Case Report Open Access
Biliary Esophagitis: A Case Report
Nicholas J Demos*, Ioana Agams and Tara J BeckerDepartment of Surgery, Hoboken University Medical Center, Hoboken, New Jersey, USA
- *Corresponding Author:
- Demos NJ
Department of Surgery, Hoboken University Medical Center
Hoboken, New Jersey, USA
Tel: +12014181000
E-mail: ndemos09@gmail.com
Received date: September 04, 2017; Accepted date: September 25, 2017; Published date: September 29, 2017
Citation: Demos NJ, Agams I, Becker TJ (2017) Biliary Esophagitis: A Case Report. J Gastrointest Dig Syst 7:529. doi:10.4172/2161-069X.1000529
Copyright: © 2017 Demos NJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Bile reflux esophagitis has been reported and discussed in the literature for many years. What makes our case unusual are the gross and microscopic photos of bile in the esophageal mucosa. The pertinent literature is discussed especially the deleterious and oncogenic effects of bile in the esophageal mucosa.
Keywords
Mucosa; Esophageal mucosa; Hiatal hernia; Biliary tract
Case Report
A 76 year old woman was admitted to Christ Hospital, Jersey City, New Jersey on March 27, 2004, with intractable bilious vomiting. On examination she was found to have severe dehydration, prostrations and atrial fibrillation with hypertension. She appeared to have continuous bilious vomiting, spilling on her bed.
Rales were present on the left lower chest. Past history revealed 20 prior hospitalizations with malnutrition, vomiting, anaemia and urgent and chronic diabetic care. Four months previously, she was admitted for removal of infected right pectoral pacemaker and replacement with a new one in the left pectoral area.
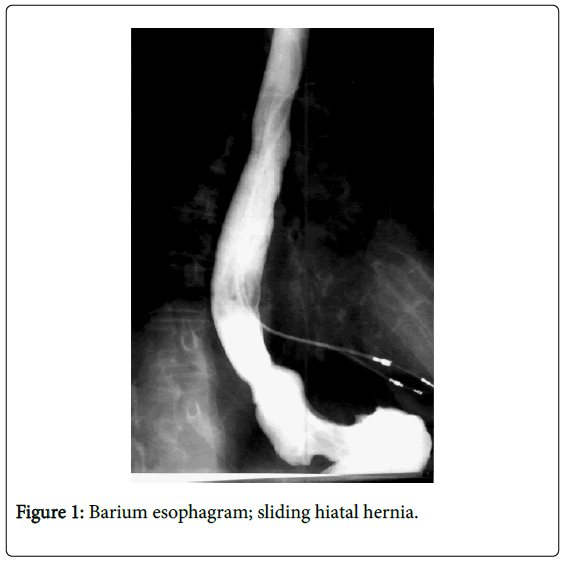
Work-up revealed a gastrointestinal series, oropharyngeal dysphagia, esophagogastric paresis, and hiatal hernia with severe gastroesophageal reflux (Figure 1). Other tests revealed severe anemia, fundal esophagitis, severe malnutrition, left lower lobe atelectasis and pneumonia. Electrocardiogram revealed atrial fibrillation, sick sinus syndrome and a functioning pacemaker. Echocardiogram showed normal left ventricular size and contractility and mild left atrial enlargement. Bacterial culture revealed gram positive bacterium and urinary infection.
A left subclavian catheter and a nasogastric catheter were inserted. Nevertheless, she kept vomiting bile. On April 22, 2004, I was called on consultation and performed an upper gastrointestinal fiberoptic endoscopy. Photograph revealed pronounces gastritis and a large hiatal hernia (Figure 2).
The esophagogastric area revealed mucosal biliary staining and Barret’s esophagus (Figure 3). Biopsies confirmed the Barret’s ulcers of esophagus (Figures 4 and 5).
The black spots in these pictures were negative for melanin and hemosiderin. No chemical tests for bile were available. The patient’s relatives refused surgical correction at this time and for the next two months.
The patient was treated for two months. A percutaneous fiberoptic gastrostomy was performed. Diabetic management, antibiotics, and antacids were given. Vomiting continued even though to a lesser extent. Two months after admission, repeat upper endoscopy was performed revealing clearing of bile staining but confirming the Barrett’s metaplasia (Figure 6). She was discharged and two months later she was readmitted to a different hospital for a repeat percutaneous gastrostomy. On November 6, 2004, she died at the nursing home.
Discussion
This case report emphasizes the destructive and fatal results of long standing gastroesophageal reflux. Bile esophagitis was present in our patient. The additional effects of bile on the esophageal mucosa are seen in Figures 3-5. Jiang has described esophagitis in children caused by bile and acid [1]. Eros described bile induced ATP depletion, vast cell degranulation and tissue damage in dogs, all of which could be prevented by choline antagonists. Severe inflammation in the submucosa but no bile was seen [2]. Aiyer also studied the bile changes in esophageal mucosa but no bile was seen in biopsies [3]. Mitros’s Atlas of extensive study of gastrointestinal pathology mentions bile gastritis but no bile esophagitis [4].
Bile plays a role with refluxed acid in the development of Barrett’s esophagus and its malignant transformation, according to Peters and colleagues [5]. In our case, visual evidence of bile staining had disappeared two months later (Figure 6). Perhaps the injury to the esophageal mucosa had occurred or it may have continued, since Barrett’s metaplasia continued in the second endoscopy (Figure 6).
Refusal of operation was unfortunate. The patient’s aspiration pneumonia cleared. The diabetes was under control. Echocardiogram revealed normal ventricular size and contractibility. The intended surgical correction carried no formidable risk. We had ample experience of surgical correction. In 1999, we published a 24 year follow-up of our stapled uncut gastroplasty in 161 patients. Only one fatality occurred in an emergency operation [6,7]. Our patient expired seven months after the first endoscopy in a nursing facility.
References
- Jiang M, Chen J, Chen F, Yu J, Liang J, et al. (2009) Bile and acid reflux in the pathogenesis of reflux oesophagitis in children. J Paediatr Child Health 45: 64-67.
- Eros G, Kaszaki J, Czobel M, Boros M (2006) Systemic phosphatidylcholine pretreatment protects canine esophageal mucosa during acute experimental biliary reflux. World J Gastroenterol 12: 271-279.
- Aiyer HS, Li Y, Harper N, Myers SR, Martin RC (2011) Molecular changes in the esophageal epithelium after a subchronic exposure to cigarette smoke in the presence of bile-acid reflux. Inhal Toxicol 23: 304-311.
- Mitros FA, Winawer SJ, Lu CC (1988) Atlas of gastrointestinal pathology. Philadelphia, Lippincott.
- Peters JH, Reveiller M, Ghatak S, Toia L, Kalatskaya I, et al. (2012) Bile exposure inhibits expression of squamous dfferentiation genes in human esophageal epithelial cells. Ann Surg 255: 1113-1120.
- Demos NJ, Ahmad I, Scalia J, Wu J, Zaklama S, et al. (1998) The esophagogastric junction: 420 questions, 420 answers. J Libbey Eurotext, France pp: 884-891.
- Demos NJ (1999) The stapled, uncut gastroplasty for hiatal hernia: 24 years’ follow-up. Dis Esophagus 12: 14-21.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 3259
- [From(publication date):
October-2017 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 2627
- PDF downloads : 632