Balance Rehabilitation using Xbox Kinect among an Elderly Population: A Pilot Study
Received: 14-Apr-2015 / Accepted Date: 22-Apr-2015 / Published Date: 28-Apr-2015 DOI: 10.4172/2165-7025.1000261
Abstract
With the current aging of the population, falls among the elderly has become a major concern for health care professionals. One major component of fall prevention is balance training, which could be achieved using the Microsoft Xbox Kinect. This video game platform uses motion sensors to capture participants’ movements and to provide visual feedback. In addition to its use for recreational purposes, it has the potential to be a great home-based tool for balance rehabilitation. The objectives of the current study are to assess its efficacy as a single tool for balance training, as well as measuring the population’s interest in this approach. Three participants with balance problem were included in this multiple-case study. They all completed the standardised 10-week program consisting of two 30-minute sessions of balance training through Kinect per week in addition to their usual multidisciplinary treatments. They were evaluated before the intervention (T0) and immediately after (T1). The following outcomes were assessed: 1) balance (Berg Balance Scale [BBS]), 2) mobility (Timed Up-and-Go [TUG]), 3) walking speed on 5m, 4), lower limb strength (Sit-to- Stand [STS]), 5) fear of falling (Activity-Specific Balance Confidence Scale [ABC Scale]) and 6) satisfaction (modified Quebec User Evaluation of Satisfaction with Assistive Technology [QUEST]). We observed an improvement in BBS, TUG and ABC scores for every participant. However, the STS score improved for two of the three participants and the walking speed stayed the same for everybody. Moreover, all of the participants were satisfied with their experience. Overall, the results showed that the Xbox Kinect could be a great adjunct to a multidisciplinary treatment to improve balance. Nevertheless, high-quality studies with more powerful designs are needed to prove the efficacy and applicability of this approach for balance rehabilitation.
Keywords: Balance; Rehabilitation; Satisfaction; Xbox Kinect
360443Introduction
With the actual aging of the population, falls among the elderly has become a major concern. Indeed, more than one third of the elderly people fall every year and half of them will fall again during the same year [1-3]. In Canada, in the beginning of the century, the expenses related to falls were estimated at 2.4 billion dollars, with an estimated increase up to 240 billion in 2040 [4].
Falling is a multifactorial situation resulting from the interaction between multiple risk factors. Among these factors, some cannot be changed while some are modifiable, such as: balance, strength, environment, etc. [2]. The latter are the factors which the professionals will base their intervention on. A review of the literature about fall prevention strategies showed that balance training is the key component of an exercise program [5]. A meta-analysis of randomized clinical trials (Cochrane Review) showed that exercise programs specifically aiming at balance improvement reduced the risk of falling of 25% [6]. Multiple conventional and non-conventional rehabilitation approaches exist to maintain or improve balance. Examples of non-conventional therapies include tango [7], yoga [8-10], and Tai Chi [11-14].
More recently, game consoles gain in interest. Indeed, the Nintendo Wii® console [15-19] and the Xbox Kinect® console [20-22] are now studied as a rehabilitation intervention tool. The main advantages of using the Nintendo Wii® and the Xbox Kinect® in rehabilitation is the possibility to use them at home, their low cost compared to other treatment methods, and their lucrative aspect benefiting compliance to treatment [21]. Actually, what differentiates these two video game consoles is the way they perceive motion. The Nintendo Wii works with a hand-held motion sensor and a force platform called the “Wii Balance Board”. The Xbox Kinect, on the other hand, works with infrared sensors that capture movements, thus eliminating any risk associated with standing on a platform and letting the upper limb free for movement.
Up to now, the Nintendo Wii has been well studied among the population at risk of falling [16,23]. Results show a tendency towards a gain in balance retraining. However, studies pertaining to the Xbox Kinect are still lacking regarding the same population [18,20,22]. Based on the increase in popularity of the use of Kinect for rehabilitation purposes, and with so few studies published to date, the objective of this study is to determine if the Xbox Kinect could enhance balance among an elderly population at risk of falling.
