Biased Estimates for 30-day Mortality Rates Post Myocardial Infarction-Impact of Inter-Hospital Transfers
Received: 19-Sep-2016 / Accepted Date: 21-Oct-2016 / Published Date: 28-Oct-2016 DOI: 10.4172/2161-1165.1000271
Abstract
Background: Acute myocardial infarction (AMI) patients are frequently transferred to tertiary care facilities for advanced procedures. Exclusion of transferred patients can result in biased estimates, especially if the focus is on a population-based cohort. The potential magnitude of this bias remains unknown. We assessed the impact of excluding transferred patients on 30-day AMI mortality estimates, over a 10-year period. Methods: All AMI hospitalizations to acute care hospitals in British Columbia, from 2000 to 2009, were captured. Transfers were defined as a discharge from the index AMI hospitalization to another hospital. We compared transfer rates by sex, age and year using logistic regression models. Age- and sex-specific 30-day AMI mortality rates and the sex odds ratios (OR) were estimated, regardless of transfer status, and for the sub-cohort excluding transferred patients. Results: Of 63,310 AMI patients, 40.6% had at least one transfer out of the index AMI hospital. Men and younger patients were more likely to be transferred. Transfer rates increased over time in all age groups regardless of sex. Overall, when transfers were excluded, 30-day AMI mortality rates were overestimated (absolute difference of 5.5% in women and 6.7% in men). Furthermore, the 30-day mortality OR (women vs. men) was underestimated: transfer outs excluded (OR=1.25, 95% CI: 1.19, 1.31) vs. all patients included (OR=1.49, 95% CI: 1.42, 1.56). Conclusions: 30-day mortality may be overestimated in population-based analyses when transfers are excluded, while the sex difference is underestimated. The observed bias is strongly affected by the magnitude and time trends of transfer rates.
Keywords: Myocardial infarction; Bias; Inter-hospital transfers; Mortality
165137Introduction
Patients hospitalized for an acute myocardial infarction (AMI) are often transferred to tertiary care facilities to receive advanced cardiac care and procedures, such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG), if these procedures are not available at the admitting hospitals. In the literature, the reported proportion of AMI patients who are transferred varies widely due to a number of factors including the population of interest, the definition of patient transfer and the structure of the health care system (i.e. presence/absence of a regional cardiac care model). Anywhere from 7% to more than 40% of all AMI patients admitted to hospital can be transferred out to other hospitals at least once during their care [1-3]. Similarly, there are varying findings with respect to the temporal changes in patient transfer rates, with rising rates in some settings and stable or declining rates in others [2,4].
In AMI outcomes research, patient transfers can introduce a methodological challenge in settings where ascertaining patient outcomes across multiple hospitals is not feasible. Transferred patients are commonly excluded from the analyses of registries or populationbased epidemiological studies if unique patient identifiers cannot be linked across multiple data holdings. For instance, in a large, national AMI registry in the United States, focused on assessing the sex differences in 30-day AMI mortality, as many as 40% of patients were identified as being transferred out and were subsequently excluded from all analyses [2]. The main finding of this study was that the excess mortality risk observed among women had diminished over time. Similarly, based on the findings of Acute Coronary Syndrome Treatment and Intervention Outcomes Network (ACTION) registry and AHA’s Get With the Guidelines (GWTG), transfers out of the index hospital ranged from 2% of the top performing hospital to 21% among the lowest performing hospitals [3].
What are the implications of such exclusions of transferred patients on the estimates of AMI outcomes? Does it introduce bias? What is the direction and extent of such bias? Would the impact vary by sex and/or by age? Would it influence the estimated magnitude of women’s excess mortality risk, post AMI? Despite the fact that hospital transfers affect a significant proportion of AMI patients, the answers to these important questions largely remain unknown. Addressing these questions can guide future study designs, as well as interpretation and comparison of findings from AMI outcomes research and hospital performance studies where the proportion of transferred patients vary or where transferred patients are handled differently across analyses.
In British Columbia (BC), we are able to access and link administrative, clinical, and outcome data on all AMI patients admitted to acute care hospitals regardless of their transfer status. We, therefore, aimed to assess the impact of excluding transferred out patients on estimates of 30-day mortality post AMI. Specifically, our objectives were to: 1) determine whether inter-hospital transfer rates vary by sex, age and over time, 2) determine whether excluding transferred patients impacts the estimated age- and sex- specific 30- day mortality rates, and 3) determine the impact, if any, on the magnitude of the excess mortality risk often observed among women, compared to men.
