the mechanical property was still maintained, with the mean tensile strength from 30.45 ± 6.78 Mpa to 16.6 ± 2.47 Mpa. Such modified BC enhanced cell proliferation in vitro and also prompted urethral epithelium, smooth muscle, vessel regeneration in an animal model [34].
Synthetic Polymer
Synthetic polymer materials were once used commonly, such as PGA, PLGA and the compound of PGA:PLGA [35,36]. They avoid potential heterogenic pathogen infection, and have ideal fiber diameter [19]. Raya-Rivera et al. [36] reported that urothelial cell seeded in PGA:PLGA successfully repaired complex urethral stricture in 5 children. The urethrography and flow rate demonstrated the tissue engineered urethra demonstrated wide caliber and satisfactory voiding function. However, the synthetic polymer has poor biocompatibility, and lacks adequate bioactive molecules for cell growth. In addition, it was reported that the degraded substances of the synthetic polymers caused chronic immunogenicity, and development of fibrosis in long term follow up [37].
Conclusion and Future Directions
Compared to traditional non modified biomaterials for urethral reconstruction, the novel biomaterials generally have higher porosity and better histocompatibility. However, the procedure of fabricating such novel materials for urethral replacement is relatively more complicated, including oxidation with 5% PAA and biological molecules binding scaffolds and electrospun biomaterials.
Reconstruction of the urethra is one of the biggest challenges in urology, especially for those patients with long complex extensive fibrosis and stricture. The vascular bed was destroyed in most cases, so the ideal scaffold should be equipped with degradable 3D porous structure to transport the nutrient to the new tissue, exhibit least immunogenicity and can promote neovascularization. Besides, it should also have suitable mechanical property because of the elastic nature of the corpus spongisum. Future studies should be conducted to find the most suitable biomaterials for the urethral reconstruction before its widespread clinical application.
Since the stricture recurrence in clinical cases is relatively high, the underlying mechanisms for the recurrence need to be clarified. The animal models that imitate the urethral stricture in clinical cases should be constructed for further study of the efficacy of different materials in urethral replacement.
References
- Macedo A Jr, Rondon A, Ortiz V (2012) Hypospadias. CurrOpinUrol 22: 447-452.
- Elgammal MA (2009) Straddle injuries to the bulbar urethra: Management and outcome in 53 patients. IntBraz J Urol 35: 450-458.
- Dolk H, Loane M, Garne E (2010) The prevalence of congenital anomalies in Europe. AdvExp Med Biol 686: 349-364.
- Kozinn SI, Harty NJ, Zinman L, Buckley JC (2013) Management of complex anterior urethral strictures with multistage buccal mucosa graft reconstruction. Urology 82: 718-723.
- Lee YJ, Kim SW (2013) Current management of urethral stricture. Korean J Urol 54: 561-569.
- Chandrasekharam VV (2013) Single-stage repair of hypospadias using longitudinal dorsal island flap: Single-surgeon experience with 102 cases. Indian J Urol 29: 48-52.
- Djordjevic M, Majstorovic M, Stanojevic D, Bizic M, Ducic S, et al. (2008) One-stage repair of severe hypospadias using combined buccal mucosa graft and longitudinal dorsal skin flap. Eur J Pediatric Surgery 18: 427-430.
- Aulagne MB, Harper L, de Napoli-Cocci S, Bondonny JM, Dobremez E (2010) Long-term outcome of severe hypospadias. J PediatrUrol 6: 469-472.
- Bhatnagar A, Upadhyaya VD, Kumar B (2012) Congenitalurethrocutaneous fistula: Case report with review of literature. Indian J PlastSurg 45: 563-565.
- Cimador M, Vallasciani S, Manzoni G, Rigamonti W, De Grazia E, et al. (2013) Failed hypospadias in paediatric patients. Nat Rev Urol 10: 657-666.
- Xu YM, Xu QK, Fu Q, Sa YL, Zhang J, et al. (2011) Oral complications after lingual mucosal graft harvesting for urethroplasty in 110 cases. BJU Int 108: 140-145.
- Ademuyiwa AO, Ojewola RW, Elebute OA, Jeje EA, Bode CO (2012) Surgically correctable morbidity from male circumcision: Indications for specialist surgical care in Lagos. Niger J Surgery 18: 71-74.
- Fiala R, Vidlar A, Vrtal R, Belej K, Student V (2007) Porcine small intestinal submucosa graft for repair of anterior urethral strictures. EurUrol 51: 1702-1708.
- Palminteri E, Berdondini E, Colombo F, Austoni E (2007) Small intestinal submucosa (SIS) graft urethroplasty: Short-term results. Eururol 51: 1695-1701.
- Palminteri E, Berdondini E, Fusco F, De Nunzio C, Salonia A (2012) Long-term results of small intestinal submucosa graft in bulbar urethral reconstruction. Urology 79: 695-701.
- Li C, Xu YM, Song LJ, Fu Q, Cui L, et al. (2008) Urethral reconstruction using oral keratinocyte seeded bladder acellular matrix grafts. J Urol 180: 1538-1542.
- Li H, Xu Y, Xie H, Li C, Song L, et al. (2014) Epithelial-differentiated adipose-derived stem cells seeded bladder acellular matrix grafts for urethral reconstruction: An animal model. Tissue Eng Part A 20: 774-784.