Method
Design
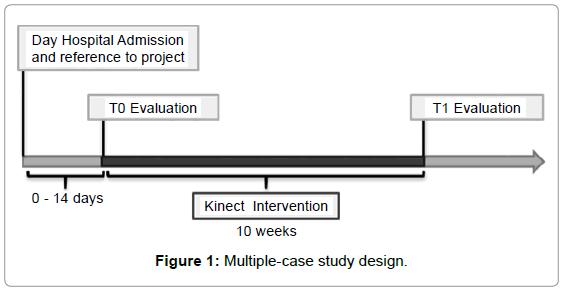
A multiple-case study design was retained in this pilot project. Measurement times were conducted at baseline (T0) and at the end of the 10-week Kinect intervention (T1). The evaluation was done by research agents who received a standardized training on measurement tools used in the study (Figure 1).
Participants and Recruitment Procedures
The studied population consisted of adults older than 65 years old with balance problems, admitted to the geriatric day hospital of the Centre de Santé et de Services Sociaux – Institut Universitaire de Gériatrie de Sherbrooke (CSSS-IUGS). Convenience sampling was used. Inclusion criteria were to have: 1) a BBS score between 41-52/56 or a fall during the last 6 months, and 2) a Modified Mini-Mental State (3MS) score > 65/100. Patients were excluded if they had: 1) a medical contraindication to physical activity, or 2) a physical or mental incapacity limiting participation. All participants were recruited by the treating doctors at the geriatric day hospital. After confirming admissibility of a patient and getting his/her approval to be contacted by a member of the research team, the study was explained to the potential participants and he/she was asked to sign the ethics form approved by the Ethics Committee of the Research Center on Aging of the CSSS-IUGS.
Intervention
The intervention consisted of a 10-week program, with bi-weekly individual sessions of 30 minutes, supervised by a physical therapist at the day hospital based at the CSSS-IUGS. The specific balance training with the Kinect console was added to every participant’s multidisciplinary treatments. A specific progression in the difficulty level of the games over the 10 weeks was determined by the physical therapist to consistently challenge the participant’s balance to allow improvement. An explanation on how the Xbox Kinect works and the goal of the individual games was given to every participant to assure their complete comprehension. An individual approach was used in order to adapt the program to every participant’s condition and to assure security (e.g. small parallel bars and balance belt were available if necessary).
The Kinect intervention included the following Kinect games: 1) Kinect Sports, 2) Kinect Adventures, 3) Your Shape Fitness Evolved, and 4) Carnival (Table 1). These allowed a combination of specific movements of the body, weight transfers and direction changes. These games were chosen to stimulate the different physical components used to improve balance. A 20-session sequence of gaming was established to help the therapist assure a controlled progression. At any time, for a safety concern, the therapist was allowed to modify the session scheduled to fit the participant’s capacities (Table 1).
| Kinect games | Specific games |
|---|---|
| Kinect Sports | Bowling Boxing Table Tennis Soccer Track and Field |
| Kinect Adventures | 20 000 leaks (all levels) Space Pop |
| Your Shape Fitness Evolved | Cardio boxing Stack ‘em up (levels 1, 2) Wallbreaker Light Race Zen (yoga) |
| Carnival | Gold Rush Mountain Funnel Cakes Fall Alley Ball Knockout Punch |
Table 1: Kinect games used in the study.
Outcome measures
Balance was evaluated using the Berg Balance Scale (BBS) [24], composed of 14 functional tasks. A 5-point Likert scale (0-4) was used for every task, for a total of 56 points. Walking was evaluated with the Timed Up and Go (TUG) [25]. This test assesses mobility and more specifically the sitting to standing transfer as well as direction changes that require balance abilities. The participant has to stand up from a chair, walk for 3 m, turn around and walk back to the chair to his/her original sitting position. The walking speed was also measured, where the participants were asked to walk as fast and comfortable as they could in a safe manner, on a distance of five meters, with their walking aid if applicable. The time to cross this distance was noted in seconds. Global strength in the lower limbs was evaluated with the Sit to Stand Test (STS) [26,27]. The total time taken by the participant to make five successive repetitions of sitting to standing was noted.
The French version of the Activity-Specific Balance Confidence Scale (ABC scale) [28] was used to measure the fear of falling. This questionnaire contained 15 questions with an activity continuum from « not at all confident » to « very confident ». Therefore, each activity was marked from 0 to 3 according to this continuum for a maximum of 45 points. The score was then converted into a percentage on a scale of 100%. The 16th item of the French version of the questionnaire was eliminated to conform to the English version.