Methods
Study population and data sources
This is a population-based, retrospective cohort study of AMI patients ≥ 20 yrs of age admitted to acute care hospitals in BC, between January 1, 2000 and December 31, 2009. We identified these patients using the BC Ministry of Health's Discharge Abstract Database (DAD) [5] and linked their records to the BC Vital Statistics Deaths registry [6]. The DAD is an administrative database, which contains clinical information on all hospitalizations and transfers as well as diagnosis codes and some patient demographics. The identification of AMI diagnosis and comorbidities based on DAD data has been previously validated [7-10]. The Vital Statistics Deaths registry provided dates for all deaths in BC. Since cause of death is not reliably coded, we used allcause mortality for our analysis. We obtained approval from the University of British Columbia Clinical Research Ethics Board to conduct this study.
Using the DAD, we defined AMI based on the International Classification of Disease (ICD) codes, 410 (ICD-9, prior to April 2001) and I21, I22 (ICD-10), found in any diagnostic field, excluding any admission for which AMI was a post-admission complication. The ICD-10 coding for differentiating ST-segment elevation MI (STEMI) vs. Non-ST-segment elevation MI (NSTEMI) diagnosis was not available for the entire study period, and therefore not used in the analysis. The study cohort was limited to index AMI hospitalizations, which were defined as any AMI hospitalization with no previous AMI hospitalization within the prior 365 days. We defined an inter-hospital patient transfer (henceforth referred to as hospital transfer) as a discharge from the index AMI admission hospital to another acute care hospital (i.e. transfer out). Linking all hospitals transfers together defined a single episode of care for a given patient. AMI hospitalizations with transfers to multiple hospitals within the same episode of care were counted only once.
We defined 30-day mortality following an AMI as any death, either in-hospital or out-of-hospital, within 30 days of a patient’s index AMI hospitalization. We characterized the study population based on sex, age and year of hospitalization, and comorbidities including diabetes, heart failure, cerebrovascular disease, chronic renal failure, pulmonary edema, cardiac dysrhythmias, and cancer. We also used the Charlson Index score as an overall measure of burden of comorbidities. The predictive performance of the Charlson Index score (based on ICD-9 and ICD-10 diagnostic codes in administrative data) for short- and long-term mortality has been previously validated [11,12]. Other important patient variables such as socioeconomic status or ethnicity were not available in our data sources.
We excluded 713 hospitalizations (1.1%) that were either nonurgent or non-emergent (potentially invalid AMI coding), or records with no reported sex, as well as those for which data linkage could not be performed (i.e., non-BC residents).
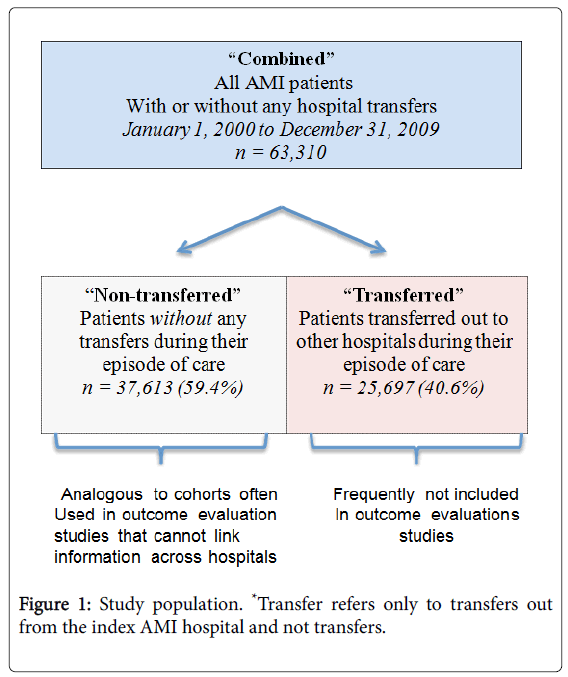
To evaluate the impact of excluding transfers on estimates of 30-day mortality, we created three groups of patients based on their transfer status: 1) the ‘combined’ cohort which includes all AMI patients with or without hospital transfers, 2) the ‘non- transferred’ sub-cohort which includes only patients without any hospital transfers and is analogous to the type of cohort often used in outcome evaluation studies that cannot link information across hospitals, and 3) the ‘transferred’ sub-cohort which includes only patients who were transferred out to other hospitals during their episode of care (Figure 1).
