Barriers to Palliative Care Uptake in Culturally and Linguistically Diverse Populations: A Systematic Review
Received: 28-Jun-2023 / Manuscript No. jpcm-23-105571 / Editor assigned: 30-Jun-2023 / PreQC No. jpcm-23-105571(PQ) / Reviewed: 14-Jul-2023 / QC No. jpcm-23-105571 / Revised: 20-Jul-2023 / Manuscript No. jpcm-23-105571(R) / Accepted Date: 26-Jul-2023 / Published Date: 27-Jul-2023 DOI: 10.4172/2165-7386.1000542
Abstract
Background and aim: Palliative care is essential for patients with life-limiting illnesses, as it enhances survival and quality of life. However, culturally and linguistically diverse individuals often struggle to access timely palliative care. This study investigates barriers to timely palliative care uptake in these populations.
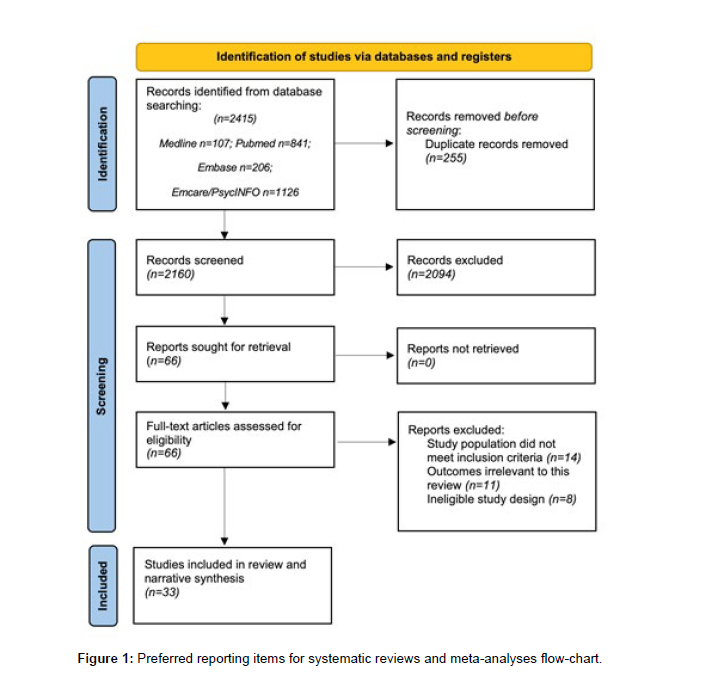
Methodology: A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Primary studies of different design exploring barriers to palliative care uptake in culturally and linguistically diverse populations were included, and data were analysed using narrative synthesis. Studies were appraised based on methodological quality and quality of reporting using the assessment criteria framework proposed by Kmet, Lee and Cook.
Data sources: PubMed, Medline, Embase, PsycINFO, EBMR and Emcare (February 2022).
Results: Of 2415 identified articles, 33 studies (30 qualitative, three quantitative) were included. Patients from diverse backgrounds reported barriers in four domains: negative attitudes towards palliative care, limited awareness of palliative care, poor understanding of their disease, and poor communication and collaboration with healthcare professionals (23 studies). Healthcare professionals reported barriers in four domains: lack of cultural understanding and awareness, lack of palliative care-specific training, emotions related to palliative care, and healthcare system/ structural barriers (19 studies).
Conclusion: Barriers to palliative care delivery in culturally and linguistically diverse cohorts mainly involve the themes of poor education and communication between patients and healthcare professionals. Developing and evaluating educational interventions targeting patients, caregivers, and healthcare professionals may improve palliative care uptake in these populations.
Keywords
Palliative care; Barriers; Transients and migrants; Culturally and linguistically diverse
What is already known about the topic?
• Early palliative care enhances survival, quality of life, and outcomes for patients and their caregivers with chronic, life-limiting illness.
• Poor palliative care uptake persists among various population groups, with limited systematic insight on culturally and linguistically diverse populations.
What this paper adds?
• This study reveals pertinent barriers experienced and endorsed by patients and healthcare professionals. Patient-perceived barriers include negative attitudes towards palliative care, limited awareness of palliative care, a poor understanding of their disease, poor communication between patients and healthcare professionals.
• Identified healthcare professional barriers span four domains: a lack of cultural understanding and awareness, a lack of palliative care-specific training, emotions related to palliative care, and healthcare system/structural barriers.
• To our knowledge, this represents the first systematic review that consolidates global migrant population data on palliative care barriers from both healthcare providers’ and patients’ perspectives.
Prior research on perceived barriers among migrants has primarily focussed on specific population groups.
Implications for practice, theory, or policy
• The majority of barriers identified in this study primarily stem from inadequate education, misinformation, or a complete absence of education, and may therefore be effectively addressed through appropriate educational interventions.
• Future studies should delineate optimal educational intervention delivery and emphasise systematic clinician training in palliative care principles to encourage early uptake.
Introduction
Palliative care is a relatively neoteric medical speciality that serves to holistically manage the needs of patients and their families or caregivers in the context of a life-limiting illness [1]. The World Health Organisation defines palliative care as ‘an approach that improves the quality of life of patients and their families who are facing problems associated with life-threatening illness’, thus ‘it prevents and relieves suffering through early identification, correct assessment and treatment of pain and other problems, physical, psychosocial and spiritual’ [2,3]. It has become a fundamental aspect of best medical practice given the world’s ageing population and increasing incidence rates of chronic diseases, concomitantly with improvements in treatments for these diseases [4]. The latter has meant there are more people living with chronic conditions who would benefit from palliative care support to improve their quality of life. Consequent to this, the relevance and role of palliative care is increasingly well-recognised. Evidence supports the concurrent and integrated provision of palliative care (including both specialist and generalised palliative care) into the traditional medical model of care for many chronic illnesses. Several randomised control trials have demonstrated improved patient and caregiver outcomes in terms of survival, quality of life and carer preparedness for the caregiving role when early palliative care is introduced [5-8].
International migration is increasing worldwide, and as of 2017, the number of international migrants was estimated to be 258 million comprising 3.4% of the global population - compared to 173 million in 2010 [9]. Accordingly, Western healthcare systems are serving an increasingly diverse population. While many individuals choose to migrate out of choice, migration is also necessitated by war, poverty, and persecution [10]. This population has the right to receive highquality accessible healthcare, including the services offered by palliative care.
The culturally and linguistically diverse population is a marginalized group that is often underserved and underrepresented in palliative care uptake. Unfortunately, this results in late palliative care involvement, when patients are already suffering from severe symptom burden [11,12]. Despite the significant proportion of the community constituted by migrant patients, the barriers to palliative care uptake for this group remain ill-defined. Previous systematic reviews have explored the palliative care experiences of migrants, but they were limited by national contexts and limited inclusion of migrant groups [12-14]. In order to support the development and implementation of models of palliative care services for the culturally and linguistically diverse population, it is crucial to delineate the breadth of barriers related to them. Therefore, this systematic review was conducted to systematically summarise and present the available published data on barriers to the uptake of palliative care among the culturally and linguistically diverse population.
Methods
This systematic review was reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15].
Design & search terms
We searched the peer-reviewed literature from inception to February 2022 in six databases: PubMed, Medline, Embase, PsycINFO, EBMR and Emcare. The following search terms were used for the identification of eligible studies:
((((((neoplasm*) OR (cancer*)) OR (chronic disease*)) OR (terminal disease*)) AND ((((((((barrier*) OR (obstacle*)) OR (challenge*)) OR (perspective*)) OR (perception*)) OR (facilitate*)) OR (enable*)) OR (experience*))) AND (((((palliative care) OR (hospice care)) OR (end of life care)) OR (terminal care)) OR (supportive care))) AND ((((((((migrant*) OR (transient*)) OR (displaced person*)) OR (CALD)) OR (culturally-and-linguistically-diverse)) OR (refugee*)) OR (asylum seeker*)) OR (non-English speaking)).