The satisfaction of the participants toward the study was objectivised by the scale of the modified version of Quebec User Evaluation of Satisfaction with Assistive Technology (modified QUEST) [29,30]. The original scale was used to evaluate the satisfaction toward the use of a walking aid and the appreciation of specific characteristics of the aid. A new version of the scale was adapted to determine the satisfaction of the patient toward the research project. The modified version consisted of three scales evaluating: 1) the satisfaction related to the technology, 2) the intervention, and 3) the services received. The scores of the scales were on 15 points, 30 points and 10 points, respectively, with a total score on 55 points
Results
Description of the sample
Four participants were admitted in the study, but only three participants (n=3) completed the intervention session. The one that withdrew from the study during the intervention did so because she felt the use of the Kinect console was too difficult (Table 2).
| Characteristics | Participant 1 | Participant 2 | Participant 3 |
|---|---|---|---|
| Gender | Woman | Woman | Woman |
| Age (years) | 82 | 80 | 92 |
| Dominance | Right | Right | Right |
| Living alone | Yes | Yes | Yes |
| Number of fall in the last 6 months | 3 | 4 | 1 |
Table 2: Characteristics of the participants.
Physical outcomes
The results for the Berg Balance Scale (/56) showed a tendency towards improvement, as well as the Timed Up and Go Test (seconds) varying between 0.6s and 14.6s. The STS (seconds) showed an improvement of less or equal to five seconds for two of the participants, while the other did not change her performance. Walking speed (seconds) stayed the same after the intervention for every participant (Table 3).
| Outcomes | Instrument tool | Participant 1 | Participant 2 | Participant 3 | ||||
|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T0 | T1 | T0 | T1 | |||
| Physical | Balance | Berg Balance Scale (BBS) (/56) | 43 | 50 | 43 | 47 | 26 | 29 |
| Global mobility | Timed up and go (TUG) (s) | 11.7 | 11.1 | 30.0 | 15.4 | 29.0 | 22.0 | |
| Global Lower Limb Strength | Sit to Stand (STS) (s) | 22.1 | 18.5 | 50.9 | 46.3 | 24.0 | 24.0 | |
| Walking speed | Walking speed (5m) (m/s) | 1.2 | 1.3 | 0.5 | 0.8 | 0.6 | 0.7 | |
| Behavioral | Fear of falling | ABC scale (/100%) | 46.6 | 71.1 | 71.1 | 73.3 | 44.4 | 53.3 |
Table 3: Results for physical, behavioral and compartmental outcomes.
Psychological outcomes
For the psychological variable, the modified QUEST (/55) showed a very high satisfaction of the participants toward the study. Only participant 3 seemed to have less appreciation regarding the intervention (Table 4).
| Modified ÉSAT scales | Participant 1 | Participant 2 | Participant 3 |
|---|---|---|---|
| Technologie (/15) | 15 | 13 | 13 |
| Intervention (/30) | 28 | 29 | 24 |
| Services (/10) | 10 | 8 | 8 |
| Total score (/55) | 53 | 50 | 45 |
Table 4: Satisfaction of participants concerning their experience (T1).
Discussion
The aim of this pilot study was to determine if the Xbox Kinect® could be an alternative intervention in balance rehabilitation in the elderly population. The results showed that using video games could be a useful tool to improve balance.
These results are similar to other studies’ results, such as the one conducted by Lai et al. (2013) [31], which demonstrated that using an interactive video-game based program (XaviX port) could improve balance in community living elderly. Lai et al. demonstrated improvement in the BBS and the TUG after an 18-session intervention. This is in accordance with the results obtained in the present study. More precisely, all of the participants showed clinically significant improvement of BBS after the intervention, demonstrating the positive effect of the intervention on balance.
These improvements led to the attainment of the threshold (score< 45) associated with a low risk of falling in activities of daily living [32] for two of the three participants (participants 1 and 2). The achievement of such an improvement in balance is the goal of a successful rehabilitation intervention. For the other participant (participant 3), there was an improvement of 3 points in the BBS score, but this was not enough to reach the threshold associated to lower risk of falling. This result can be explained by the facts that the initial balance performance of participant 3 was a lot lower than the other participants (score of 26 vs. 43), she was older (92 vs. < 82 years old) and her satisfaction about the intervention lower. Our hypothesis for the lack of improvement for participant 3 is that she took 13 weeks to complete 17 sessions instead of the 10 weeks initially planned to complete 20 sessions because of a lack of attendance and motivation to complete all of the sessions. This lack of compliance most likely impeded on the intervention’s efficacy. It is recognised that motivation towards exercises is related to better performance [33-35].
