Case Report Open Access
Benign Metastasizing Leiomyoma
Beatriz Sastre* and Emilio Valbuena
Department of Radiology, Hospital General Universitario de Guadalajara, Guadalajara, Spain
- *Corresponding Author:
- Beatriz Sastre
Department of Radiology
Hospital General Universitario de Guadalajara
Guadalajara, Spain
Tel: 0034666381055
E-mail: beasastre@hotmail.com
Received Date: April 24, 2017; Accepted Date: May 11, 2017; Published Date: May 16, 2017
Citation: Sastre B, Valbuena E (2017) Benign Metastasizing Leiomyoma. OMICS J Radiol S2:001. doi: 10.4172/2167-7964.S2-001
Copyright: © 2017 Sastre B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Benign Metastasizing Leiomyoma (BML) is a rare disease characterized by proliferation of uterine smooth muscle tissue in extrauterine locations. The lungs are the most affected organ. The patient type is a female in the pre/ perimenopausal age that has been gone through a myomectomy several years before when during a routine chest roentgenogram multiple pulmonary shadows are noticed. We report a case of a 54-years-old female who presented a chest X-ray with multiple bilateral pulmonary nodules during a health checkup. She had no symptomatology and personal history just included uterine leiomyomectomy of the uterus 16 years before. A contrast-enhanced CT confirmed the nodules within a normal interstitium. A biopsy was performed and histopathological examination showed characteristics of smooth muscle cell differentiation giving the diagnosis of BML. The management strategy decided was just radiological follow-up and she is stable ever since.
Keywords
Benign Metastasizing Leiomyoma (BML); Lung nodules; Leiomyoma
Case Presentation
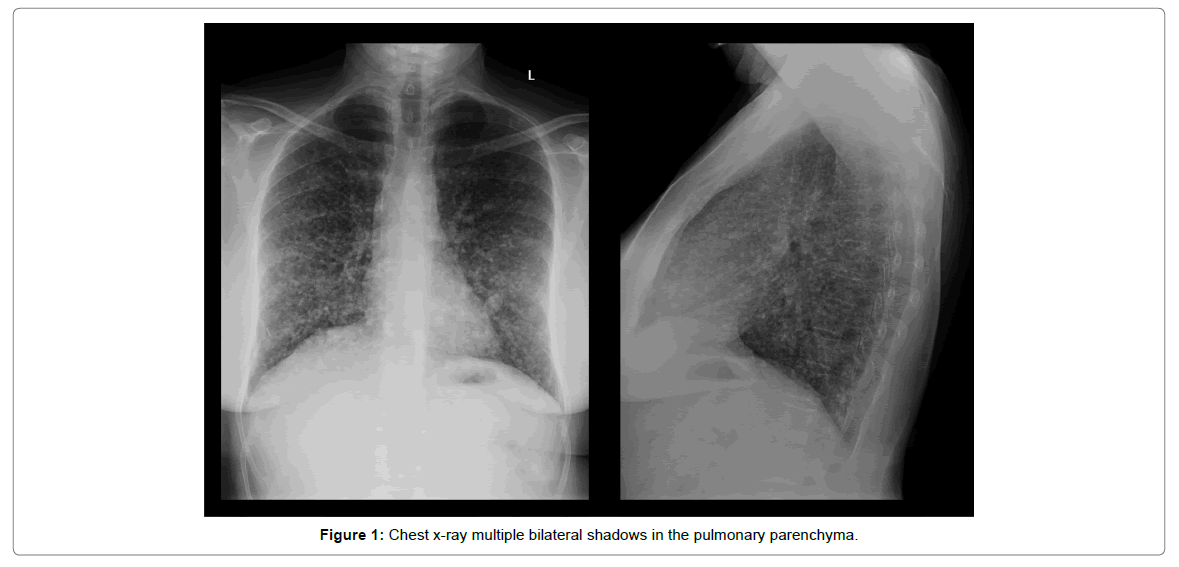
A 54-years-old perimenopausal female was referred to the pneumology outpatient clinic for further evaluation of incidental lung nodules. Chest X-ray showed multiple bilateral shadows in the pulmonary parenchyma (Figure 1). Asked about any clinical symptom, she just referred a light dyspnea in high exercise situations. She had no personal history of pulmonary disease, being all the respiratory tests within the normal ranges. Surgical intervention of a myomectomy was carried out 16 years earlier.