Inclusion & exclusion criteria
Inclusion criteria included primary studies investigating any outcome related to barriers of palliative care uptake, including qualitative studies, clinical trials, or observational studies. All study participants were adults (over 18 years). All patient participants had a diagnosis of terminal, chronic or life-limiting illnesses. All healthcare professionals were involved in the care of culturally and linguistically diverse patients. Studies were only included if the patient or caregiver/ family member participants comprised over 50% of the study cohort. In accordance with the systematic review’s objectives, the search was restricted to peer-reviewed published studies, and thus excluded literature such as case reports, case studies and editorial letters. Systematic reviews and other review papers were not included in the results of this review. No language restrictions were applied. Studies were independently selected by two reviewers (SH and MA) through a process of screening titles and abstracts, followed by a comprehensive full-text assessment. Disagreements were resolved by discussion. (Table 1)
| Component | Criteria |
|---|---|
| Study Population | Inclusion criteria
|
| Study design | Inclusion criteria
|
| Outcomes | Any outcome related to barriers of palliative care uptake was eligible |
| Language | No language restrictions |
Table 1: Inclusion and exclusion criteria.
Data extraction and assessment of methodological quality
Customized excel spreadsheets were created for collecting data from all selected studies. Data encapsulated author, year, country, study aim, design, data collection methods, population, participants’ characteristics, and outcomes related to barriers to palliative care uptake. Data were retrieved independently by two reviewers (SH and MA). The quality of included studies was assessed and appraised independently by two authors (SH and MA) using the qualitative and quantitative assessment criteria framework proposed by Kmet, Lee and Cook [16]. This tool was chosen as it is applicable to studies of different design, and it robustly assesses all components of the primary study, including the research question, study design, sampling strategy and data analysis. Based on the total score, studies were classified as ‘low’ quality (0-12 for quantitative and qualitative studies), ‘moderate’ quality (13-16 for quantitative and qualitative studies) or ‘high’ quality (17-20 for quantitative and qualitative studies).
Synthesis method
A narrative synthesis was used to amalgamate concepts and data from a wide range of differing methodologies, as our review contains both quantitative and qualitative studies. We followed the guide detailed by Popay et al. to systematize the process of analysis, especially as other methods, such as a meta-analysis were inappropriate for our paper due to the degree of heterogeneity in the included studies [17]. The steps outlined by Popay et al. included (1) preliminary analysis, (2) exploration of relationships, and (3) assessment of the robustness of synthesis.
Results
The initial literature search identified 2415 papers. After removing 255 duplicates, a further 2094 articles were excluded following title and abstract screening. The remaining 66 articles were retrieved, and fulltext screening was performed. A total of 33 articles met our inclusion criteria and were retained for analysis (Figure 1).
The barriers to palliative care were categorised into 2 overarching groups: 1) barriers related to patients and their carers, and 2) barriers related to healthcare practitioners. Table 2 summarises the characteristics of each of the included studies.
| Study no. | Author/Year/ Country | Aim | Design | Participants | Data collection method | Outcomes related to barriers of Palliative Care uptake |
|---|---|---|---|---|---|---|
| 1 | Alananzeh I, Halcomb E, et al., 2020, Australia | To investigate the models of support preferred by Arab Australians living with chronic conditions and to identify potential barriers to the uptake of support programs for chronic conditions | Quantitative - Cross-sectional study | 251 Arab Australian patients with at least one chronic condition (Hypertension 53.8%, Arthritis 53.8%, Diabetes 39.8%, Respiratory conditions 13.9%) | Survey | 22% of respondents did not find palliative care useful at all. |
| 2 | Ayash et al., 2017, USA | To investigate the unmet socio-economic needs among Arab American breast cancer patients compared with other immigrant and migrant patients. | Quantitative - Comparative study of nested cohort | 309 multiethnic patients (Arabs n=36, Latinos n=145, Caribbean immigrants of African descent n=128) with breast cancer | Survey | This study found significantly poor health literacy among respondents, as well as language and financial barriers impeding uptake of palliative care. More than two-thirds of Arab patients were unaware of their cancer stage. |
| 3 | Bellamy et al., 2013, New Zealand | To investigate the unmet socio-economic needs among Arab American breast cancer patients compared with other immigrant and migrant patients. | Qualitative | 80 Health Professionals working in specialist (comprising hospice and specialist palliative care teams, n=26) and generalist palliative care settings (comprising GP surgeries, hospital-based teams and residential aged care facilities, n=54) | Focus-groups and joint interviews | A lack of palliative care education for patients informed beliefs that palliative care is unwelcoming and contrary to patients’ cultural beliefs. Health professionals were reluctant to provide palliative care due to anxieties related to the constraints posed by the physical environment in accommodating extended families. |
| 4 | Broom et al., 2019, Australia | To improve the experiences of people from diverse cultural backgrounds and how professionals in cancer care experience their encounters with migrant cancer patients with a focus on how they work with cultural diversity in their everyday practice | Qualitative | 57 Health Professionals working with migrants in cancer care including multicultural community workers (n=8), allied health workers (n=26), doctors (n=13) and nurses (n=10) | Focus groups | Culture was experienced differently in each patient, and treating a patient as a unique person was seen as unrealistic given resource and institutional constraints. |
| 5 | Butow et al., 2012, Australia | To understand: interpreters' perceptions of their role; challenges faced working in the adult oncology setting; training and support needs. | Qualitative | 30 interpreters (Greek n=7, Chinese n=11, Arabic n=12) working in cancer-focussed settings | Focus groups | Cancer consultations are emotionally draining and interpreters may be reluctant to provide their service in these settings |
| 6 | Chiang et al., 2015, Australia | To understand the experience of a large minority group of Mandarin-speaking cancer patients after diagnosis and treatment of their cancer in Australia with a view to delineate if cultural or linguistic factors affected the quality of care provided | Qualitative | 22 Mandarin-speaking cancer patients (Breast cancer n=7, gastric cancer n=3, prostate cancer n=2, lung cancer n=2) | Semi-structured interviews | Stigma attached to the illness of cancer and palliative care in Chinese culture. Respondents did not understand that curative treatment was not always available. Language barriers existed between Chinese patients and health professionals which limited patients’ ability to advocate for themselves. |
| 7 | De Graaf et al., 2010, Netherlands | To elicit the perspectives of palliative care from immigrant families with a Turkish or Moroccan background. | Qualitative | 33 cases of terminal cancer involving 83 individuals interviewed (Patients n=6, Caregivers n=30, Health Professionals n=47). Patients and their caregivers were of Turkish or Moroccan background, care providers were of Dutch background. | Exploratory interviews | Palliative care was seen as shameful with many families finding it difficult to hand over care to professionals to avoid gossip in the community. Religious beliefs also proved barriers to palliative care, and pain relief was refused as patients believed dying should occur with a clear mind to face God. |
| 8 | De Graaf et al., 2010, Netherlands | To explore how communication and decision-making in Pall care among Turkish and Moroccan patients is influenced by different styles of care management. | Qualitative | 33 cases of terminal cancer involving 83 individuals interviewed (Patients n=6, Caregivers n=30, Health Professionals n=47). Patients and their caregivers were of Turkish or Moroccan background, care providers were of Dutch background. | Exploratory interviews | There are conflicting views on the role of the ‘care management group’: Dutch care providers see the patient as their primary discussion partner, while in Turkish and Moroccan families, relatives play a major part in the communication and decision-making. |