Statistical analysis
Demographics and baseline comorbidities were summarized by transfer status using median and interquartile range for age, and counts and percentages for categorical variables. Time trends were based on combining two years intervals. Age was grouped into four categories, 20-55, 56-64, 65-74 and ≥ 75 yrs old. Transfer rate was estimated as the proportion of patients being transferred from the index AMI hospitalization and was compared across age groups using a chi-square test. Since the ‘transferred’ and ‘non-transferred’ groups are sub-cohorts of the ‘combined’ cohort, and thus not independent of each other, no testing between the ‘combined’ cohort and either of the sub-cohorts was done.
Logistic regression models were constructed for the odds of being transferred to examine the impact of age, sex and time (i.e. AMI hospitalization year); all two- and three-way interactions for age, sex and time were explored, however, the final model included only the two-way interactions because the three-way interaction was not significant. Thirty-day morality rates were described using percentages by sex, age and transfer status and sex differences were tested for each age and transfer group with a chi- square test. The bias in the estimated 30-day mortality rates of the ‘non-transferred’ sub-cohort was calculated as its difference from the estimated mortality rates of the ‘combined’ cohort.
To understand the impact of the transferred patients on the estimated sex gap, the 30-day mortality odds ratio (OR) and 95% confidence intervals (CI) for women vs. men were estimated using logistic regression models for sex only and additionally adjusting for age, time, and the significant 2-way interactions among age, sex and year, based on data from the ‘combined’ cohort and the ‘nontransferred’ sub- cohort, respectively. All analyses were conducted using SAS version 9.4 (Cary, NC).
Results
Study population
During our 10-year study period, there were 64,023 AMI hospitalizations in BC. After exclusions (n=713), a total of 63,310 index AMI hospitalizations were included in our study and formed the ‘combined’ cohort, which includes all hospitalizations regardless of transfer status. Among AMI cases in the ‘combined’ cohort, 37,613 (59.4%) had no hospital transfers during their episode of care (i.e. the ‘non-transferred’ sub-cohort).
The remaining 25,697 (40.6%) patients had at least one interhospital transfer during their episode of care (i.e. the ‘transferred’ subcohort).
The baseline characteristics of these three groups, ‘combined’, ‘nontransferred’ and ‘transferred’, are summarized in Table 1. Overall, the median age of the patients in the ‘combined’ cohort was 72 yrs with 35.0% being women. The ‘transferred’ patients were younger (median age: 65 yrs), and less likely to be women (28.6%).
| Combined | Non-transferred | Transferred | ||||
|---|---|---|---|---|---|---|
| n = 63,310 | n = 37,613 | n = 25,697 | ||||
| Women n =22,187 |
Men n =41,123 |
Women n =14,831 |
Men n =22,782 |
Women n =7,356 |
Men n =18,341 |
|
| Median Age (Q1, Q3) | 78 (67, 84) | 68 (57, 78) | 81 (73, 86) | 73 (60, 82) | 70 (60, 78) | 63 (54, 72) |
| Shock, n (%) | 465 (2.1) | 778 (1.9) | 323 (2.2) | 516 (2.3) | 142 (1.9) | 262 (1.4) |
| Diabetes, n (%) | 5621 (25.3) | 9454 (23) | 3738 (25.2) | 5565 (24.4) | 1883 (25.6) | 3889 (21.2) |
| Heart Failure, n (%) | 5287 (23.8) | 6626 (16.1) | 4131 (27.9) | 4687 (20.6) | 1156 (15.7) | 1939 (10.6) |
| Cancer, n (%) | 539 (2.4) | 1094 (2.7) | 455 (3.1) | 864 (3.8) | 84 (1.1) | 230 (1.3) |
| Cerebrovascular Disease, n (%) | 684 (3.1) | 955 (2.3) | 573 (3.9) | 720 (3.2) | 111 (1.5) | 235 (1.3) |
| Pulmonary Edema, n (%) | 156 (0.7) | 172 (0.4) | 114 (0.8) | 117 (0.5) | 42 (0.6) | 55 (0.3) |
| Acute Renal Failure, n (%) | 1083 (4.9) | 1694 (4.1) | 901 (6.1) | 1311 (5.8) | 182 (2.5) | 383 (2.1) |
| Chronic Renal Failure, n (%) | 1285 (5.8) | 2191 (5.3) | 1054 (7.1) | 1671 (7.3) | 231 (3.1) | 520 (2.8) |
| Cardiac Dysrhythmias, n (%) | 3802 (17.1) | 5989 (14.6) | 2886 (19.5) | 3894 (17.1) | 916 (12.5) | 2095 (11.4) |
| Charlson Index ≥ 5, n (%) | 1147 (5.2) | 1729 (4.2) | 962 (6.5) | 1402 (6.2) | 185 (2.5) | 327 (1.8) |
Note: ‘Combined’ cohort includes all AMI patients with or without hospital transfers within an episode of care, ‘Non-transferred’ sub-cohort includes only patients without any hospital and ‘Transferred’ sub-cohort includes only patients who were transferred to other hospitals during their episode of care.