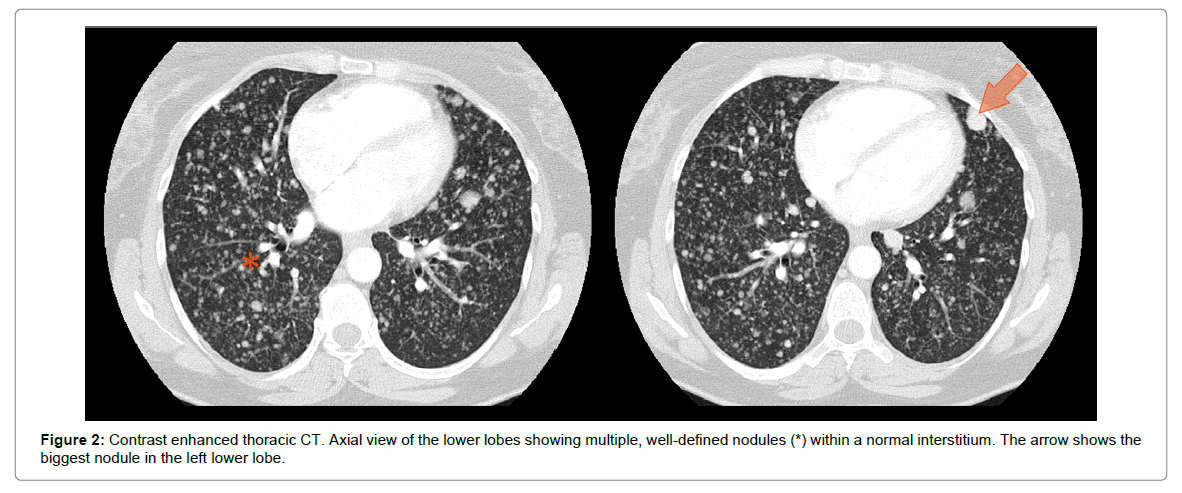
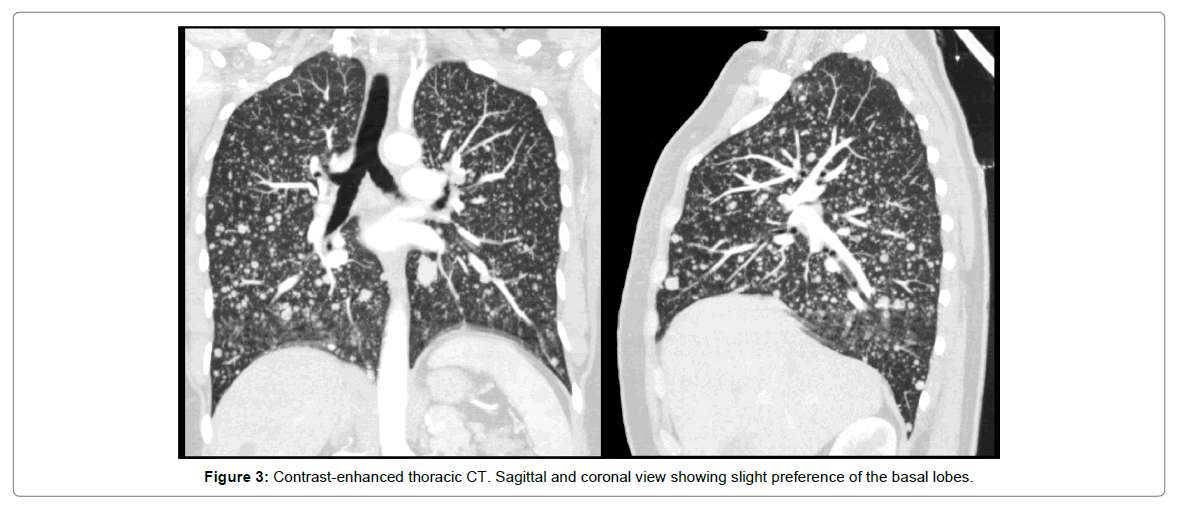
A contrast-enhanced Computed Tomography (CT) confirmed the presence of multiple, well defined, pulmonary nodules (Figure 2). They presented a bilateral disposition with a slight preference for basal regions (Figure 3). They didn’t enhance after contrast medium. The size was variable, but all of them were lower than 2 c, the biggest one was located in the left lower lobe (Figure 2). The rest of the interstitium was normal. No lymphadenopathies or other findings were noticed.
A PET scan revealed multiple nodules with an intermediate SUV uptake; the maximum was 3.0, without any other alteration.
In the multidisciplinary committee, it was decided to get a biopsy by means of Video-Assisted Thoracoscopic Surgery (VATS).