| 9 | De Graaf et al., 2010, Netherlands | To gain insight into the factors that influence communication between health professionals and Turkish and Moroccan immigrants in the palliative phase of cancer | Qualitative | 33 cases of terminal cancer involving 83 individuals interviewed (Patients n=6, Caregivers n=30, Health Professionals n=47). Patients and their caregivers were of Turkish or Moroccan background, care providers were of Dutch background. | Semi-structured interviews | There is miscommunication regarding palliative care due to differing cultural backgrounds between care providers and patients. The multilingual communication triangle of patient - family - care provider often also complicates the bridging of differences in care perceptions. |
| 10 | Dhingra et al., 2020, USA | To describe attitudes and beliefs concerning advanced care planning in older, non-English-speaking Chinese Americans in a medically underserved urban region | Qualitative | 179 Chinese American older adults (mean age 68.2 years) | Exploratory interviews | Cultural beliefs impeded palliative care discussions: 1/3rd of participants believed that talking about death in the presence of a dying person could accelerate death, and 13.1% of participants believed that talking about death can bring bad luck. |
| 11 | Dorji et al., 2021, Canada | To explore how Asian Buddhists, exposed to Western cultures, perceive death and dying with dignity, and examine their preferences for end-of-life care. | Qualitative | 15 Asian Buddhists | Exploratory interviews | A minority of participants (3/15) believed that dying with dignity should not involve medical intervention, in contrast to Western surveys where euthanasia and physician-assisted suicide are often considered the way to die with dignity. |
| 12 | Frey et al., 2013, New Zealand | To identify challenges to the use of hospice services for Māori, Pacific and Asian patients within the context of one district health board. | Qualitative | 52 participants (Māori/Pacific/Asian cancer patients and family n=37, health professionals n=15) | Semi-structured interviews | Lack of familiarity with the role of hospice services or the services available. Misperceptions of palliative care resulted in delayed uptake: hospice and palliative care was perceived as a place to die. Language barriers and cultural presumptions held by health professionals impeded palliative care uptake. |
| 13 | Green et al., 2018, Australia | To elicit the experiences of palliative care health professionals when providing care for patients from Culturally and Linguistically Diverse backgrounds which differ from mainstream Australian language and culture. | Qualitative | 28 Palliative Care staff | Focus groups | Lack of awareness of cultural norms around dealing with death to provide a good death experience. Stigma associated with the term palliative care and therefore avoidance of using it in practice. Patients wished to avoid pain medication equating “morphine with death”. Language barriers and families disliked using interpreters due to confidentiality issues. |
| 14 | Green et al., 2019, Australia | To understand the clinical and psychosocial journey of Culturally and Linguistically Diverse palliative care patients | Quantitative | 100 deceased patients from Culturally and Linguistically Diverse backgrounds (Chinese 20%, Greek 14%, Italian 14%, Macedonian 10%) | Data mining of medical records | Belief that opiates and sedatives were shortening patients’ life. Poor understanding of palliative care and the end-of-life phase among caregivers. |
| 15 | Guo et al., 2021, Jordan | To identify the needs and experiences of adult refugees in Jordan with advanced cancer and informal caregivers. | Qualitative | 29 refugees (Patients n=22, Caregivers n=7) from Syria n=14, Iraq n=4, Libya n=5, Palestine n=4, Yemen n=2 | Semi-structured interviews | Participants felt that doctors were working outside their scope when attempting to provide psychosocial-spiritual support. Frustration with health professionals as patients felt they did not discuss medical issues with them creating uncertainty. Expensive treatment associated with palliative care was a barrier to palliative care uptake. |
| 16 | Kirby et al., 2017, Australia | To explore the experiences and perspectives of professional interpreters in supporting the transition of Culturally and Linguistically Diverse patients to specialist palliative care | Qualitative | 20 professional interpreters (Vietnamese n=4, Mandarin n=3, Greek n=3, Bosnian n=2) working in oncology and palliative care settings in metropolitan hospitals | Semi-structured interviews | Challenges of translating meaning of 'palliative care', communicating and expressing sensitivity while remaining professional. Interpreters had to handle their own emotional burden while discussing sensitive end-of-life matters. |
| 17 | Lim et al., 2019, Australia | To explore the challenges and unmet needs experienced by the Australian Chinese community affected by cancer, to understand the contexts that hindered optimal care for this community | Qualitative | 62 adult Mandarin (n=37) and Cantonese-speaking (n=25) participants (Cancer survivors n=34, Carer n=28) | Focus groups | Unmet information and support needs for cancer patients. Patients were health illiterate (65% of survivors, 78% of participants) and held negative cultural attitudes towards cancer and its therapies. Language barriers. |
| 18 | Lin et al., 2019, Taiwan | To explore the decision-making processes and drivers of receiving palliative care in advance care planning discussions from perspectives of advanced care patients, families and healthcare professionals | Qualitative | 45 participants, including advanced care patients who were likely to be in last 12 months of life (n=15) family members (n=15) and healthcare professionals (n=15) from inpatient oncology and hospice units Advanced care patients were most diagnosed with liver cancer n=3, lung cancer n=3, colon cancer n=2, and oesophageal cancer n=2 |
Semi-structured interviews | Patients’ did not understand the term palliative care. Clinicians found it challenging to talk openly with patients about cancer progression due to lack of trusting clinician-patient relationship. |
| 19 | McGrath et al., 2021, Australia | To examine the needs and experiences of families from non-English speaking backgrounds | Qualitative | 33 caregivers of patients experiencing terminal care, from Indian n=4, Filipino n=5, Chinese n=7, and Italian n=10 backgrounds | Focus groups | Poor awareness of palliative care and hospice services. Patients from cultural groups indicated that talking about death or dying was a cultural taboo. There was also a language barrier. |
| 20 | Morris et al., 2005, USA | To improve understanding of how to approach discussions between language-discordant patients and clinicians about terminal or life-threatening illness | Qualitative | 68 professional medical interpreters (Asian n=32, North American n=18, South/Central American n=11, European n=5, African n=2) | Focus groups | Health professionals had poor understanding of cultural rituals surrounding death. There was poor coordination with other providers, and interpreters struggled to provide education to patients about death and dying. |
| 21 | Nielsen et al., 2015, Canada | To examine the meanings of home and negotiations of care between Chinese immigrants receiving palliative home care, their family caregivers, and home healthcare practitioners | Qualitative | 20 participants (Chinese patients with terminal cancer n=4, their caregivers n=5, and health care providers n=11) | Semi-structured interviews | Poor understanding of palliative care services available. Cultural taboo of death along with language barriers, and poor health professional understanding of patients’ cultures. |
| 22 | Paal et al., 2017, Germany | To explore the views and end-of-life preferences of patients with a migration history in Germany and to identify migration specific themes, to generate a theoretical hypothesis for further research and clinical applications | Qualitative | 37 patients (Non-migrant German patients n=19, Migrant patients from Europe, US, Israel, Turkey, Indonesia n=18) with advanced/life-limiting disease (Cancer n=28, Chronic, non-malignant disease n=9) receiving palliative care in different settings | Semi-structured interviews | Patients denied the need for palliative care and often did not understand what it was. Talking about the end-of-life was linguistically and culturally suppressed. |
| 23 | Papadopoulos et al., 2007, United Kingdom | To explore the meanings and experiences of cancer of Chinese people in London | Qualitative | 35 participants of Chinese background (Health professionals n=5, Asylum seekers n=7, migrants with unknown legal status n=6, young adults n=7, elders n=10) | Focus group | Stigma associated with cancer, and poor understanding of palliative care services due to health illiteracy (more common in older groups). |
| 24 | Schrank et al., 2017, Austria | To understand staff experiences of the impact of culture on cancer care | Qualitative | 21 healthcare professionals from different settings of oncology and palliative care (Physicians 37%, Nurses 29%, Psychologists 19%) and with a range of individual migration backgrounds (International migrant status 24%, Born in rural areas i.e., within country migration 37%) | Semi-structured interviews | Culture-specific barriers to palliative care uptake including intrafamilial withholding of information, alternative medicines, traditions related to death including avoidance of speaking about death. |