Table 1: Baseline patient characteristics.
Additionally, irrespective of sex, transferred patients had fewer baseline comorbid conditions than non-transferred patients. Thus, the exclusion of the transferred patients resulted in a cohort of patients (i.e. ‘non-transferred’ sub-cohort) who were older (median age: 76 yrs), more likely to be women (39.4%) and with more comorbidities at their index hospitalization, as compared to the ‘combined’ cohort.
It is important to note that women who were not transferred were the oldest and had the greatest burden of comorbidities compared to all other patients.
Trends in hospital transfer rates
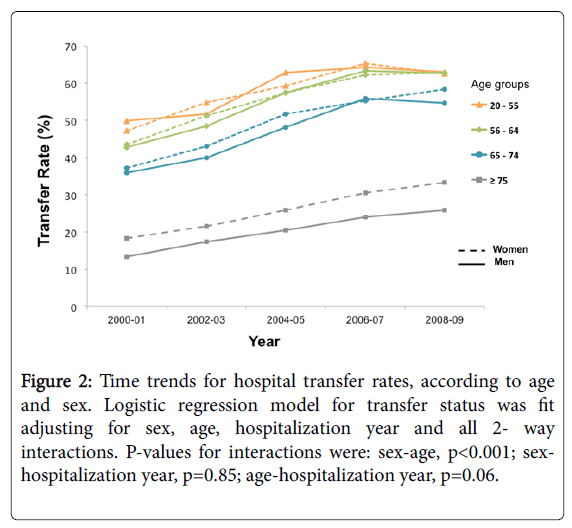
The proportion of AMI patients who were transferred at least once during their episode of care decreased with increasing age, from 58.1% in the 20-55 age group to 23.2% in the ≥ 75 age group (Table 2). The transfer rates differed by sex, with older men (>65 yrs) transferred more than older women (>65 yrs), (age-sex interaction p-value<0.001).
| Age groups (years) | Transfer Rate n (%) | P-value for sex difference* | ||
|---|---|---|---|---|
| Overall n=25,697 |
Women n=7,356 |
Men n=18,341 |
||
| 20-55 | 6,498 (58.1) | 1,244 (58.7) | 5,254 (58.0) | 0.51 |
| 56-64 | 6,196 (56.0) | 1,408 (55.3) | 4,788 (56.2) | 0.42 |
| 65-74 | 6,752 (48.0) | 2,048 (46.5) | 4,704 (48.7) | 0.01 |
| ≥ 75 | 6,251 (23.2) | 2,656 (20.3) | 3,595 (25.9) | <0.001 |
*Logistic regression model for transfer status was fit adjusting for sex, age, hospitalization year and all 2- way interactions with sex, age and hospitalization year. Only the sex-age interaction was significant (p<0.001). P-value for sex-hospitalization year interaction was 0.86 and for age-hospitalization year interaction was 0.06.
Table 2: Distribution of hospital transfers in the combined cohort, according to age and sex.
Furthermore, over the 10-year study period, similar increases in transfer rates were observed across all age groups (age-year interaction p-value=0.06), and for both men and women (sex-year interaction pvalue= 0.85) (Figure 2).
Figure 2: Time trends for hospital transfer rates, according to age and sex. Logistic regression model for transfer status was fit adjusting for sex, age, hospitalization year and all 2- way interactions. P-values for interactions were: sex-age, p<0.001; sexhospitalization year, p=0.85; age-hospitalization year, p=0.06.