Histopathological examination of the lesion showed pulmonary nodules with smooth muscle cells differentiation, without neither atypical nor mitotic activity. Inmunohistochemical analysis was positive for actine. The morphological and immunohistochemical pattern discarded the diagnosis of lymphangioleiomyomatosis.
With all the radiological, clinical and histopathological findings, the diagnosis of BML was confirmed.
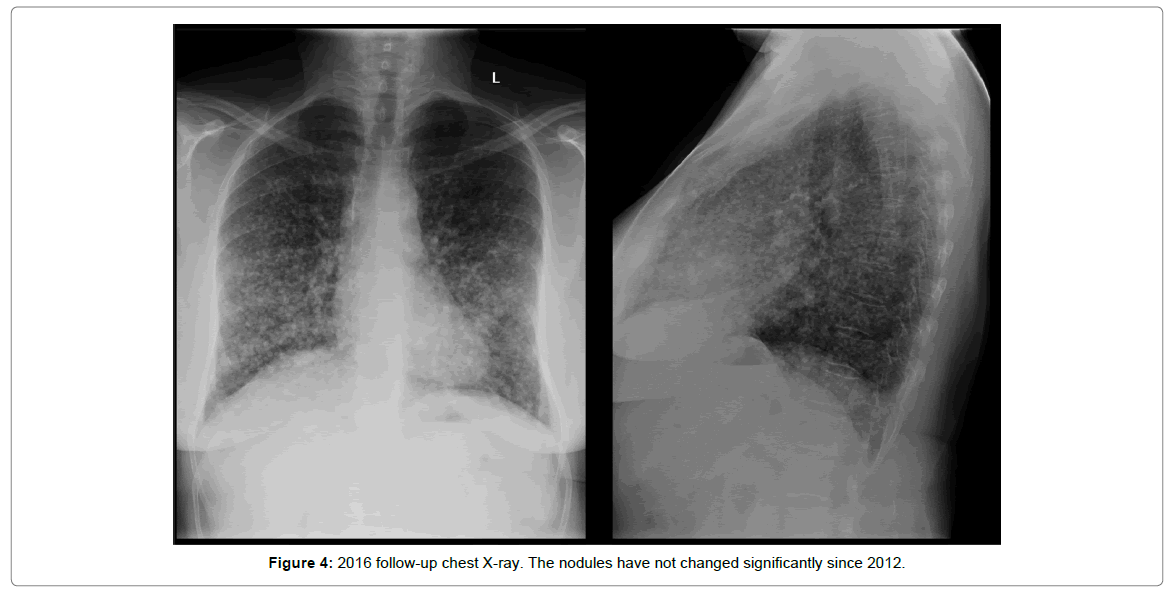
Giving, she was in a perimenopausal state; a “wait-and-see” treatment strategy with radiology surveillance was decided. There has been 5 years and the patient is still asymptomatic without radiological signs of pulmonary progression (Figure 4).
Discussion
The uterine myomas are the most common gynecological neoplasm in childbearing age women. They are considered to be benign, as the result of proliferation of uterine smooth muscle tissue. However, there have been described very infrequent situations in which the tumor presents a distant progression of smooth muscle cell to other organs. There are different types of growing pattern including Benign Metastasizing Leiomyoma (BML), intravascular leiomyomatosis and disseminated peritoneal leiomyomatosis [1]. The most afflicted organs are the lungs [2], but there have been documented extrapulmonary involvement in heart, spine, bone, skull base, omentum and mesentery, lymph nodes and deep soft tissue.
Benign metastasizing leiomyoma of the lung was first described in 1939 by Steiner [3], who reported a 36-years-old female with a history of benign uterine leiomyomas with pulmonary metastases that suffered cor pulmonale. Nowadays, it is still a very rare condition with only less than 150 cases published in the literature [4]. The pathogenesis is still controversial and several hypotheses had been proposed including in situ proliferation, low-grade uterine leiomyosarcoma and, even, the possibility of surgically induced displacement [5].
Martin [6] classified leiomyomatous lung lesions into three categories: benign metastasizing lesions in women, metastasic leiomyoma in men and children, and multiple pulmonary fibroleiomyomatous hamartoma.
BML has been described in women of reproductive age, more frequently during the premenopausal period. In most cases, the patients are asymptomatic, but they can also exhibit cough, dyspnea and, in worst cases, rapidly decreased pulmonary function and death [7].
All the patients have personal history of leiomyomas; some of them have gone through a myomectomy several years before the diagnosis. It is described in the literature that the mean years between the surgery and the pulmonary manifestation is 15 years [8].