| 25 | Shanmugasundaram et al., 2009, Australia | To explore the issues related to accessing palliative care services for Indian migrants; to identify the effectiveness of palliative care in supporting the patient and family and to recommend strategies for improving this care | Qualitative | 6 family members of Indian terminally ill patients (Advanced cancer n=5, Stroke n=1) | Semi-structured interviews | Respondents lacked awareness of the palliative care services available to them which caused additional burden and mental stress. Participants reported very little cultural-specific services in Australia. |
| 26 | Shaw et al., 2012, Australia | To identify cultural sensitivities that are important to the acceptability of a telephone-based supportive care intervention; to identify cultural barriers and facilitators to intervention participation | Qualitative | 18 participants (Patients n=14, Carers n=4) of Culturally and Linguistically Diverse background (Arab n=10, Chinese n=8) attending community-based Chinese or Arabic cancer support groups. Patients had advanced cancer most commonly at the following sites: breast n=4, gynaecological n=2, prostate n=2 | Focus groups and semi-structured interviews | Patients lacked familiarity with the health care system and had limited understanding of cancer and treatment. Language barriers between patients and health professionals. |
| 27 | Sinclair et al., 2014, Australia | To explore attitudes towards advanced care planning among older, first-generation Dutch-Australian and Italian-Australian migrants | Qualitative | 30 older participants with migrant status (Dutch migrants n=21, Italian migrants n=9) Mean age was 71 for Dutch participants and 74 for Italian participants |
Extended ethnographic interviews and group discussions | Patients were distrustful of medical institutions, and there was a language barrier between patients and health professionals. |
| 28 | Sneesby et al., 2011, Australia | To obtain information to support palliative care healthcare workers to meet the needs of the Sudanese population in death, dying and bereavement | Qualitative | 15 participants identifying as South Sudanese migrants. Their migrations occurred between 6 months and 6 years prior. | Focus groups | Participants had poor understanding of palliative care and wished to avoid discussing death and dying. |
| 29 | Watts et al., 2017, Australia | To identify oncology nurses' and oncologists' individual experiences and challenges in communicating with patients from minority backgrounds | Qualitative | 38 oncology health practitioners (Oncology nurses n=21, Medical oncologists n=12, Radiation oncologists n=5) | Individual interviews or focus groups | Poor confidence among health professionals to work with diverse patients; overall lack of cultural competency. There was a lack of awareness of the support services available to minority patients and their families. Respondents also reported a lack of time to broach palliative and supportive care. |
| 30 | Watts et al., 2018, Australia | To ascertain the systemic barriers encountered by oncology health professionals working with patients from ethnic minorities to guide the development of a communication skills training programme | Qualitative | 38 oncology health practitioners (Oncology nurses n=21, Medical oncologists n=12, Radiation oncologists n=5) | Individual interviews or focus groups | Little formal training for health professionals in cultural competency. Language barriers limited the amount of information regarding palliative care that was able to be conveyed. |
| 31 | Weber et al., 2016, Switzerland | To survey oncology nurses and oncologists about difficulties in taking care of Culturally and Linguistically Diverse patients and about interests in cross-cultural training | Qualitative – descriptive cross-sectional survey | 152 oncology health practitioners (Oncology nurses n=108, Oncologists n=44) | Questionnaire | Communication difficulties surrounding the end-of-life due to a lack of confidence. Further, an absence of written materials in other languages and absence of a shared common language. |
| 32 | Worth et al., 2009, Scotland | To examine the care experiences of South Asian Sikh and Muslim patients in Scotland with life-limiting illnesses and their families, to understand the reasons for any difficulties with access to services and how these might be overcome | Qualitative | 63 participants (Patients n=25, Carers n=18, Key health professionals n=20). Patients were of South Asian Sikh (n=7) or Muslim (n=18) background, and had a diagnosis of cancer (n=10) or other life-limiting condition (n=15) with a prognosis |
Semi-structured interviews | Cultural taboo of discussing dying openly. Stigma associated with palliative care and hospice, and patients were reluctant to receive care from people from a different culture. |
| 33 | Yılmaz et al., 2020, Netherlands | To gain insight into the unfulfilled instrumental and affective needs of Turkish Dutch and Moroccan-Dutch older cancer patients/survivors, the barriers perceived by healthcare professionals in fulfilling these needs, how eHealth tool can support these needs and decrease barriers | Qualitative | 31 participants (Older patients >60 with cancer n=19, Health practitioners n=12) Patients were of Turkish-Dutch (n=10) and Moroccan Dutch (n=9) background. Health practitioners were GPs (n=7) and oncology nurses (n=5) |
Semi-structured interviews, focus groups | Cultural taboo to discuss cancer and death. Health professionals lacked cultural competency, and there was often miscommunication between different clinicians. Language barriers persisted between patients and health professionals. |
| Note that studies 7, 8 and 9 are three publications resulting from the same study. | ||||||
Table 2: Characteristics of included studies.
Assessment of methodological quality
The results of the quality assessment, as outlined in Tables 3a and 3b, were derived using Kmet, Lee and Cook’s assessment tool [16]. Among the evaluated studies, two were rated as having low methodological quality, while the remaining studies demonstrated either moderate (n=10) or high (n=21) methodological quality. Notably, the most prevalent area compromising the quality of methodological quality across the studies was reflexivity. A total of 18 studies scored a ‘0’ in this domain, indicating that researchers in these studies may not have adequately addressed their own biases, assumptions and influence on research processes and findings. Moreover, several of these studies lacked sufficient information about the researchers’ backgrounds, expertise, and the measures taken to mitigate potential biases.
Identified barriers to palliative care uptake
Twenty-three studies examined the barriers to palliative care utilisation related to patients and their families. Of these, 14 studies solely examined the patient/carer perspective, and the remaining 9 surveyed both patient/carer and healthcare practitioner perspectives.
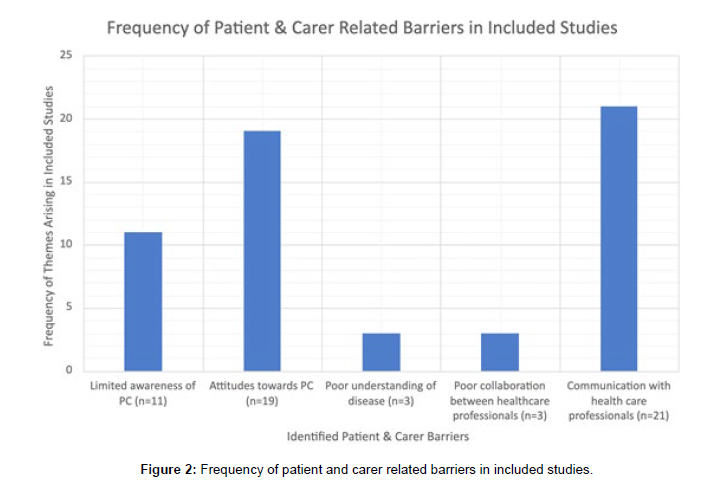
Barriers from the perspective of patients and carers
The most pertinent barriers from the patient/carer perspective included negative attitudes towards palliative care, limited awareness of palliative care, a poor understanding of their disease, and poor communication with healthcare practitioners. The spread of the prevalence of each of these barriers in included studies is shown in Figure 2.
Negative attitudes towards palliative care
Nineteen studies found that patients and their carers held beliefs contrary to the principles of palliative care. These beliefs were mainly sourced from cultural perspectives (n=15) [18-32]. Twelve of these studies revealed a stigma towards palliative care and life-limiting illnesses arising from cultural beliefs and practices [18-20,22,24-28,30- 32]. The most common of these was the taboo nature of conversations surrounding death, end of life, and illness (n=11) [19,20,22,24-28,30- 32]. For instance, Chinese patients often did not disclose their diagnosis to their communities to avoid community backlash and shame [19,22,25,26]. Six studies explored cultural attitudes misaligning with the practices of palliative care [20,21,23,25,29,31]. Three of these studies examined the perceptions of Turkish-Dutch [20,21] and Buddhist [23] migrants who rejected medical intervention at the end-of-life due to the belief that a certain extent of suffering should be inherent during the death process. Six studies highlighted the central role the family unit plays in decision-making and communication, which was often hard to accommodate in inpatient palliative care services [18,20,21,29,31,33]. Four studies showed patients misperceiving palliative care principles, with many conflating it with end-of-life care only [33,36]. Accordingly, they viewed accepting palliative care therapy as ‘giving up’ and necessarily forgoing active disease-modifying treatment.