Impact of excluding transferred patients on 30-day mortality rate estimates
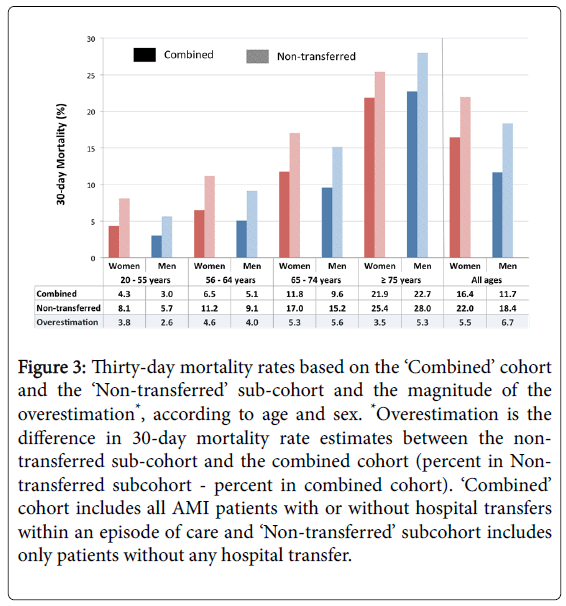
Overall, the estimated 30-day mortality rate for the ‘nontransferred’ sub-cohort was higher than the estimate for the ‘combined’ cohort, 19.8% vs . 13.3%, respectively (Figure 3).
Figure 3: Thirty-day mortality rates based on the ‘Combined’ cohort and the ‘Non-transferred’ sub-cohort and the magnitude of the overestimation*, according to age and sex. *Overestimation is the difference in 30-day mortality rate estimates between the nontransferred sub-cohort and the combined cohort (percent in Nontransferred subcohort - percent in combined cohort). ‘Combined’ cohort includes all AMI patients with or without hospital transfers within an episode of care and ‘Non-transferred’ subcohort includes only patients without any hospital transfer.
This higher estimated 30-day mortality rate in the ‘non-transferred’ sub-cohort, compared to the overall ‘combined’ cohort, was consistent across all sex and age groups.
However, the overestimation was greater in women in the younger age groups, while in the older age groups, the overestimation was greater in men (Figure 3).
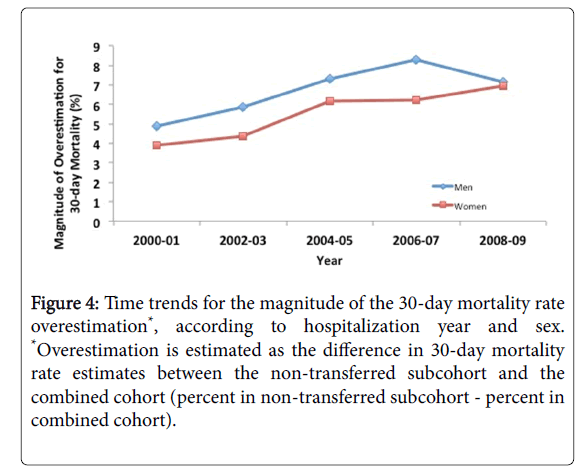
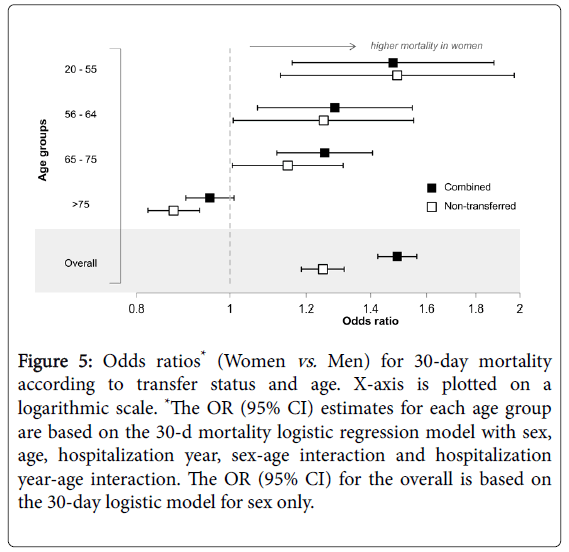
Over the study period, the magnitude of this overestimation increased for both men and women (Figure 4). In the most recent year, the 30-day mortality post AMI was overestimated by 7.2% in men and 6.9% in women. Furthermore, when estimating the 30-day mortality odds ratio for women vs. men, the sex gap was attenuated when the transferred patients were excluded, in contrast to when transferred patients were not excluded [OR (women vs. men)=1.25, (95% CI: 1.19, 1.31) in the ‘non-transferred’ sub-cohort compared to OR=1.49, (95% CI: 1.42, 1.56) in the ‘combined’ cohort]) (Figure 5).