For the TUG, participant 1 showed no improvement in her performance. However, she was not at risk at T0 with a score below 12s [36], leading to a decreased probability of improvement after the intervention. Unlike participant 1, participants 2 and 3 showed a poor performance at T0 and improved drastically their performance at T1 (Δ = 14.6 and 7.0, respectively). These differences are higher than the error that is associated to the standard error of measurement, which is 5.5% [37]. However, none of them reached the threshold associated with a decreased risk of falling (score < 12s) [36]. Based on these results, it seems that balance (BBS score) is not directly related to sitting to standing transfer, walking abilities and direction changes (TUG score).
There was improvement in the STS test for two participants (Δ = 3.6 and 4.6 for participant 1 and 2, respectively), but not for participant 3. The differences obtained were not associated to the standard error measurement set at 6.3% [38]. However, all participants were over the optimal cut-off of 15 s, both at T0 and T1. Our results are similar to the study conducted by Kim et al. [39] using the Xbox Kinect. Indeed, by doing the Kinect program, the participants had to somewhat stand for a long period of time which can increase the strength of their lower limbs.
The walking speed of all participants showed some small improvement after the intervention (Δ between 0.1 and 0.3). Even if the differences are smalls, they are still meaningful as they at least reached the minimum meaningful change in walking speed of approximately 0.1 m/s [40]. Moreover, participants 2 and 3 were below the cut off of 0.7 m/s, which put them in the “at risk of fall” category. It seems that the Kinect does not have a really strong effect on walking speed, which is not surprising because the Kinect games do not work on this specific task. However, it was interesting to evaluate that outcome even though our intervention did not specifically work on the capacity of walking because it could have been improved by some indirect effects.
As we can see with the ABC Scale, participants who presented fear of falling at T0 (participant 1 and 3) improved their score after the intervention. No clinical change occurred with the participant 2 [41], but he presented only a slight fear of falling at the beginning, leading to poor probability of significant change.
The satisfaction of the participants toward the study evaluated by the modified QUEST was good in all three sections of the questionnaire: technology, intervention and services. The participant 1 was more satisfied toward the study than participant 2 who was more satisfied than participant 3.
What cognitive ability is necessary to use the Kinect as a balance intervention? The participant who did not completed the 10-week Kinect intervention seemed to have cognitive and comprehension difficulties that could have impeded the intervention sessions with the Kinect®. Based on this information, the Xbox Kinect could be of better use in rehabilitation with a population that has a minimum of cognition and comprehension to understand the tasks and that has enough physical skills to apply the tasks used in the game console. Motivation and adherence to treatment would therefore also be improved.
Internal validity must be discussed. Indeed, selection biases cannot be excluded. The small sample number and recruitment by the rehabilitation team may have led to the selection of only those who present the best potential to improve. Moreover, the persons may have accepted to participate because they are more open to computer technology and video games.
Information bias does not seem to be an issue. Indeed, choice of valid and reliable tests and standardization of the assessors led to a decrease of this type of bias. The strengths of our study were that the 20-session program was standardized so exercises done over time were not influenced by the patient’s or the therapist’s preferences. Therapists assessing and treating the participants were not the same. Participants also appreciated the experience as detailed above.
However, many limits were found in this study. First, there was no control group and the sample was small (n=3). We cannot say if improvements shown in our pilot study are related to the intervention or happened because of chance or natural recovery. Therefore, they cannot be generalized to our population. Cognitive impairments were the most frequent reason why patients were not referred or included in the study, regardless of the 3MS score threshold (23/30). Although the program was standardized, factors inherent to a clinical setting such as individual differences, limitations and pain forced minor modifications along the 10-week program. One confounding bias is that some patients also received occupational therapy consisting partially of balance physical therapy-like interventions, thus influencing our results. Also, considering the interrater reliability of the measurement tools, the fact that various evaluators assessed the participants at both T0 and T1 may have influenced our results, but this bias was attenuated by a standardized training given to all the evaluators.
Conclusion
Overall, our study has contributed to expanding the knowledge about the possible use of the Xbox Kinect as a new rehabilitation tool for balance deficits, especially in a home setting. In a society where the access time to a rehabilitation program is in constant increase and with an aging population at risk of falling we can see the benefits in the future of a Kinect home-based program to improve balance. Nevertheless, further research is indicated to enhance the current literature, especially among a larger population who suffers little cognitive impairment, as it was one of our main limits. Comparing traditional treatments with or without adding extra Kinect training sessions would be very interesting, being that it may be a good addition to the treatment for balance or fall prevention.