Limited awareness of palliative care
| Criteria Points | Column11 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Qualitative studies | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total (/20) |
| Bellamy et al. (2013) New Zealand [18] | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 0 | 16 |
| Broom et al. (2019) Australia [47] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 18 |
| Butow et al. (2012) Australia [50] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 0 | 17 |
| Chiang et al. (2015) Australia [19] | 2 | 2 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 0 | 15 |
| De Graaff et al. (2010) Netherlands [40] | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 19 |
| De Graaff et al. (2012) Netherlands [21] | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 19 |
| De Graaff et al. (2012) Netherlands [41] | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 17 |
| Dorji et al. (2021) Canada [23] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 20 |
| Frey et al. (2013) New Zealand [33] | 2 | 1 | 2 | 1 | 2 | 2 | 0 | 1 | 1 | 1 | 13 |
| Green et al. (2018) Australia [42] | 2 | 1 | 2 | 1 | 1 | 2 | 2 | 0 | 2 | 0 | 13 |
| Guo et al. (2021) Jordan [36] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 19 |
| McGrath et al. (2001) Australia [24] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 1 | 0 | 15 |
| Morris et al. (2005) US [43] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 18 |
| Kirby et al. (2017) Australia [48] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 0 | 17 |
| Lim et al. (2019) Australia [25] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 20 |
| Lin et al. (2019) Taiwan [37] | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 1 | 17 |
| Nielsen et al. (2015) Canada [26] | 2 | 1 | 2 | 2 | 1 | 1 | 1 | 2 | 2 | 2 | 16 |
| Paal et al. (2017) Germany [27] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 20 |
| Papadopoulos et al. (2007) UK [28] | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 2 | 0 | 15 |
| Schrank et al. (2017) Austria [44] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 0 | 17 |
| Shanmugasundaram et al. (2009) Australia [38] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 17 |
| Shaw et al. (2012) Australia [39] | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 0 | 2 | 0 | 15 |
| Sinclair et al. (2014) Australia [29] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 0 | 17 |
| Sneesby et al. (2011) Australia [30] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 0 | 17 |
| Watts et al. (2017) Australia [45] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 0 | 17 |
| Watts et al. (2018) Australia [49] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 0 | 17 |
| Weber et al. (2016) Switzerland [31] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 0 | 16 |
| Worth et al. (2009) Scotland [46] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 0 | 16 |
| Yılmaz et al. (2020) Netherlands [32] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 0 | 17 |
| The questions in the checklist used were as follows: 1-Question/objective sufficiently described?; 2-Study design evident and appropriate?; 3-Context for the study clear?; 4-Connection to a theoretical framework/wider body of knowledge?; 5-Sampling strategy described, relevant and justified? 6-Data collection methods clearly described and systematic?; 7-Data analysis clearly described and systematic?; 8-Use of verification procedure(s) to establish credibility?; 9-Conclusions supported by the results?; 10 – Reflexivity of the account? Note that in response to these criteria questions, ‘0’ denotes “No”, ‘1’ denotes “Partial”, and ‘2’ denotes “Yes”. |
|||||||||||
Table 3a: Quality assessment of included qualitative studies.
| Criteria Points | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| QUANTITATIVE STUDIES | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | Total (/20) |
| Alananzeh et al. (2020) Australia [34] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 20 | ||||
| Ayash et al. (2017) United States [40] | 1 | 1 | 2 | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 16 | ||||
| Dhingra et al. (2020) United States [22] | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 18 | ||||
| Green et al. (2019) Australia [35] | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 0 | 2 | 2 | 16 | ||||
| The questions in the checklist used were as follows: 1-Question/objective sufficiently described?; 2-Study design evident and appropriate?; 3-Method of subject/comparison group selection or source of information/input variables described and appropriate?; 4-Subject (and comparison group, if applicable) characteristics sufficiently described?; 5-if interventional and random allocation was possible, was it described?; 6-if interventional and blinding of investigators was possible, was it reported?; 7-If interventional and blinding of subjects was possible, was it reported?; 8-Outcome and (if applicable) exposure measure(s) well defined and robust to measurement/misclassification bias? Means of assessment reported?; 9-Sample size appropriate?; 10-Analytic methods described/justified and appropriate?; 11-Some estimate of variance is reported for the main results?; 12-Controlled for confounding?; 13-Results reported in sufficient detail?; 14-Conclusions supported by the results? Note that in response to these criteria questions, ‘0’ denotes “No”, ‘1’ denotes “Partial”, and ‘2’ denotes “Yes”. |
|||||||||||||||
Table 3b: Quality assessment of included quantitative studies.
Eleven studies found that migrant patients and their carers had little to no awareness of palliative care [22,24-28,30,33,37-39]. Seven studies revealed respondents commonly had unmet information and support needs regarding the palliative care services available to them and how to access them, with this uncertainty causing additional burden and mental stress [24-26,28,33,38,39]. Four studies showed patients did not know the definitions of palliative care [22,25,30,37]. This was commonly due to poor health literacy, illiteracy, or poor education from healthcare staff.
Poor understanding of disease
Three identified studies found that patients and their caregivers occasionally demonstrated limited understanding of their disease processes [28,35,40]. In two of these studies, participants did not completely understand the implications of their initial diagnosis, translating to continuing uncertainty regarding disease course, treatment, and prognostication [28,40]. This restricted the ability of patients and carers to engage in advance care planning and explore the option of palliative care. In addition, carers’ poor understanding of disease sometimes caused potential unintended harm to patients, with one study describing six cases of families attempting to force-feed dying relatives, stemming from a lack of understanding of the physiology of the end-of-life phase, where appetite is lost [35].
Poor communication and collaboration with healthcare professionals
A major reported barrier to the implementation of palliative care was the miscommunication between patients and healthcare professionals, appearing as a central barrier in 21 studies [19,20,24- 27,29-32,35-37,39-46]. Of these, 15 studies revealed that language barriers proved an obstacle to timely palliative care introduction, as migrants comprised a substantial majority of the study population in these studies [19,24-27,29,31,32,39-42,44-46]. The use of interpreters to mitigate this issue posed its own drawbacks, with patients in three studies feeling that using an interpreter impeded their care as they were less likely to ask questions about cancer and treatment [19,42,43]. There was also variability regarding the quality of the interpreter, and in one study, carers cited privacy concerns in using an interpreter, while providers held ethical concerns in utilising a family member for interpretation [42]. Furthermore, six studies revealed patients’ mistrust of clinicians and institutions, which impacted the ability of clinicians to facilitate dialogue with patients, leading to the delayed introduction of palliative care [20,29,30,32,37,42].
Moreover, three studies revealed that patients and carers perceived poor collaboration between healthcare practitioners as a barrier to delivering quality palliative care [25,32,43]. All of these studies revealed that patients reported receiving conflicting information from different providers due to poor documentation and communication between specialists, resulting in inadequacies regarding continuity of care.
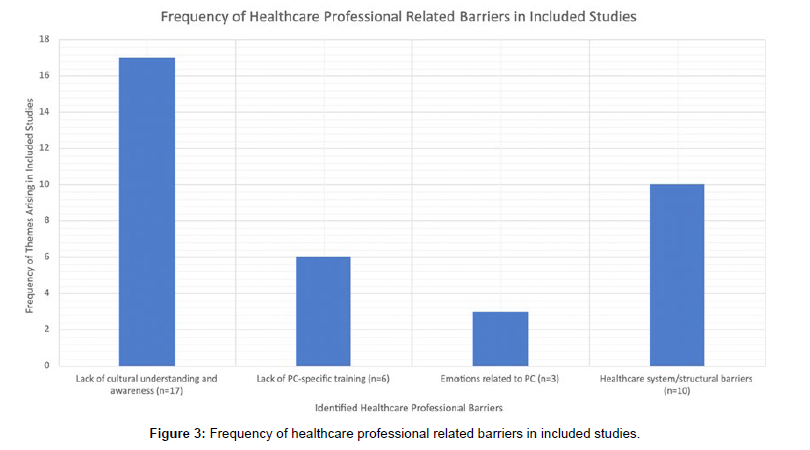
Barriers from the perspective of healthcare professionals
Nineteen studies examined the barriers to palliative care utilisation related to healthcare practitioners (healthcare practitioners), with 10 examining solely the healthcare practitioners' perspective and 9 surveying healthcare practitioners and patient/carer perspectives.
Healthcare practitioners-related barriers included: a lack of cultural understanding and awareness, a lack of palliative care-specific training, emotions related to palliative care, and existing healthcare system/ structural barriers. The spread of the prevalence of each of these barriers in included studies is shown in Figure 3.
Lack of cultural understanding and awareness
Seventeen studies explored clinicians’ lack of cultural understanding as an impediment to early palliative care referral [18,21,26,31-33,37- 39,42-49]. In all 17 studies, providers were not conversant with certain cultural conventions surrounding end-of-life discussion and death/dying rituals. In one study, healthcare practitioners played a gatekeeping role in palliative care by assuming patients would not use the service due to their cultural background and beliefs [33]. Moreover, five studies explored the role of the family unit for migrant patients in shared decision-making and support at the end-of-life, which was often seen as a point of unfamiliarity and a barrier to palliative care delivery for clinicians [18,37,43-45].
Lack of palliative care-specific training
Six studies explored the providers' lack of palliative care-specific training as a barrier to palliative care delivery [18,32,42,43,45,48]. Healthcare practitioners often lacked training in an array of palliative care-specific skills, reporting difficulty in conveying emotional support to patients [43,48], finding a balance between practising with sensitivity while remaining professional, and explaining palliative care to culturally diverse patients with perceived low-health literacy [32,45]. Healthcare practitioners also struggled to navigate familial preferences for non-disclosure to ill relatives despite this conflicting with what is perceived as a professional responsibility to disclose all information to the patient [18,42].