Figure 4: Time trends for the magnitude of the 30-day mortality rate overestimation*, according to hospitalization year and sex. *Overestimation is estimated as the difference in 30-day mortality rate estimates between the non-transferred subcohort and the combined cohort (percent in non-transferred subcohort - percent in combined cohort).
Figure 5: Odds ratios* (Women vs. Men) for 30-day mortality according to transfer status and age. X-axis is plotted on a logarithmic scale. *The OR (95% CI) estimates for each age group are based on the 30-d mortality logistic regression model with sex, age, hospitalization year, sex-age interaction and hospitalization year-age interaction. The OR (95% CI) for the overall is based on the 30-day logistic model for sex only.
The estimates of age-specific odds ratio for 30-day mortality were consistently underestimated using the ‘non-transferred’ sub-cohort, as compared to the ‘combined cohort’, except for the 20-55 age group.
Transferred patients
In order to gain a better understanding of the observed overestimation of the 30-day mortality rates, and hence the underestimation of the sex gap in 30-day mortality, the characteristics of the transferred patients (i.e. excluded patients) were assessed.
As previously described in Table 1, transferred patients were more likely to be men, younger and less likely to have comorbid conditions.
As well, transferred patients had a lower 30-day mortality rate, as compared to non-transferred patients (3.9% vs. 19.8%, p<0.001), which is likely a reflection of their younger age and presence of fewer comorbid conditions.
This observed difference in mortality rates was present in all age groups (Table 3).
| Age group | 30-day mortality (%) post AMI | |||||
|---|---|---|---|---|---|---|
| Women | Men | |||||
| Non- transferred | Transferred | p-value | Non- transferred | Transferred | p-value | |
| 20-55 | 8.1 | 1.7 | <0.001 | 5.7 | 1.1 | <0.001 |
| 56-64 | 11.2 | 2.8 | <0.001 | 9.1 | 2 | <0.001 |
| 65-74 | 17 | 5.7 | <0.001 | 15.2 | 3.8 | <0.001 |
| ≥ 75 | 25.4 | 8 | <0.001 | 28 | 7.5 | <0.001 |
‘Non-transferred’ sub-cohort includes only patients without any hospital transfers; ‘Transferred’ sub-cohort includes only patients who were transferred from their index hospital to another hospital during their episode of care.
Table 3: Thirty-day Post AMI mortality rates, according to transfer status and sex.
Discussion
In this large, population-based study of AMI patients, we found that 40% of patients had at least one hospital transfer during their episode of care and the proportion of transferred patients increased over time for both men and women and across all age groups. Overall, transferred patients were younger, more likely to be male, less likely to have comorbid conditions and thus had lower 30-day mortality rates than the patients who were not transferred. Excluding the transfers from the analysis resulted in an overestimation of 30-day mortality post AMI, in both men and women, and across all age groups with a more pronounced bias observed among younger women, as compared to younger men, and older men, as compared to older women. Importantly, the magnitude of this overestimation has increased over time. Furthermore, the overall sex difference in 30-day mortality was underestimated in the cohort that excluded the transferred patients, erroneously implying a smaller sex gap than what would be observed in a cohort that included both transferred and non-transferred patients.
Several studies have examined the proportion of hospital transfers among AMI patients, their characteristics as well as the organizational structure and patterns of transfers [13]. Methodologically, excluding transferred patients in the analysis is an approach that is commonly used in outcomes research when linking hospitalization records is not feasible; however, very few studies have addressed the consequences of excluding this group of patients. Our study is the first comprehensive assessment of the magnitude of the resulting bias in 30-day post AMI mortality rates by sex, age when such exclusions are undertaken.
Our finding that a large proportion of AMI patients are transferred during their hospitalization is also consistent with prior studies in the United States. Based on the nationwide Medicare data, Iwashyna et al. found that 44% of all AMI patients admitted to non-revascularization hospitals were transferred to hospitals with revascularization capabilities [13]. Similarly, Roe et al. observed that among NSTEMI patients in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines) registry, 46% were transferred to tertiary care hospitals and that this proportion has increased over time [14]. The American College of Cardiology/ American Heart Association (AHA) guidelines provide a class I recommendation for early invasive management of STEMI as well as NSTEMI patients with high risk of mortality and recurrent ischemia [15,16]. This, coupled with the fact that majority of hospitals in Canada and the US do not have revascularization capabilities, it is expected that a large proportion of AMI patients would be transferred to tertiary care hospitals with a more specialized cardiac care.