Acknowledgements
We would like to thank all the participants who took part in this study. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Costello E, Edelstein JE (2008) Update on falls prevention for community-dwelling older adults: review of single and multifactorial intervention programs. J Rehabil Res Dev 45: 1135-1152.
- Fabre JM, Ellis R, Kosma M, Wood RH (2010) Falls risk factors and a compendium of falls risk screening instruments. J GeriatrPhysTher 33: 184-197.
- GschwindYJ, Wolf I, Bridenbaugh SA, KressigRW (2011) Basis for a Swiss perspective on fall prevention in vulnerable older people. Swiss Med Wkly 141: w13305.
- Markle-Reid M, Browne G, Gafni A, Roberts J, Weir R, et al. (2010) A cross-sectional study of the prevalence, correlates, and costs of falls in older home care clients 'at risk' for falling. Can J Aging 29: 119-137.
- Olson SL, Chen SS, Wang CY (2011) Effect of a home exercise program on dynamic balance in elderly with a history of falls. J Aging Phys Act 19: 291-305.
- Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, et al. (2001) Interventions for preventing falls in elderly people. Cochrane Database Syst Rev 4: CD000340.
- McKinley P, Jacobson A, Leroux A, Bednarczyk V, Rossignol M, et al. (2008) Effect of a community-based Argentine tango dance program on functional balance and confidence in older adults. J Aging Phys Act 16: 435-453.
- Chen KM, Tseng WS, Ting LF, Huang GF (2007) Development and evaluation of a yoga exercise programme for older adults. J AdvNurs 57: 432-441.
- Chen KM, Tseng WS (2008) Pilot-testing the effects of a newly-developed silver yoga exercise program for female seniors. J Nurs Res 16: 37-46.
- Roland KP, JakobiJM, Jones GR (2011) Does yoga engender fitness in older adults? A critical review. J Aging Phys Act 19: 62-79.
- Leung DP, Chan CK, Tsang HW, Tsang WW, Jones AY (2011) Tai chi as an intervention to improve balance and reduce falls in older adults: A systematic and meta-analytical review. AlternTher Health Med 17: 40-48.
- Liu H, Frank A (2010) Tai chi as a balance improvement exercise for older adults: a systematic review. J GeriatrPhysTher 33: 103-109.
- Tousignant M, Corriveau H, Roy PM, Desrosiers J, Dubuc N, et al. (2013) Efficacy of supervised tai chi exercises versus conventional physical therapy exercises in fall prevention for frail older adults: A randomized controlled trial. DisabilRehabil 35: 1429-35.
- Wu G1 (2002) Evaluation of the effectiveness of Tai Chi for improving balance and preventing falls in the older population--a review. J Am GeriatrSoc 50: 746-754.
- Dougherty J, Kancel A, Ramar C, Meacham C, Derrington S (2011) The effects of a multi-axis balance board intervention program in an elderly population. Mo Med 108: 128-132.
- Gil-Gomez JA, Llorens R, Alcaniz M, Colomer C (2011) Effectiveness of a wii balance board-based system (ebavir) for balance rehabilitation: A pilot randomized clinical trial in patients with acquired brain injury. J NeuroengRehabil 8: 30.
- Laver K, George S, Ratcliffe J, Quinn S, Whitehead C, et al. (2012) Use of an interactive video gaming program compared with conventional physiotherapy for hospitalised older adults: A feasibility trial. DisabilRehabil 34: 1802-1808.
- Taylor MJ, McCormick D, Shawis T, Impson R, Griffin M (2011) Activity-promoting gaming systems in exercise and rehabilitation. J Rehabil Res Dev 48: 1171-1186.
- Young W, Ferguson S, Brault S, Craig C (2011) Assessing and training standing balance in older adults: a novel approach using the 'Nintendo Wii' Balance Board. Gait Posture 33: 303-305.
- Llorens R, Alcaniz M, Colomer C, Navarro MD (2012) Balance recovery through virtual stepping exercises using kinect skeleton tracking: A follow-up study with chronic stroke patients. Stud Health Technol Inform 181: 108-112.
- Chang YJ, Chen SF, Huang JD (2011) A Kinect-based system for physical rehabilitation: a pilot study for young adults with motor disabilities. Res DevDisabil 32: 2566-2570.