Emotional burden related to palliative care
Three studies explored the emotional burden carried by healthcare practitioners towards palliative care as a barrier to its implementation [42,48,50]. In all studies, respondents had difficulty managing the emotional burden of challenging clinical encounters. One study also revealed a fear of making a ‘bad situation worse’ by speaking to patients about palliative care and forcing them to uncover hidden emotions [42]. Accordingly, providers believed it was therefore easier to avoid these issues by not raising palliative care at all.
Healthcare system/structural barriers
Ten studies explored structural healthcare barriers to implementing early palliative care in migrant populations [18,25,31,36,38- 40,45,46,49]. A pertinent theme that arose was the financial struggle for patients and their families in the face of expensive treatment and frequent hospital attendances (n=4) [25,36,39,40]. Moreover, two studies reported that care settings were unsuitable for the complex cultural needs of family groups, often not being set up to cope with large numbers of family [18,38]. An additional three studies explored miscommunication as another structural healthcare barrier [31,46,49], noting the absence of written materials in other languages explaining services and procedures (n=2) [31,49] and difficulty organising interpreters at short notice (n=2) [46,49]. Two studies also reported on significant time restraints placed on consultations, abrogating patients the chance to discuss their agendas [45,49].
Discussion
Main findings
This review aimed to synthesise and present the available data related to the barriers to palliative care uptake among the culturally and linguistically diverse population, pertinent as the introduction of palliative care in this group is traditionally delayed compared to non-migrant patients. To our knowledge, this is the first review to systematically present evidence on a variety of patient and carer, and healthcare practitioner barriers to palliative care delivery. The results reveal insights into common barriers to palliative care. We discuss these findings to provide direction for developing future interventions to improve palliative care uptake in the culturally and linguistically diverse population.
What this study adds
Barriers among patients and carers
Most studies included in this review identified patient- and carer-related barriers to palliative care uptake in the culturally and linguistically diverse population. These barriers were commonly sourced from cultural attitudes towards death, the end-of-life period, and the nature of suffering [18-32]. Cultural misalignment with medical principles is an essential and recurring theme in the extant body of literature, frequently appearing as a barrier to other medical modalities. For example, several studies exploring the obstacles to migrant healthcare access found that culturally and linguistically diverse patients often avoided healthcare services due to fear of discrimination, a perceived culture of silence, and poor health literacy [51,52].
Similarly, non-migrant patients have frequently stigmatised palliative care, associating it with death and care only at the very end of life [53,54]. In comparison, while culturally and linguistically diverse participants relate stigma to cultural attitudes, non-culturally and linguistically diverse patients in these studies sourced misperceptions of palliative care from the community and previous experiences of family members and friends. Significantly, palliative care continues to be perceived negatively by the general public [55] and medical profession [56] alike, and stigma of any kind has been shown to impact health and therapeutic outcomes deleteriously [57]. In this vein, patients are less likely to access palliative care services if they either experience palliative care stigma from clinicians or endorse it themselves [58].
Moreover, included studies frequently documented patients’ and carers’ lack of awareness and understanding of palliative care processes. This is a theme found in other studies exploring the perceptions of non-migrant patients [53,59], suggesting this theme extends across cultures. Notably, the introduction of palliative care is often delayed until patients request it, despite clinicians possibly wishing to refer patients earlier [60], implying that patients with a poor understanding of palliative care may not have equitable access, compared to those with better health literacy by their unawareness to request it.
These two themes - stigma and unawareness of palliative care - are conceivably sourced from incorrect or misguided education, or a total lack thereof. Therefore, a possible remedy would be introducing an educational initiative to patients and their carers to improve their cognisance of palliative care and dispel common misconceptions. This has been performed in previous studies, where researchers compared patient perceptions of palliative care before and after a definition was provided, demonstrating a temporal link between the educational intervention and amelioration of patient attitudes [53,54]. Notably, the education intervention in these studies was brief and low burden, suggesting a simple educational intervention can shift perspective and understanding in the patient and carer cohort, improving palliative care uptake.
The final theme identified among the patient and carer cohorts was poor communication among healthcare practitioners, patients, and carers. Chiefly, language barriers led to the delayed introduction of palliative care in multiple studies, a theme recurrent in the literature that has been demonstrated to reduce patient satisfaction and the quality of healthcare delivered [61]. In palliative care specifically, several studies have found that limited-English proficiency patients receive worse quality end-of-life care and goals of care discussion than English-proficient patients [62], and that this can be improved with the use of professional interpreters63,64. However, in our review, patients were sometimes reluctant to utilise interpreter services due to privacy concerns and variability in the quality of the interpreter used [19,42,43]. In addition, a review of the literature reported that poor clinical outcomes in interpreting are found with the use of untrained or ad hoc interpreters, defined as “an untrained person called upon to interpret, such as a family member, a bilingual staff member, or a self-declared bilingual in a hospital waiting room” [64]. This contrasts with professional interpreters, who have been shown to improve clinical outcomes substantively [64]. Therefore, to improve palliative care uptake, communication should be prioritised by increasing the availability of professional interpreters in the hospital and clinic setting.
Barriers among healthcare professionals
Several studies identified healthcare professional barriers to the uptake of palliative care in culturally and linguistically diverse populations. Providers’ lack of cultural understanding was identified as the most pertinent barrier to palliative care uptake. Palliative care delivery must consider the shifting and culturally diverse setting in which healthcare is delivered in multicultural societies. Therefore, healthcare practitioners must consider, respect, and become sensitive to the various cultures and cultural norms encountered, especially when dealing with the sensitivities surrounding death and end-of-life [65]. The literature outside this review documents the subjectivity of pain, detailing its dependence on the particular context of a patient, including their cultural background [66], highlighting the necessity of providing culturally-apt healthcare. Several randomised controlled trials have demonstrated the benefit of utilising culturally sensitive material and training for healthcare practitionerss [65,67]. A study by Hölzel et al. randomised 435 adult primary cancer migrant patients to receive either standard translated or culturally sensitive adapted material, measuring the patient-rated usefulness of provided information. Usefulness was significantly higher in the intervention group, suggesting that culturallysensitive material can improve patient-practitioner communication and health outcomes [67]. Another randomised control trial found that cultural sensitivity training in healthcare practitioners increased open-mindedness, cultural awareness, and the ability to communicate with people from minority backgrounds [65]. In this study, after one year, patients who received care from trained providers demonstrated improvement in utilising social resources and overall functional capacity65. Accordingly, healthcare practitioners training in cultural awareness and palliative care principles must be indicated. Studies delineating educational initiatives that combine cultural training with palliative care training should be conducted to improve palliative care uptake in the culturally and linguistically diverse population.
Moreover, providers’ lack of palliative care-specific training was reported as a barrier in multiple studies. This finding is consistent with other studies that found a lack of palliative care inclusion in medical school curricula in the US, Australia, and the UK [68,69]. Where palliative care education has been included, it is often delivered inconsistently, with significant variation between different medical schools [70,71]. Additionally, this teaching is often presented within the classroom, with many students completing medical school without clinical exposure to death or dying patients [69]. This largely contributes to the feelings of under-preparedness and inadequacy frequently reported by medical students and junior physicians alike, resulting in healthcare professionals often lacking the skills to convey emotional support to patients and explain the principles of palliative care sensitively and effectively to culturally and linguistically diverse recipients. With an ever-ageing population that will exhibit a longer chronic phase before death, almost all healthcare professionals will encounter patients with palliative care needs.
Furthermore, an undertrained medical workforce has implications for patient outcomes. For example, a randomised control trial by Thoonsen et al. found that General Practitioners trained with a palliative care education programme could identify more patients suitable for palliative care than the control group (median 3 vs. 2, p=0.046) and more often provided multidimensional care than the group of untrained GPs (p=0.024) [72]. It can be argued that an unskilled workforce will fall short in identifying and addressing the complex supportive care needs of patients with life-limiting illnesses. Therefore, it is imperative to introduce and standardise palliative care education and training in medical school and post-graduate speciality curricula to improve palliative care delivery.