Given the potentially large proportion of AMI patients who are transferred out to other hospitals during their episode of care, it is important to understand the impact of their inclusion/exclusion when assessing or comparing population-based patient outcomes, or hospital rankings, across multiple sites/studies. As highlighted in our findings, excluding transfers can result in an overestimation of 30-day post AMI mortality rates. It is important to note that the larger the proportion of transfers, the greater the magnitude of this bias will be. Our findings, as well as those in prior studies [14,17] have consistently shown that transferred patients have lower 30-day mortality rates and as such removing this group of patients, results in a cohort of patients with higher mortality. The reasons for the lower 30-day mortality rates among transferred patients are multifactorial. Transferred patients are more likely to have a lower cardiac risk profile, have fewer comorbidities, are younger and more likely to be men, which contribute to a lower risk for 30-day mortality post AMI.
Among younger adults, the bias was greater in women than in men, resulting in an overestimation of the sex gap in 30-day mortality rates. In contrast, among older adults, the bias was greater in men. The magnitude and direction of the bias for each age-sex stratum is not only a function of the proportion of transfers, but also on the difference in the 30-day mortality rates in the non-transferred and transferred patients in that stratum [i.e. bias=proportion of transfers x (30-day mortality rate of the non-transferred cohort 30-day mortality rate of the transferred cohort]. For instance, the larger bias observed among younger women seems to be driven by the particularly high mortality rates in the non-transferred cohort and not by the proportion of transfers which were similar to that observed among younger men. Furthermore, we observed that the overestimation of 30- day mortality is in fact increasing over time, which is most likely a reflection of the increasing trend in transferring AMI patients to hospitals with more advanced cardiac treatments.
Our finding of an underestimation of the sex gap in 30-day mortality is intriguing and highlights the caution required when comparing conclusions across studies with varying methods for handling transferred patients. For instance, a prior study on sex differences in 30-day mortality post AMI, based on the US National Registry of Myocardial infarction (NRMI), reported a narrowing of the mortality gap between men and women over the years. In this study, 41% of women and 48% of men were excluded due to limitations in establishing outcomes of transferred patients [2]. On the other hand, in a recent population based analysis of the sex gap in 30-day mortality post AMI, which did not exclude transferred patients, a persistent difference in mortality rates in women as compared to men was observed over a 10-year study period [18]. Based on our current findings, it is reasonable to speculate that the differences in the patient populations, in terms of exclusion of transferred patients, may have contributed to these inconsistent findings and the apparent closing of the sex gap in the NRMI registry.
Our study is not without its own limitations. First, detailed sociodemographic factors, including income and ethnicity were not available in our study and therefore we were not able to measure their impact on the observed transfer rates and post AMI mortality. Furthermore, we were not able to capture factors related to hospital characteristics such as revascularization capacity as well as rural vs. urban. We would expect that the transfer rates would be higher in the rural areas and as such the magnitude of the observed bias in 30-day AMI mortality estimates would be greater.
We were also unable to distinguish STEMI and NSTEMI. Given the current guidelines for the immediate transfer of STEMI patients to a PCI-capable hospital to undergo primary PCI, we speculate that a larger proportion of transferred patients are those with STEMI presentation admitted to hospitals without revascularization capabilities rather than NSTEMI patients. This would be in line with our current finding of lower 30-day mortality among transferred patients, as STEMI patients are shown to have lower short-term mortality rates than NSTEMI patients [19].
The strength of our study lies in its 10-year population-based cohort with access to outcomes information on both transferred and nontransferred AMI patients. This provided a unique opportunity to identify and quantify the impact of the exclusion of transferred patients on commonly reported 30-day mortality outcomes post AMI.
Summary and Conclusion
The observed difference in the characteristics and outcomes of transferred and non-transferred AMI patients has implications for outcomes research, especially in population-based studies, where the focus is on all patients admitted with AMI. When the proportion of transferred AMI patients is high, failure to include their outcomes in the evaluation will likely result in an overestimation of the 30-day mortality rate. This finding also highlights the need for caution when comparing conclusions across studies with varying methods for handling transferred patients.