The diagnosis is usually incidental; during a routine chest roentgenogram. In the chest X-ray multiple, bilateral shadows are displayed in the pulmonary parenchyma. The Computed Tomography (CT) confirms the presence of multiple, well-circumscribed lesions, that are usually bilateral. Cases with just a solitary lesion have also been reported, in the 13% in radiological evaluation by Horstmann et al. [9]. The nodules range a size between milimeters and few centimeters and the rest of the interstitium is normal. The lesions do not enhance with intravenous contrast medium. A military pattern or cystic degeneration is very rare but can be seen [10]. There are no lymphadenopaties associated. BML presents a characteristic endobronchial and pleural sparing. The PET-CT is recently being used to make the differential diagnosis. The nodules show any significant FDG uptake.
The histopathological study confirms the diagnosis. A VATS biopsy must be made and not a Fine-Needle Aspiration (FNA), in order to have enough tissue sample [2]. The macroscopically examination shows a solid, well delimited lesion composed of spindle-shaped cells with smooth muscle differentiation. The BML histological features are of a benign nature: low mitotic rate, absence of neither necrosis nor cytological atypia. Inmunohistochemical study show actin and desmin markers positive, in relation with smooth muscle origin. There has been reported also the presence of estrogen and progesterone receptors, that relates it to female genital tract, and is related to a good prognoses. Also, low Ki-67 is seen, that confirms the low proliferative state.
Currently, there is no established treatment for BML. Hormonal manipulation medically, through administration of progesterone and aromatase inhibitors, or surgically, with hysterectomy and bilateral oophorectomy, have been reported with varied results. If the patient is asymptomatic and in the perimenopausal or postmenopausal state, a “wait-and-see” strategy should be enough [11], just if an increase of size of pulmonary lesions is noticed surgical resection can be proposed, but is still very controversial. Therefore, an individual treatment approach should be considered in each patient depending on its hormonal status and radiological features.
Conclusion
Although a rare disease, benign metastasizing leiomyoma of the lung should be considered when multiple bilateral pulmonary nodules are seen in an asymptomatic-perimenopausal female with history of leiomyoma’s.
References
- Rivera JA, Christopoulos S, Small D, Trifiro M (2004) Hormonal manipulation of benign metastasizing leiomyomas: report of two cases and review of the literature. J Clin Endocrinol Metab 89: 3183-3188.
- Chen S, Zhang Y, Zhang J, Hu H, Cheng Y, et al. (2013) Pulmonary benign metastasizing leiomyoma from uterine leiomyoma. World J Surg Oncol 11: 163.
- Steiner PE (1939) Metastasizing fibroleiomyoma of the uterus: report of a case and review of the literature. Am J Pathol 15: 89-110.
- Lewis EI, Chason RJ, DeCherney AH, Armstrong A, Elkas J, et al. (2013) Novel hormone treatment of benign metastasizing leiomyoma: an analysis of five cases and literature review. Fertil Steril 99: 2017-2024.
- Burkhadt A, Otto HF, Kaukel E (1981) Multiple pulmonary (hamartomatous?) leiomyomas. Virchows Archiv 394: 133-141.
- Martin E (1983) Leiomyomatous lung lesions: a proposed classification. AJR 141: 269-272.
- Säynäjäkangas O, Maiche AG, Liakka KA (2004) Multiple progressive pulmonary leiomyomatous metastases treated with tamoxifen: a case report with a review of the literature. Acta Oncol 43: 113-114.
- Kayser K, Zink S, Schneider T, Dienemann H, André S, et al. (2000) Benign metastasizing leiomyoma of the uterus: Documentation of clinical, immunohistochemical and lectin-histochemical data of ten cases. Virchows Archiv 437: 284-292.
- Horstmann JP, Pietra GG, Harman JA, Cole NG, Grinspan S (1977) Spontaneous regression of pulmonary leiomyomas during pregnancy. Cancer 39: 314-322.
- Osadchy A, Zehavi T, Zissin R (2014) Pulmonary benign metastasising leiomyomas presenting as fluid-containing masses on CT in a patient with two unrelated malignancies. Br J Radiol 78: 639-641.
- Hoetzenecker K, Ankersmit HJ, Aigner C, Lichtenauer M, Kreuzer S, et al. (2009) Consequences of a wait-and-see strategy for benign metastasizing leiomyomatosis of the lung. Ann Thorac Surg 87: 613-614.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 3617
- [From(publication date):
specialissue-2017 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 2771
- PDF downloads : 846