Strengths and limitations of this study
While rigorously conducted, this systematic review has several limitations. First, while we performed a comprehensive search, it is possible that articles were missed or overlooked. Second, the studies were heterogeneous regarding palliative care providers (general practitioners, oncologists, interpreters, specialist palliative care physicians) and the type of palliative care provided (general, specialist, home). Third, most of the included studies were qualitative and suffered from limited sample sizes, restricting the generalisability of the results to other populations. However, this was addressed by including studies from diverse ethnographic populations and countries (including developed and developing nations), allowing for a universal exploration into migrant-perceived barriers to palliative care. Given the exponentially increasing rate of migration worldwide coupled with an ever-ageing population, healthcare systems will see a rise in culturally and linguistically diverse patients needing palliative care services over the coming years.
Conclusion
Palliative care can significantly benefit patients from culturally and linguistically diverse backgrounds who have unmet supportive care needs. However, our systematic review has identified several barriers that impede the provision of streamlined palliative care services to this population group. These barriers can be primarily attributed to poor education and communication between patients, their carers, and healthcare professionals, as well as inadequate training of healthcare professionals in palliative care. To improve access, utilisation, and delivery of palliative care to this traditionally underserved population, it is essential to develop interventions and educational initiatives targeting these themes. By identifying these barriers, we hope to guide the development of initiatives that will effectively address the challenges faced by patients from culturally and linguistically diverse backgrounds and ensure that they receive the palliative care they need and deserve.
Acknowledgements
The authors would like to thank John Holgate and Marika Sablatura Nagy, medical librarians at St. George Hospital Sydney, for their help and guidance in developing and conducting the search strategy for this systematic review. The authors would also like to thank Dr. Sonit Singh for his help in guiding the analytical methods used in this paper.
Conflicting interests and other information
No competing financial interests or other conflicts of interest exist concerning this article's research, authorship, and publication. Data sourced in writing this review is available within the article. As this present review used publicly accessible data as evidence, no ethics approval was required. This review was not registered and a protocol was not prepared previously. This review utilised publicly accessible data as evidence, available through search engines and public databases.
References
- Saunders C (2001) The evolution of palliative care. J R Soc Med 94:430-432.
- Sepúlveda C, Marlin A, Yoshida T, Ullrich A (2002) Palliative Care: The World Health Organization's Global Perspective. J. Pain Symptom Manage 24:91-96.
- World Health Organization (2007) Palliative care.
- World Health Organization (2020) Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2019 global survey.
- Greer JA, Jackson VA, Meier DE, Temel JS (2013) Early integration of palliative care services with standard oncology care for patients with advanced cancer. CA Cancer J Clin 63:349-363.
- Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, et al. (2010) Early Palliative Care for Patients with Metastatic Non–Small-Cell Lung Cancer. N Eng J Med 363:733-742.
- Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, et al. (2009) Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 302:741-749.
- Gade G, Venohr I, Conner D, McGrady K, Beane J, et al. (2008) Impact of an Inpatient Palliative Care Team: A Randomized Controlled Trial. J Palliat Med 11:180-190.
- Segal UA (2019) Globalization, migration, and ethnicity. Public Health 172:135-142.
- Clancy M, Taylor J, Bradbury-Jones C, Phillimore J (2020) A systematic review exploring palliative care for families who are forced migrants. J Adv Nurs 76:2872-2884.
- Kwok HHY, Low J, Devakumar D, Candy B (2020) Experience and perspectives on palliative or end-of-life care of Chinese people and their families as immigrants to high-income countries: a systematic review and thematic synthesis. BMJ Glob Health 5:003232.
- Shabnam J, Timm HU, Nielsen DS, Raunkiaer M (2021) Palliative Care Utilization among Non-Western Migrants in Europe: A Systematic Review. J Immigr Minor Health 1-19.
- Evans N, Meñaca A, Andrew EV, Koffman J, Harding R, et al. (2012) Systematic review of the primary research on minority ethnic groups and end-of-life care from the United Kingdom. J Pain Symptom Manage 43:261-286.
- de Graaff FM, Mistiaen P, Devillé WLJM, Francke AL (2012) Perspectives on care and communication involving incurably ill Turkish and Moroccan patients, relatives and professionals: a systematic literature review. BMC Palliat Care 11:1-37.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev 88: 105906.
- Kmet LM, Cook LS, Lee RC (2004) Standard quality assessment criteria for evaluating primary research papers from a variety of fields.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, et al. (2006) Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme. Version 1:92.
- Bellamy G, Gott M (2013) What are the priorities for developing culturally appropriate palliative and end-of-life care for older people? The views of healthcare staff working in New Zealand. Health Soc Care Community 21:26-34.
- Chiang YC, Collins A, Chopra P, Lu T, Tan ES, et al. (2015) Understanding the experiences of Mandarin-speaking patients diagnosed with life-threatening cancer in Australia. Palliat Support Care 13:1317-1323.
- De Graaff FM, Francke AL, Van Den Muijsenbergh METC, Van Der Geest S (2010) 'Palliative care': A contradiction in terms? A qualitative study of cancer patients with a Turkish or Moroccan background, their relatives and care providers. BMC Palliat Care 9:19.
- de Graaff FM, Francke AL, van den Muijsenbergh METC, van der Geest S (2012) Understanding and improving communication and decision-making in palliative care for Turkish and Moroccan immigrants: A multiperspective study. Ethn Health 17:363-384.
- Dhingra L, Cheung W, Breuer B, Huang P, Lam K, et al. (2020) Attitudes and beliefs toward advance care planning among underserved Chinese-American immigrants. J Pain Symptom Manage 60:588-594.
- Dorji N, Lapierre S (2021) Perception of death and preference for end-of-life care among asian buddhists living in montreal, Canada. Death Stud 46:1933-1945.
- McGrath P, Vun M, McLeod L (2001) Needs and experiences of non-English-speaking hospice patients and families in an English-speaking country. Am J Hosp Palliat Care 18:305-312.
- Lim BT, Butow P, Mills J, Miller A, Pearce A, et al. (2019) Challenges and perceived unmet needs of Chinese migrants affected by cancer: Focus group findings. J Psychosoc Oncol 37:383-397.
- Nielsen LS, Angus JE, Howell D, Husain A, Gastaldo D (2015) Patient-centered care or cultural competence: negotiating palliative care at home for Chinese Canadian immigrants. Am J Hosp Palliat Care 32:372-379.
- Paal P, Bukki J (2017) "If I had stayed back home, I would not be alive any more..." -- Exploring end-of-life preferences in patients with migration background. PLoS One 12:314.
- Papadopoulos I, Guo F, Lees S, Ridge M (2007) An exploration of the meanings and experiences of cancer of Chinese people living and working in London. Eur J Cancer Care 16:424-432.
- Sinclair C, Smith J, Toussaint Y, Auret K (2014) Discussing dying in the diaspora: Attitudes towards advance care planning among first generation Dutch and Italian migrants in rural Australia. Soc Sci Med 101:86-93.
- Sneesby L, Satchell R, Good P, van der Riet P (2011) Death and dying in Australia: Perceptions of a Sudanese community. J Adv Nurs 67:696-702.
- Weber O, Sulstarova B, Singy P (2016) Cross-Cultural Communication in Oncology: Challenges and Training Interests. Oncol Nurs Forum 43:24-33.
- Yılmaz NG, Sungur H, van Weert JCM, van den Muijsenbergh M, Schouten BC (2020) Enhancing patient participation of older migrant cancer patients: needs, barriers, and eHealth. Ethn Health 27:1123-1146.
- Frey R, Gott M, Raphael D, Black S, Teleo‐Hope L (2013) 'Where do I go from here'? A cultural perspective on challenges to the use of hospice services. Health & Social Care in the Community 21:519-529.
- Alananzeh I, Halcomb E, Chan A (2020) Support preferences for Arabic people with a chronic condition living in Australia: A descriptive survey. Nurs Health Sci 22:1076-1083.
- Green A, Jerzmanowska N, Thristiawati S, Green M, Lobb EA (2019) Culturally and linguistically diverse palliative care patients' journeys at the end-of-life. Palliat Support Care 17:227-233.
- Guo P, Alajarmeh S, Alarja G, Alrjoub W, Al-Essa A, et al. (2021) Compounded trauma: A qualitative study of the challenges for refugees living with advanced cancer. Palliat Med 35:916-926.