Acknowledgments
The BC’s Ministry of Health, and Vital Statistics Agency approved access and use of the data facilitated by population data BC. We thank the Population Data BC for facilitating this process. We also thank the BC Centre for Improved Cardiovascular Health for providing support for this study.
Disclaimer: Inferences, opinions, and conclusions drawn in this study are those of the authors, and do not reflect the opinions or policies of the Data Steward(s).
Disclosures: None
Source of Funding: Canadian Institutes of Health Research (CIHR)
References
- Kosseim M, Mayo NE, Scott S, Hanley JA, Brophy J, et al. (2006) Ranking hospitals according to acute myocardial infarction mortality: should transfers be included? Med care 44: 664-670.
- Vaccarino V, Parsons L, Peterson ED, Rogers WJ, Kiefe CI et al. (2009) Sex differences in mortality after acute myocardial infarction: changes from 1994 to 2006. Arch Intern Med 169: 1767-1774.
- Peterson ED, Roe MT, Chen AY, Fonarow GC, Lytle BL, et al. (2010) The NCDR ACTION Registry-GWTG: transforming contemporary acute myocardial infarction clinical care. Heart 96:1798-1802.
- Patel AB, Quan H, Faris P, Knudtson ML, Traboulsi M, et al. (2011) Temporal associations of early patient transfers and mortality with the implementation of a regional myocardial infarction care model. Can j cardiol 27: 731-738.
- Canadian Institute of Health Information (2013) Discharge Abstract Database (Hospital Separations).
- BC Vital Statistics Agency (2013) BC Vital Statistics Deaths. Population Data BC
- McCormick N, Lacaille D, Bhole V, Zubieta JA (2014) Validity of myocardial infarction diagnoses in administrative databases: a systematic review. PloS one 9: e92286.
- Levy AR, Tamblyn RM, Fitchett D, McLeod PJ, Hanley JA (1999) Coding accuracy of hospital discharge data for elderly survivors of myocardial infarction. Can J cardiology 15: 1277-1282.
- Austin PC, Daly PA, Tu JV (2002) A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am heart J 144: 290-296.
- Humphries KH, Rankin JM, Carere RG, Buller CE, Kiely FM et al. (2000) Co-morbidity data in outcomes research: are clinical data derived from administrative databases a reliable alternative to chart review? J Clin Epidemiol 53: 343-549.
- Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, et al. (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10Â administrative data. Med care 43:1130-1139.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J chron dis 40: 373-383.
- Iwashyna TJ, Kahn JM, Hayward RA, Nallamothu BK (2010) Interhospital transfers among Medicare beneficiaries admitted for acute myocardial infarction at nonrevascularization hospitals. Circ Cardiovasc Qual Outcomes 3: 468-475.
- Roe MT, Chen AY, Delong ER, Boden WE, Calvin JE, et al. (2008) Patterns of transfer for patients with non-ST-segment elevation acute coronary syndrome from community to tertiary care hospitals. Am heart J 156: 185-192.
- O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, et al. (2013) 2013 ACCF/AHA guideline for the management of ST-Â-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 61: 485-510.
- Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, et al. (2014) 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 64: 2645-2687.
- Westfall JM, Kiefe CI, Weissman NW, Goudie A, Centor RM, et al. (2008) Does interhospital transfer improve outcome of acute myocardial infarction? A propensity score analysis from the Cardiovascular Cooperative Project. BMC Cardiovasc Disord 8: 22.
- Izadnegahdar M, Singer J, Lee MK, Gao M, Thompson CR, et al. (2014) Do younger women fare worse? Sex differences in acute myocardial infarction hospitalization and early mortality rates over ten years. J women's health 23: 10-17.
- McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, et al. (2011) Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Medicine 124: 40-47.
Citation: Izadnegahdar M, Lee MK, Gao M, Pak M, Humphries KH (2016) Biased Estimates for 30-day Mortality Rates Post Myocardial Infarction-Impact of Inter-Hospital Transfers. Epidemiology (Sunnyvale) 6:271. DOI: 10.4172/2161-1165.1000271
Copyright: © 2016 Humphries KH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 12024
- [From(publication date): 10-2016 - Jul 12, 2025]
- Breakdown by view type
- HTML page views: 11080
- PDF downloads: 944