- Lange B, Chang CY, Suma E, Newman B, Rizzo AS, et al. (2011) Development and evaluation of low cost game-based balance rehabilitation tool using the microsoftkinect sensor. ConfProc IEEE Eng Med BiolSoc 2011: 1831-1834.
- Agmon M, Perry CK, Phelan E, Demiris G, Nguyen HQ (2011) A pilot study of Wii Fit exergames to improve balance in older adults. J GeriatrPhysTher 34: 161-167.
- Berg KO, Wood-Dauphinee SL, Williams JI, Maki B (1992) Measuring balance in the elderly: validation of an instrument. Can J Public Health 83 Suppl 2: S7-11.
- Podsiadlo D, Richardson S (1991) The timed "up & go": A test of basic functional mobility for frail elderly persons. J Am GeriatrSoc 39: 142-148.
- Bohannon RW1 (1995) Sit-to-stand test for measuring performance of lower extremity muscles. Percept Mot Skills 80: 163-166.
- Ostchega Y, Harris TB, Hirsch R, Parsons VL, Kington R, et al. (2000) Reliability and prevalence of physical performance examination assessing mobility and balance in older persons in the us: Data from the third national health and nutrition examination survey. J Am GeriatrSoc 48: 1136-1141.
- Powell LE, Myers AM (1995) The Activities-specific Balance Confidence (ABC) Scale. J GerontolABiolSci Med Sci50A: M28-34.
- Demers L, Weiss-Lambrou R, Ska B (2000) Item analysis of the quebec user evaluation of satisfaction with assistive technology (quest). Assist Technol 12: 96-105.
- Demers L, Weiss-Lambrou R, Ska B (1996) Development of the quebec user evaluation of satisfaction with assistive technology (quest). Assist Technol 8: 3-13.
- Lai CH, PengCW, Chen YL, Huang CP, Hsiao YL, et al. (2013) Effects of interactive video-game based system exercise on the balance of the elderly. Gait Posture 37: 511-515.
- Donoghue D, Physiotherapy Research and Older People (PROP) group, Stokes EK (2009) How much change is true change? The minimum detectable change of the Berg Balance Scale in elderly people. J Rehabil Med 41: 343-346.
- Moreno JA, González-Cutre D, MartÃn-Albo J, Cervelló E (2010) Motivation and performance in physical education: an experimental test. J Sports Sci Med 9: 79-85.
- Maclean N, Pound P, Wolfe C, Rudd A (2000) Qualitative analysis of stroke patients' motivation for rehabilitation. BMJ 321: 1051-1054.
- Colombo R, Pisano F, Mazzone A, Delconte C, Micera S, et al. (2007) Design strategies to improve patient motivation during robot-aided rehabilitation. J NeuroengRehabil 4: 3.
- Bischoff HA, StähelinHB, Monsch AU, Iversen MD, Weyh A, et al. (2003) Identifying a cut-off point for normal mobility: a comparison of the timed 'up and go' test in community-dwelling and institutionalised elderly women. Age Ageing 32: 315-320.
- Wang CY, Sheu CF, ProtasEJ (2009) Test-retest reliability and measurement errors of six mobility tests in the community-dwelling elderly. Asian J GerontolGeriatr 4:8-13.
- Goldberg A, Chavis M, Watkins J, Wilson T (2012) The five-times-sit-to-stand test: validity, reliability and detectable change in older females. Aging ClinExp Res 24: 339-344.
- Kim J, Son J, Ko N, Yoon B (2013) Unsupervised virtual reality-based exercise program improves hip muscle strength and balance control in older adults: a pilot study. Arch Phys Med Rehabil 94: 937-943.
- Chui K, Hood E, Klima D (2012) Meaningful Change in Walking Speed Meaningful Change in Walking Speed. Top GeriatrRehabil 28: 97-103.
- Lajoie Y, Gallagher SP (2004) Predicting falls within the elderly community: Comparison of postural sway, reaction time, the berg balance scale and the activities-specific balance confidence (abc) scale for comparing fallers and non-fallers. Arch GerontolGeriatr 38: 11-26.
Citation: Beaulieu-Boire L, Belzile-Lachapelle S, Blanchette A, Desmarais PO, Lamontagne-Montminy L, et al. (2015) Balance Rehabilitation using Xbox Kinect® among an Elderly Population: A Pilot Study. J Nov Physiother 5:261. DOI: 10.4172/2165-7025.1000261
Copyright: © 2015 Beaulieu-Boire L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 19097
- [From(publication date): 4-2015 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 14304
- PDF downloads: 4793