- Lin CP, Evans CJ, Koffman J, Sheu SJ, Hsu SH, et al. (2019) What influences patients' decisions regarding palliative care in advance care planning discussions? Perspectives from a qualitative study conducted with advanced cancer patients, families and healthcare professionals. Palliat Med 33:1299-1309.
- Shanmugasundaram S, O'Connor M (2009) Palliative care services for Indian migrants in Australia: Experiences of the family of terminally Ill patients. Indian J Palliat Care 15:76-83.
- Shaw J, Butow P, Sze M, Young J, Goldstein D (2013) Reducing disparity in outcomes for immigrants with cancer: A qualitative assessment of the feasibility and acceptability of a culturally targeted telephone-based supportive care intervention. Support Care Cancer 21:2297-2301.
- Ayash C, Costas-Muniz R, Badreddine D, Ramirez J, Gany F (2017) An Investigation of Unmet Socio-Economic Needs Among Arab American Breast Cancer Patients Compared with Other Immigrant and Migrant Patients. J Community Health 43:89-95.
- De Graaff FM, Francke AL, van Muijsenbergh METC, der Geest S (2012) Talking in triads: Communication with Turkish and Moroccan immigrants in the palliative phase of cancer. J Clin Nurs 21:3143-3152.
- Green A, Jerzmanowska N, Green M, Lobb EA (2018) 'Death is difficult in any language': A qualitative study of palliative care professionals' experiences when providing end-of-life care to patients from culturally and linguistically diverse backgrounds. Palliat Med 32:1419-1427.
- Morris WM, Wenrich MD, Nielsen EL, Treece PD, Jackson J, et al. (2005) Communication about End-of-Life Care between Language-Discordant Patients and Clinicians: Insights from Medical Interpreters. J Palliat Med 8:1016-1024.
- Schrank B, Rumpold T, Amering M, Masel EK, Watzke H, et al. (2017) Pushing boundaries-culture-sensitive care in oncology and palliative care: a qualitative study. Psycho-oncology 26:763-769.
- Watts KJ, Meiser B, Zilliacus E, Kaur R, Taouk M, et al. (2017) Communicating with patients from minority backgrounds: Individual challenges experienced by oncology health professionals. Eur J Oncol Nurs 26:83-90.
- Worth A, Irshad T, Bhopal R, Brown D, Lawton J, et al. (2009) Vulnerability and access to care for South Asian Sikh and Muslim patients with life limiting illness in Scotland: Prospective longitudinal qualitative study. BMJ: British Medical Journal 338:1-19.
- Broom A, Parker RB, Kirby E, Kokanović R, Woodland L, et al. (2019) A qualitative study of cancer care professionals' experiences of working with migrant patients from diverse cultural backgrounds. BMJ Open 9:956.
- Kirby E, Broom A, Good P, Bowden V, Lwin Z (2017) Experiences of interpreters in supporting the transition from oncology to palliative care: a qualitative study. Asia Pac J Clin Oncol 13:497-505.
- Watts KJ, Meiser B, Zilliacus E, Kaur R, Taouk M, et al. (2018) Perspectives of oncology nurses and oncologists regarding barriers to working with patients from a minority background: Systemic issues and working with interpreters. Eur J Cancer Care 27:1-9.
- Butow PN, Lobb E, Jefford M, Goldstein D, Eisenbruch M, et al. (2012) A bridge between cultures: interpreters' perspectives of consultations with migrant oncology patients. Supportive Care Cancer 20:235-244.
- Guirgis M, Nusair F, Bu YM, Yan K, Zekry AT (2012) Barriers faced by migrants in accessing healthcare for viral hepatitis infection. Intern Med J 42:491-496.
- Sherif B, Awaisu A, Kheir N (2022) Refugee healthcare needs and barriers to accessing healthcare services in New Zealand: a qualitative phenomenological approach. BMC Health Serv Res 22:1310.
- Donlan J, Ufere NN, Indriolo T, Jackson V, Chung RT, et al. (2020) Patient and Caregiver Perspectives on Palliative Care in End-Stage Liver Disease. J Palliat Med 24:719-724.
- Zimmermann C, Swami N, Krzyzanowska M, Leighl N, Rydall A, et al. (2016) Perceptions of palliative care among patients with advanced cancer and their caregivers. CMAJ 188:217-227.
- McIlfatrick S, Slater P, Beck E, Bamidele O, McCloskey S, et al. (2021) Examining public knowledge, attitudes and perceptions towards palliative care: a mixed method sequential study. BMC Palliat Care 20:44.n
- Von Roenn JH, Voltz R, Serrie A (2013) Barriers and approaches to the successful integration of palliative care and oncology practice. J Natl Compr Canc Netw 11:11-16.
- Hatzenbuehler ML, Phelan JC, Link BG (2013) Stigma as a fundamental cause of population health inequalities. Am J Public Health 103:813-821.
- Shen MJ, Wellman JD (2019) Evidence of palliative care stigma: The role of negative stereotypes in preventing willingness to use palliative care. Palliat Support Care 17:374-380.
- Carbonneau M, Davyduke T, Spiers J, Brisebois A, Ismond K, et al. (2018) Patient Views on Advance Care Planning in Cirrhosis: A Qualitative Analysis. Can J Gastroenterol Hepatol 18.
- Low J, Davis S, Vickerstaff V, Greenslade L, Hopkins K, et al. (2017) Advanced chronic liver disease in the last year of life: a mixed methods study to understand how care in a specialist liver unit could be improved. BMJ Open 7:6887.
- Al Shamsi H, Almutairi AG, Al Mashrafi S, Al Kalbani T (2020) Implications of Language Barriers for Healthcare: A Systematic Review. Oman Med J 35:122.
- Silva MD, Genoff M, Zaballa A, Jewell S, Stabler S, et al. (2016) Interpreting at the End of Life: A Systematic Review of the Impact of Interpreters on the Delivery of Palliative Care Services to Cancer Patients with Limited English Proficiency. J Pain Symptom Manage 51:569-580.
- Flores G (2005) The Impact of Medical Interpreter Services on the Quality of Health Care: A Systematic Review. Med Care Res Rev 62:255-299.
- Karliner LS, Jacobs EA, Chen AH, Mutha S (2007) Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res 42:727-754.
- Majumdar B, Browne G, Roberts J, Carpio B (2004) Effects of Cultural Sensitivity Training on Health Care Provider Attitudes and Patient Outcomes. J Nurs Scholarsh 36:161-166.
- Givler A, Bhatt H, Maani-Fogelman PA (2020) The importance of cultural competence in pain and palliative care. StatPearls.
- Hölzel LP, Ries Z, Kriston L, Dirmaier J, Zill JM, et al.(2016) Effects of culture-sensitive adaptation of patient information material on usefulness in migrants: a multicentre, blinded randomised controlled trial. BMJ Open 6:2008.
- Horowitz R, Gramling R, Quill T (2014) Palliative care education in US medical schools. Med Educ 48:59-66.
- Chiu N, Cheon P, Lutz S, Lao N, Pulenzas N, et al. (2015) Inadequacy of Palliative Training in the Medical School Curriculum. J Cancer Educ 30:749-753.
- Lloyd-Williams M, MacLeod RD (2004) A systematic review of teaching and learning in palliative care within the medical undergraduate curriculum. Med Teach 26:683-690.
- Bickel-Swenson D (2007) End-of-life training in U.S. medical schools: a systematic literature review. J Palliat Med 10:229-235.
- Thoonsen B, Gerritzen SH, Vissers KC, Verhagen S, van Weel C, et al. (2019) Training general practitioners contributes to the identification of palliative patients and to multidimensional care provision: secondary outcomes of an RCT. BMJ Support Palliat Care 9:18.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Abasseri M, Hoque S, Kochovska S, Caldwell K, Sheahan L, et al.(2023) Barriers to Palliative Care Uptake in Culturally and Linguistically DiversePopulations: A Systematic Review. J Palliat Care Med 13: 542. DOI: 10.4172/2165-7386.1000542
Copyright: © 2023 Abasseri M, et al. This is an open-access article distributedunder the terms of the Creative Commons Attribution License, which permitsunrestricted use, distribution, and reproduction in any medium, provided theoriginal author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1645
- [From(publication date): 0-2023 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 1408
- PDF downloads: 237