- Li C, Xu YM, Liu ZS, Li HB (2013) Urethral reconstruction with tissue engineering and RNA interference techniques in rabbits. Urology 81: 1075-1080.
- Feng C, Xu YM, Fu Q, Zhu WD, Cui L, et al. (2010) Evaluation of the biocompatibility and mechanical properties of naturally derived and synthetic scaffolds for urethral reconstruction. J Biomed Mater Res A 94: 317-325.
- Bhargava S, Patterson JM, Inman RD, MacNeil S, Chapple CR (2008) Tissue-engineered buccal mucosa urethroplasty-clinical outcomes. EurUrol 53: 1263-1269.
- Liu Y, Bharadwaj S, Lee SJ, Atala A, Zhang Y (2009) Optimization of a natural collagen scaffold to aid cell-matrix penetration for urologic tissue engineering. Biomaterials 30:3865-3873.
- Wu S, Liu Y, Bharadwaj S, Atala A, Zhang Y (2011) Human urine-derived stem cells seeded in a modified 3D porous small intestinal submucosa scaffold for urethral tissue engineering. Biomaterials 32:1317-1326.
- Dorin RP, Pohl HG, De Filippo RE, Yoo JJ, Atala A (2008) Tubularized urethral replacement with unseeded matrices: What is the maximum distance for normal tissue regeneration? World J Urol 26: 323-326.
- Huang JW, Xie MK, Zhang YY, Wei GJ, Li X, et al. (2014) Reconstruction of penile urethra with the 3-dimensional porous bladder acellular matrix in a rabbit model. Urology 84:1499-1505.
- Zhang L, Du A, Li J, Pan M, Han W, et al. (2016) Development of a cell-seeded modified small intestinal submucosa for urethroplasty. Heliyon 2:e00087.
- Chung YG, Tu D, Franck D, Gil ES, Algarrahi K, et al. (2014) Acellular bi-layer silk fibroin scaffolds support tissue regeneration in a rabbit model of onlayurethroplasty. PLoS One 9: e91592.
- Gomez P, Gil ES, Lovett ML, Rockwood DN, Di Vizio D, et al. (2011) The effect of manipulation of silk scaffold fabrication parameters on matrix performance in a murine model of bladder augmentation. Biomaterials 32:7562-7570.
- Fan S, Zhang Y, Shao H, Hu X (2013) Electrospun regenerated silk fibroin mats with enhanced mechanical properties. Int J BiolMacromol 56: 83-88.
- Xie M, Song L, Wang J, Fan S, Zhang Y, et al. (2013) Evaluation of stretched electrospun silk fibroin matrices seeded with urothelial cells for urethra reconstruction. J Surg Res 184: 774-781.
- Xie M, Xu Y, Song L, Wang J, Lv X, et al. (2014) Tissue-engineered buccal mucosa using silk fibroin matrices for urethral reconstruction in a canine model. J Surg Res 188: 1-7.
- Lv X, Li Z, Chen S, Xie M, Huang J, et al. (2016) Structural and functional evaluation of oxygenating keratin/silk fibroin scaffold and initial assessment of their potential for urethral tissue engineering. Biomaterials 84: 99-110.
- Zhang K, Guo X, Zhao W, Niu G, Mo X, et al. (2015) Application of Wntpathway inhibitor delivering scaffold for inhibiting fibrosis in urethra strictures: In vitro and in vivo study. Int J MolSci 16: 27659-27676.
- Lv X, Yang J, Feng C, Li Z, Chen S, et al. (2015) Bacterial cellulose-based biomimetic nanofibrousscaffold with muscle cells for hollow organ tissue engineering. ACS Biomaterials Science and Engineering 2: 19–29.
- Huang JW, Lv XG, Li Z, Song LJ, Feng C, et al. (2015) Urethral reconstruction with a 3D porous bacterial cellulose scaffold seeded with lingual keratinocytes in a rabbit model. Biomed Mater 10:055005.
- Fu Q, Deng CL, Zhao RY, Wang Y, Cao Y (2014) The effect of mechanical extension stimulation combined with epithelial cell sorting on outcomes of implanted tissue-engineered muscular urethras. Biomaterials 35: 105-112.
- Raya-Rivera A, Esquiliano DR, Yoo JJ, Lopez-Bayghen E, Soker S, et al. (2011) Tissue-engineered autologous urethras for patients who need reconstruction: An observational study. Lancet 377: 1175-1182.
- Ceonzo K, Gaynor A, Shaffer L, Kojima K, Vacanti CA, et al. (2006) Polyglycolic acid-induced inflammation: Role of hydrolysis and resulting complement activation. Tissue Eng 12: 301-308.
Relevant Topics
- Agricultural biotechnology
- Animal biotechnology
- Applied Biotechnology
- Biocatalysis
- Biofabrication
- Biomaterial implants
- Biomaterial-Based Drug Delivery Systems
- Bioprinting of Tissue Constructs
- Biotechnology applications
- Cardiovascular biomaterials
- CRISPR-Cas9 in Biotechnology
- Nano biotechnology
- Smart Biomaterials
- White/industrial biotechnology
Recommended Journals
Article Tools
Article Usage
- Total views: 12425
- [From(publication date):
June-2016 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 11537
- PDF downloads : 888